Overview of Vascular Diseases
Vascular diseases are any abnormal conditions that affect the circulatory system and are responsible for more mortality and morbidity than any other category of human disease. The spectrum of pathology encompasses congenital and acquired disorders that are arterial, venous, capillary or lymphatic in origin. Vascular disease can affect virtually any vessel in the body and present with different symptoms in different regions of the body. The most commonly involved areas include the heart, head, neck, and upper and lower extremities. Less commonly, vessels supplying the bowel may be involved leading to bowel infarction.
Table of Contents
Are you more of a visual learner? Check out our online video lectures and start your vascular medicine course now for free!
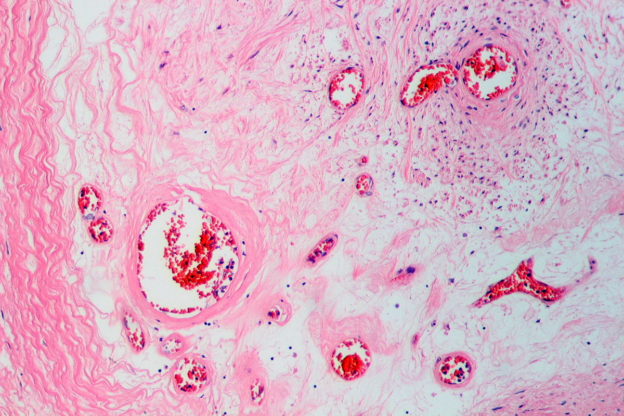
Image: “Occluded artery of the lower leg by an old organized thrombus in peripheral vascular disease.” by Patho – Own work, License: CC BY-SA 3.0
Definition of Terms
- Thrombosis – the formation or presence of a blood clot (thrombus) in a blood vessel
- Stenosis – the narrowing/tightening of the lumen of a blood vessel
- Occlusion – obstruction/blockade of a blood vessel
- Dissection –a tear within the wall of a blood vessel, which allows blood to separate the wall layers
- Necrosis – death of tissue
- Ischemia – reduction/restriction in blood supply
Arterial Diseases
Raynaud’s Syndrome
This refers to peripheral digital ischemia due to vasospasms precipitated by stress or cold. Fingers or toes ache and change color from pale to blue, to red.It may be idiopathic (Raynaud’s Disease/Primary Raynaud Phenomenon), characterized by the occurrence of the vasospasm alone, with no association with another illness. There may be an underlying cause (Secondary Raynaud Phenomenon) usually an autoimmune disease, such as systemic sclerosis (90% of individuals with scleroderma), systemic lupus erythematosus (SLE), rheumatoid arthritis and dermatomyositis/polymyositis.
Buerger’s Disease

Image: “55-year-old female with advanced Buerger’s disease. Two toes amputated due to gangrene. Both legs scheduled for amputation.” by Onthelist – Own work, License: CC BY-SA 4.0
Patients often present with moderate-to-severe claudication that can quickly progress to critical limb ischemia featuring rest pain or tissue loss. Abstinence from tobacco is the only measure known to prevent disease progression.
Carotid artery stenosis
This usually occurs as a result of atherosclerotic disease of the carotid artery, accounting for 20% of strokes and transient ischemic attacks. Symptomatic patients with ipsilateral stenosis >/=70% should have a carotid endarterectomy.Peripheral artery disease
Claudication, which is defined as reproducible ischemic muscle pain, is one of the most common manifestations of peripheral arterial occlusive disease (PAOD) caused by atherosclerosis.Claudication occurs during physical activity and is relieved after a short rest. Ankle-brachial index (ABI) is a useful non-invasive way of establishing the presence of PAOD and is calculated as the ratio of systolic blood pressure at the ankle to that in the arm (normal range, 0.9-1.1; PAOD, <0.9). Angiography is the criterion standard arterial imaging study for the diagnosis of PAOD. Management may be:
- Conservative: regular exercise, tobacco cessation, control of lipid profile, diabetes, and hypertension. Anti-platelets agents have a role (usually aspirin).
