Development of the Gastrointestinal Tract and the Bronchial System
Table of Contents
Development of the Gastrointestinal Tract
Embryonic Origin of the Gastrointestinal Tract
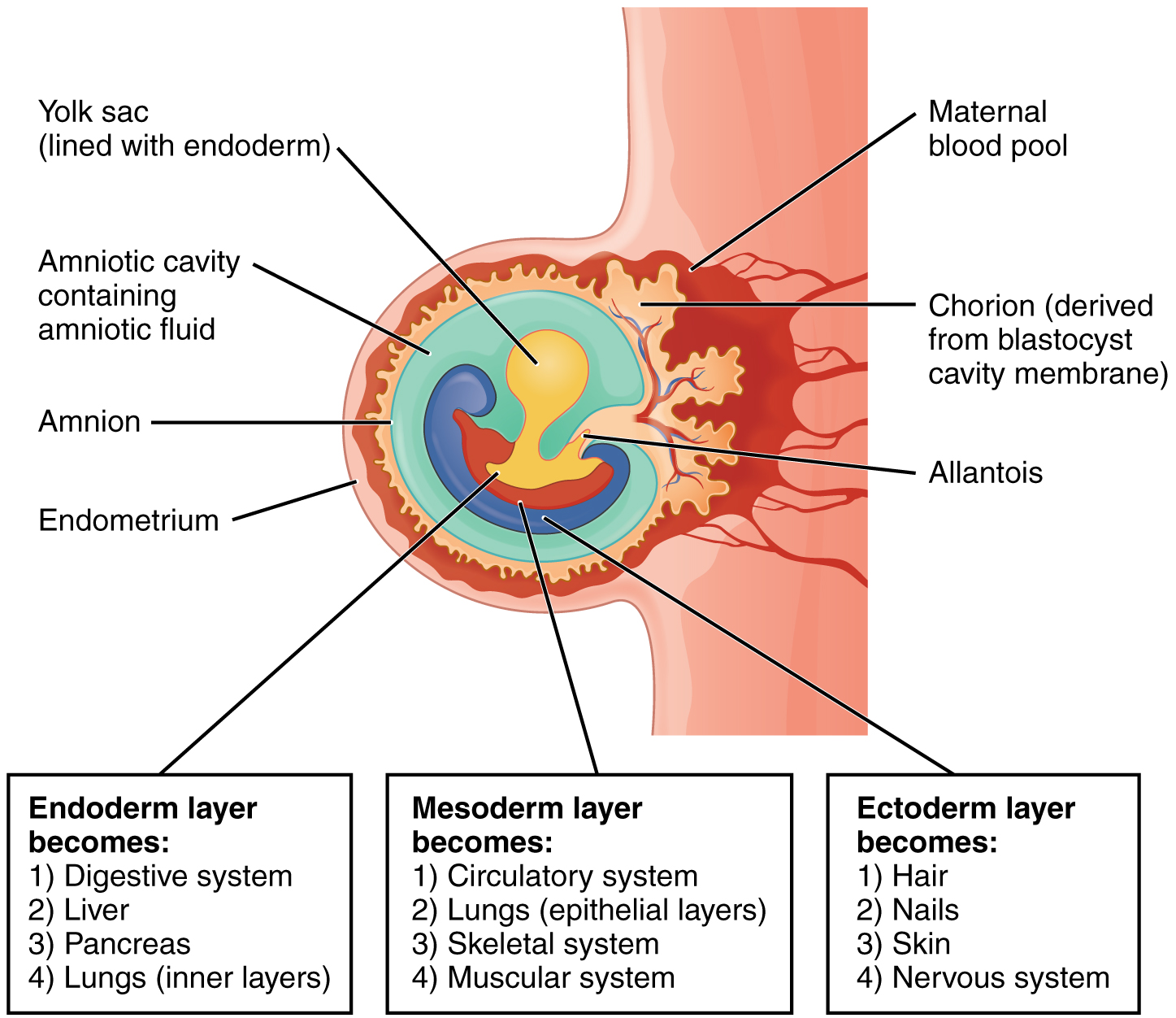
Organ development is preceded by the formation of the three germ layers: endoderm, mesoderm, and ectoderm. During the process of gastrulation and the formation of the embryo, cavities emerge, which give rise to all internal organs.
