Acute Back Pain — Clinical Features and Differential Diagnosis
Table of Contents
Introduction
The upright posture of a human being has its downside and back pain is a very frequent phenomenon among humans as a result of their posture. According to a study, more than 80 % of people had experienced some form of back pain in their lifetime.
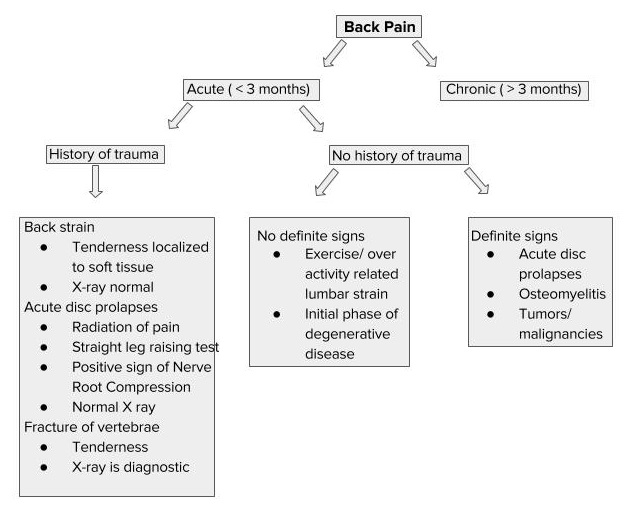
Acute back pain lasts for a few days to 3 months but, when it lasts for more than 3 months, it can be called chronic back pain. Most of the acute back pain is due to musculoligamentous injury and subsides without any intervention in 2 to 4 weeks. In about half of the cases, acute back pain may recur.
Epidemiology of Acute Back Pain
Age
Acute back pain is common in adults. The first episode of acute back pain often occurs between 20 and 40 years of age. It is mostly related to trauma or abnormal posture and may be the first reason to seek medical care as an adult. It is rare in children unless there is a congenital defect precipitating the backache. In the elderly population, back pain is often chronic and due to degenerative or metabolic causes.
Sex
Acute back pain is common in women. Several factors, for instance, multiple pregnancies, hormonal changes after menopause, poor nutrition, and obesity increase the risk of back pain in the female population.
Occupation
Certain occupations, for instance, heavy lifters, miners and truck drivers have an increased prevalence of a backache due to repetitive mechanical strain to the back.
Differential Diagnosis of Acute Back Pain
Acute back pain has wide differential diagnoses, ranging from benign self-limiting conditions to the life-threatening ones. The pain can be of any type—dull, severe, throbbing, or pricking. It can be mild, moderate to severe and debilitating. Depending on the origin, back pain can be classified into different types:
Approach to a Patient with Acute Back Pain
Clinical Features of Acute Back Pain
A detailed history and physical examination are essential for evaluating the cause of acute back pain. A history of recent trauma or heavy weight lifting is important.
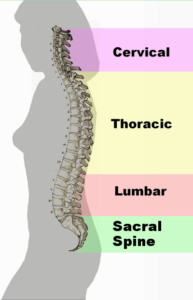
Image: “Spinal column curvature” by
http://en.wikipedia.org/wiki/user:Vsion – Originally Vsion’s work. License: CC0
The site of pain varies according to the cause or location of the lesion. It may be anywhere from upper to lower back. For instance, cervical disc prolapse causes pain in the upper back and neck, while lumbar disc prolapse causes pain in the lower back. Sometimes, pain is referred to arms and legs, which is mostly due to nerve root compression.
Acute back pain is of short duration. Sometimes, chronic back pain is superimposed by an acute aggravation of the pain, e.g., the degenerative conditions, osteoporosis, and osteomyelitis pain are insidious in onset, but aggravated by sudden movements or over activities.
The knowledge of aggravating and relieving factors is important. Musculoligamentous pain typically increases with activity and relieves with rest. Some conditions like seronegative spondyloarthritis and ankylosing spondylitis cause pain that characteristically gets worse after rest and relieves during activity. Severe back pain at night that responds to aspirin may indicate a benign tumor. Back pain related to menstruation is of gynecological etiology.
Associated symptoms
Stiffness
Stiffness is a prominent feature of inflammatory arthritis, e.g., rheumatoid arthritis and ankylosing spondylitis.
Pain in other joints
The rheumatic diseases present with pain in multiple joints in addition to back pain. Rheumatoid arthritis involves the small joint of hands bilaterally.
Neurological symptoms
Paraesthesia, numbness, tingling sensation or weakness are associated features of nerve root compression, often by a disc prolapse.
Physical examination
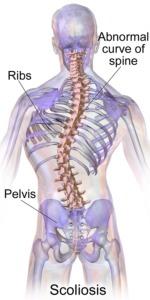
Image: “Scoliosis” by
Blausen.com staff (2014). “Medical gallery of Blausen Medical 2014”. WikiJournal of Medicine. License: CC BY 3.0
Look for an abnormal standing posture, for instance, scoliosis(sidewise bending of the vertebral column), kyphosis (forward bending of the vertebral column), lordosis (backward bending of the vertebral column), forward flexion of the torso on the lower limbs, and pelvic tilt.
Look for tenderness, swelling, and range of movements. Tenderness is present in fractures, inflammatory, and infective conditions. Vertebral tuberculosis (Pott’s disease) present as a cold abscess or a swelling.
Abdominal, rectal or per vaginal examination may be performed wherever necessary to exclude the gynecological or abdominal conditions presenting as a back pain.
The straight leg raising test is performed to detect nerve root compression. Peripheral pulses should be palpated to exclude vascular causes of back pain. Vascular claudication may present as acute back pain.
Image: “The picture shown is a straight leg test that is sometimes used to help diagnose a herniated lumbar disc.” by
Davidjr74. License: CC0
Investigations for Acute Back Pain
Most cases of acute back pain are self-limiting and do not require investigation unless certain red flag signs are present. The red flag signs are given in the following table:
Red Flags for Back Pain
- Age > 50 years
- No improvement after 4 weeks of treatment
- Unexplained weight loss
- Pain worse at night
- Previous history of cancer
- Progressive neurological deficits
- Bladder or bowel dysfunction
- Prolonged use of corticosteroids
- Fever
- Anemia
- Elevated ESR, CRP
Laboratory investigations
Complete blood count, erythrocyte sedimentation rate, and C-reactive protein levels are beneficial if there is a suspicion of infection or a neoplasm.
Vitamin D, serum calcium, and parathyroid hormone levels are advised in elderly patients with degenerative and metabolic conditions. Rheumatoid factor and anti-CCP are indicated for rheumatoid arthritis.
Radiological examination
Treatment of Acute Back Pain
- If there are no red flag signs, the patients should be reassured and educated.
- Most of the cases of non-specific acute back pain resolve within 2 to 4 weeks.
- Mild analgesics and muscle relaxants should be prescribed.
- Spinal exercises, rest, traction, hot packs, and corset are also helpful in the management of acute back pain.
- Resume normal activities as soon as possible.
- If red flag signs are present, the patient should be properly investigated and referred to a specialist.
- If a specific disease is diagnosed by different diagnostic modalities, it should be managed accordingly.

Nice Blog…
ResponderEliminarThanks for sharing this with us.
If you have Back Pain problem and you want the best medication to cure your problem at an affordable price then you can contact Dr. Rajinder Singh at Kalyan Hospital in Ludhiana.