- Surgical: open bypass surgery or endovascular therapy (e.g. stents, balloons, or atherectomy devices)
Inflammatory Diseases
An inflammatory disorder of the blood vessel is referred to as a vasculitis. It presents with systemic manifestations (including fever, malaise, myalgias, and arthralgias) and organ dysfunction that depends on the pattern of vascular involvement. It should, therefore, be considered in any unidentified multisystem disorder.Most vasculitis responds to steroid therapy. Vasculitis can result from infections, but, more commonly, has an immunologic basis such as immune complex deposition, anti-neutrophil antibodies (ANCAs), or anti-endothelial cell antibodies. Vasculitis may also be secondary to other diseases such as SLE, rheumatoid arthritis, hepatitis B & C, and HIV.
Different forms of vasculitis tend to specifically affect vessels of a particular caliber and location. They are categorized as follows, depending on the size of the blood vessel affected:
- Large vessel vasculitis: giant cell arteritis and Takayasu arteritis
- Medium vessel vasculitis: Polyarteritis Nodosa and Kawasaki disease.
- Small vessel vasculitis:
- ANCA positive: microscopic polyangiitis, Wegener’s Granulomatosis, Churg-Strauss Syndrome
- ANCA negative: Henoch-Schonlein Purpura, Goodpasture’s Syndrome, cryoglobulinemia
Giant cell arteritis (GCA)
This is also known as cranial or temporal arteritis. It is associated with polymyalgia rheumatic in 50% of individuals. Common signs and symptoms of GCA include visual disturbances, headache, jaw claudication, neck pain, and scalp tenderness.It should always be considered in the differential diagnosis in patients 50 years of age or older with an elevated erythrocyte sedimentation rate. If suspected, steroid therapy (prednisolone) should be started immediately as failure to do so risk irreversible bilateral visual loss. Temporal artery biopsy is the criterion standard for the diagnosis of this granulomatous vasculitis.
Takayasu arteritis
This is also known as aortic arch syndrome or pulseless disease. It is a rare, systemic, inflammatory large-vessel vasculitis of unknown etiology that most commonly affects women of childbearing age (commonly 20-40 years old). It usually affects the aorta and its major branches, causing stenosis and thrombosis. Acute inflammation causes dilatation and aneurysms. Its incidence is higher in Asian countries, such as Japan, and rarer elsewhere.Polyarteritis Nodosa (PAN)
This is a systemic vasculitis characterized by necrotizing inflammatory lesions that affect medium-sized arteries resulting in microaneurysm formation, aneurysmal rupture with hemorrhage, thrombosis, and, consequently, organ ischemia or infarction. Like other vasculitides, PAN is a multi-system disorder with a myriad of manifestations, although it commonly affects the skin, joints, the gut, and the kidneys. PAN may be associated with hepatitis B.Kawasaki disease
This is an acute febrile vasculitic syndrome of early childhood (median age of 10 months), characterized by the inflammation of medium to small-sized arteries causing aneurysms to form. Prognosis is good with treatment (aspirin or intravenous immunoglobulin), although, in a small percentage of patients, it can lead to death resulting from coronary artery aneurysms (CAA). Coronary arteritis can cause aneurysms that rupture or thrombose, resulting in myocardial infarction.Microscopic polyangiitis
This is also known as hypersensitivity vasculitis or leukocytoclastic vasculitis. It is a necrotizing vasculitis affecting small-sized vessels. Necrotizing glomerulonephritis (seen in 90% of patients) and pulmonary capillaritis are particularly common.Wegener’s granulomatosis

Image: “Wegener’s granulomatosis” by Yale Rosen from USA, uploaded by CFCF, License: CC BY-SA 2.0
- Granulomas of the lung and/or upper respiratory tract (ear, nose, sinuses and throat).