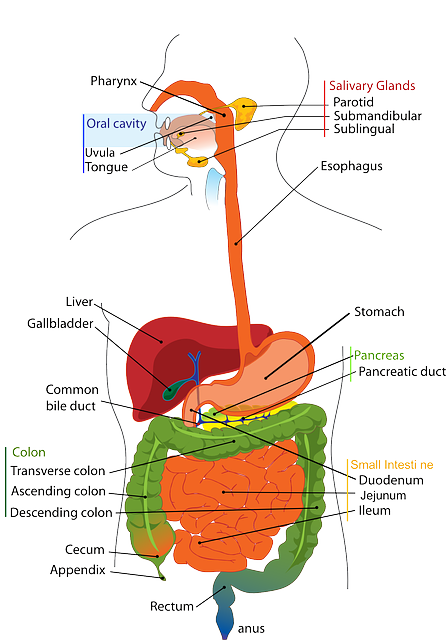
Approximately, on the 23rd day of development, the folding of the embryonic disc takes place, separating part of the yolk sac. At the time of the formation of the embryo, the endoderm gives rise to the primitive gut tube – the origin of the entire gastrointestinal tract, as well as further organs, such as the liver and lungs. The gut tube is incorporated into the growing embryo, which means that the gut can develop within the emerging peritoneal cavity. The gut tube is folded into a blind-ended tube. Its cranial end terminates blindly at the oropharyngeal membrane (membrana buccopharyngea) and its caudal end terminates blindly at the cloacal membrane. The gut tube can be divided into four sections:
- Pharyngeal gut: Oral– & nasal cavities and associated structures, pharyngeal pouches.
- Foregut: Pharynx, esophagus, stomach, duodenum, as well as lung, trachea, bronchi, liver,pancreas.
- Midgut: Duodenum, jejunum, ileum, descending and transverse colon, as well as Brunner’s glands, Peyer’s patches and vermiform appendix.
- Hindgut: Transverse colon and descending colon, rectum as well as allantois (embryonic bladder) and urogenital sinus.
Development of the Peritoneal Cavity and Mesentery
Body cavities, or coeloms, are “spaces” within the embryo lined with serous membrane (or serosa). The emergence of a really big space is pathological and might occur, for example, through an influx of air or blood. In the physiological state, the parietal serosa, deriving from the mesoderm of the body wall, and the visceral serosa from the mesoderm of the organ wall, are closely associated with each other. The parietal serosa lines the abdominal wall; the visceral serosa covers the intestinal wall.
Pericardioperitoneal canals (coelomic openings) extend along the intestinal tube and connect the pericardial with the peritoneal cavity. The lateral folding of the embryo results in the growth of pleuropericardial folds on both sides of the intestinal tube; flaps, which converge anteriorly and posteriorly with the intestinal tube and dorsally, only a narrow fold of tissue remains. This connection between the eventual intestine and abdominal cavity is called the mesentery. Mesenteries are covered with visceral serosa, connect organs to each other or to the abdominal wall, and conduct associated nerves and blood vessels.
A distinction is made between ventral and dorsal mesentery. The ventral mesentery develops in the upper abdomen and connects the stomach and upper duodenum with the anterior abdominal wall and liver. It later contains the portal vein, hepatic artery and common bile duct. The dorsal mesentery extends along the entire intestine and contains the three major arteries of the intestine, namely the celiac artery supplying the foregut, the superior mesenteric artery supplying the midgut and the inferior mesenteric artery supplying the hindgut.