- Vasculitis of small to medium-sized vessels, most prominently in the lungs and upper respiratory tract
- Glomerulonephritis
Churg-Strauss Syndrome
This is also known as allergic granulomatosis and angiitis. It is a small vessel vasculitis classically associated with asthma, eosinophilia, and granulomas.Henoch-Schonlein Purpura (HSP)
This is a systemic variant of IgA nephropathy (Berger’s Disease), causing a small vessel vasculitis. It usually presents with a purpuric rash on extensor surfaces (typically on the legs) and glomerulonephritis. Diagnosis is usually clinical, but can be confirmed with positive immunofluorescence for IgA and C3 in skin or renal biopsy.Goodpasture’s Syndrome
This is also known as anti-glomerular basement membrane (GBM) disease, and, as the name suggests, it is caused by the development of autoantibodies to type IV collagen, an essential component of the GBM. This autoimmune disorder is characterized by autoantibodies directed against the glomerular and the alveolar basement membrane, hence patients present clinically with manifestations of both pulmonary and renal disease, which may include hemoptysis and hematuria.Cryoglobulinaemia
This is characterized by the presence of cryoglobulins in the serum. This may result in a clinical syndrome of systemic inflammation (most commonly affecting the kidneys and skin) caused by cryoglobulin-containing immune complexes. It may be associated with hepatitis C.Diseases of the Aorta
Aortic dissection

Image: “CT reconstruction of aortic dissection” by Dr. Lars Grenacher (www.grenacher.de), uploaded by J. Heuser – scan courtesy of Dr. Lars Grenacher (www.grenacher.de), License: CC BY-SA 3.0
Aortic dissections occur mainly in two age groups: (1) men aged 40 to 60 years with antecedent hypertension (more than 90% of cases); and (2) younger patients with connective tissue abnormalities that affect the aorta (e.g. Marfan Syndrome). Dissections can also be iatrogenic (e.g. complicating arterial cannulation), and rarely, for unknown reasons, may occur in pregnant women. Aortic dissections are generally classified into two types:
- Proximal lesions: type A dissections, involving the ascending aorta, with or without involvement of the descending aorta (DeBakey type I or II, respectively)
- Distal lesions: type B dissections, usually beginning beyond the subclavian artery (DeBakey type III).
Aneurysms
Aortic aneurysms are congenital or acquired dilatations of the heart or blood vessels. Aneurysms of the aorta are fusiform, which are circumferential dilations that can be up to 20 cm in diameter.The two most important causes of aortic aneurysms are atherosclerosis and hypertension. Other conditions that weaken vessel walls and lead to aneurysms include trauma, vasculitis, congenital defects, and infections (the so-called mycotic aneurysms). Complications are related to rupture, thrombosis, and embolization.
Renal artery stenosis
This is the major cause of renovascular hypertension. The patient presents with refractory hypertension (i.e. poor control of hypertension, despite treatment with three or more antihypertensive agents). It tends to occur in older individuals, with atherosclerosis being, by far, the most common etiology of renal artery stenosis.Venous Diseases
Pulmonary embolism
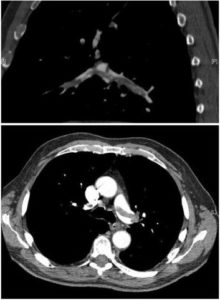
Image: “CT pulmonary angiography images confirming the presence of a saddle embolus and substantial thrombus burden in the lobar branches of both main pulmonary arteries.” by Aung Myat and Arif Ahsan – Percutaneous mechanical thrombectomy for the treatment of acute massive pulmonary embolism: case report. Thrombosis Journal 2007, 5:20. doi:10.1186/1477-9560-5-20, License: CC BY 2.0
The classic presentation of pulmonary embolism is an abrupt onset of pleuritic chest pain, shortness of breath and hypoxia.
Risk factors include recent surgery (especially abdominal/pelvic or hip/knee replacement), thrombophilia (e.g. antiphospholipid syndrome), leg fracture, prolonged bed rest/reduced mobility, malignancy, pregnancy/postpartum, hormone replacement therapy, and a previous pulmonary embolism. Management of this involves anticoagulation (e.g. using low-molecular-weight heparin) and thrombolysis (e.g. alteplase).
Deep venous thrombosis (DVT)
DVT is a manifestation of venous thromboembolism (DVT). Although most DVT is occult and resolves spontaneously without complication, lots of deaths result from DVT-associated massive pulmonary embolism (PE).Risk factors include recent surgery (especially abdominal/pelvic or hip/knee replacement), trauma, thrombophilia (e.g. antiphospholipid syndrome), leg fracture, prolonged bed rest/reduced mobility, malignancy, pregnancy, obesity, hormone replacement therapy/synthetic estrogen, or a previous DVT.
Diagnosis is based on validated clinical prediction rules (e.g. the Wells score) and D-dimer testing (which is sensitive, but not specific for DVT as it is also increased in infections, pregnancy, malignancy, and post-op). A negative D-dimer result, combined with a low pretest clinical probability score is sufficient to exclude DVT. Anticoagulation is the mainstay of therapy. Inferior vena caval filters may be used in active bleeding, or when anticoagulation fails, to minimize the risk of thromboembolism.
Varicose veins
This refers to the long tortuous and dilated veins of the superficial venous system. The superficial veins of the upper and lower leg typically are involved, and the causes include:- Primary causes (95%): unknown, congenital valve absence (very rare)
- Secondary causes (5%): obstruction: DVT, fetus, ovarian tumor; valve destruction: DVT; arteriovenous malformation, constipation, overactive muscle pumps (e.g. cyclists)
Varicosities (venous dilations) of other sites worth mentioning include esophageal varices which occur is secondary to portal hypertension. They are important as they are prone to ruptures that can lead to massive (even fatal) upper gastrointestinal hemorrhage.
Congenital Malformations
Hemangioma

Image: “Small hemangioma on the scalp of a two-year-old female.” by Cbheumircanl – Own work, License: Public Domain
Although these localized lesions are typically confined to the head and neck, they occasionally may be more extensive (angiomatosis) and can arise internally, with most of these internal lesions being found in the liver. Malignant transformation is rare. Histological/clinical variants include:
- Capillary hemangiomas: commonest; occur in the skin, subcutaneous tissues, and mucous membranes of the oral cavities and lips, as well as in the liver, spleen, and kidneys.
- Juvenile hemangiomas: (so-called strawberry hemangiomas) of the newborn skin.
- Pyogenic granulomas
Cavernoma (cavernous hemangioma)
These are composed of large, dilated vascular channels. Compared to other hemangiomas, cavernous hemangiomas are more infiltrative, frequently involve deeper structures and do not spontaneously regress. Of note, cavernous hemangiomas constitute one component of von Hippel-Lindau disease, in which vascular lesions are commonly found in the cerebellum, brain stem, retina, pancreas, and liver.Malformations of the aorta
Congenital malformations of the aorta include aortic valvular stenosis or complete-aortic valvular atresia, coarctation of the aorta, double aortic arch, right aortic arch, and an interrupted aortic arch.Worth mentioning is the coarctation of the aorta with an estimated incidence of 3.2/10,000 births. In this malformation, the aortic lumen below the origin of the left subclavian artery is significantly narrowed. It is distinguished into two types based on the level of constriction in relation to the entrance of the ductus arteriosus as preductal and postductal.
Diseases of the Lymphatic System
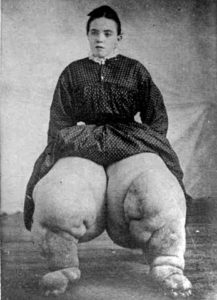
Elephantiasis
This refers to leg lymphedema resulting from lymphatic filariasis. The most frequent organisms causing this disease are Wuchereria bancrofti and Brugia malayi. These filarial worms block the flow of lymph, causing edematous arms, legs, and scrotum. The disease is transmitted by the bite of the infected Anopheles and Culex mosquitoes. Filariasis is diagnosed by detection of microfilariae in blood. It is treated with a combination of diethylcarbamazine and albendazole.Cysts (cavernous lymphangiomas/cystic hygromas)
These benign lesions are composed of massively dilated lymphatic spaces lined by endothelial cells and are typically found in the neck or axilla of children. They can be very large, filling the axilla or producing gross deformities of the neck. Cavernous lymphangiomas of the neck are common in Turner Syndrome.Review Questions
The correct answers can be found below the references.1. A 23-year-old man presents with fever, weight loss, malaise, abdominal pain and myalgias. Workup reveals that the patient has Polyarteritis Nodosa. Which of the following is associated with this form of vasculitis?
- Arsenic
- Chlamydia pneumonia
- Hepatitis B virus
- Human herpes-virus 8
- Human immunodeficiency virus
- Aneurysms of the abdominal aorta
- Aneurysms of the coronary arteries
- Dissection of the thoracic aorta
- Ischemia and gangrene of the extremities
- Rupture of a berry aneurysm.
- Ethnicity
- Obesity
- Renal artery stenosis
- Smoking
- Stress

Comentários
Enviar um comentário