The dorsal mesentery associated with the ascending and descending colon coalesces later with the posterior abdominal wall and then becomes retroperitoneal. This gives rise to the root of the mesentery (radix mesenterii), which attaches the small intestine to the dorsal body wall. It extends from the upper left corner of the junction between duodenum and jejunum (duodenojejunal flexure) to the bottom right junction between ileum and colon (ileocecal junction). At the transverse colon, the root of transverse mesocolon (radix mesocoli transversi) and, attached to the sigmoid colon, the mesosigmoid fold arises.
Organs of the Upper Abdomen
Below the already formed diaphragm, the intestinal tube expands into a spindle-shaped stomach. The rotation of the stomach of 90 degrees is caused by an accelerated growth of the left side. The greater curvature of the stomach is now left, the lesser curvature right. The rotation of the stomach causes the duodenum, which is attached to the stomach, to subsequently rotate and shift dorsally.
Considering the location of the stomach within the embryo, a descent can be noted. On day 32, the stomach is level with the 7th cervical vertebra; on day 50, it reaches its final position between the 11th thoracic and the 3rd lumbar vertebra. During the process, the stomach is shifted towards the left and the pylorus is brought into a horizontal position. Thus, on the right side, a space for the developing liver and pancreas, as a budding from the duodenum, has been created.
Development of the Pancreas
From day 26 and on day 28, two pancreatic buds develop, which eventually fuse to form the exocrine pancreas. It is only based on the later duct system that these two primordial (dorsal and ventral) portions can still be distinguished. In week 9, the endocrine parts of the pancreas(islets of Langerhans) arise from the endocrine cells of the pancreatic epithelium. The pancreatic islets already synthesize hormones during the fetal period, in particular, the growth-enhancing insulin, whereas the exocrine pancreas becomes functionally active only after birth.
Development of the Liver
Also, the liver starts to develop from the 25th/26th day. It is the most important hematopoietic organ of the embryo and fetus. Gland-like epithelial liver cords and the excretory duct system (later referred to as the biliary system) arise from another epithelial bud (liver bud or hepatic diverticulum). Hematopoietic stem cells are embedded in the fast growing mesenchymal tissue located between the epithelial liver cords.
In the second half of pregnancy, hematopoiesis is downregulated and the development of hepatocytes is facilitated. Epithelial liver cords develop gradually into the typical hepatic lobules. The liver reaches its full and versatile metabolic capacity only after birth, when the intestine is also fully developed. Prenatally, the liver is responsible for the degradation of fetal hemoglobin, causing the dark coloring of the meconium – the first bowel movement of the neonate.
Organs of the Lower Abdomen
In the lower abdomen, the midgut gives rise to the small and large intestine. To understand how both reach their final position within the abdominal cavity, one has to consider the rotation of the umbilical loop.
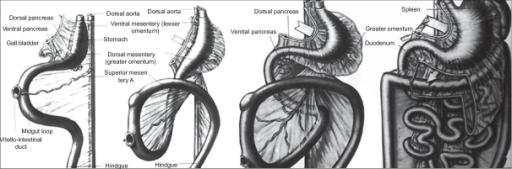
On about the 32nd day, the midgut forms the umbilical loop, which is supplied by the superior mesenteric artery in the dorsal mesentery. This artery now serves as the axis of rotation. The small intestine located cranial to the loop grows faster than the caudally located large intestine. The small intestine initially extends into the umbilical coelom, and, at a later stage, once the abdominal cavity is large enough, shifts inwards again. This is referred to as physiologic herniation.
Following a rotation of 270 degrees counter-clockwise of the midgut loop around the superior mesenteric artery, the large intestine is positioned above the small intestine and reaches its final position below the liver (transverse colon). From there, as a result of further growth, the ascending colon arises from the midgut and the descending colon from the hindgut.
Furthermore, the hindgut gives rise to the sigmoid colon. The rectum, the upper part of the anal canal and part of the genitourinary system arise from the so-called cloaca. The lower part of the anal canal is ectodermal (not endodermal) in origin, thus the junction between the two is not visible externally, but can be observed internally.
Functional Development of the Intestine
The formation of characteristic histological structures (villi, intestinal crypts, etc.) occurs during the first weeks of life. During the embryonic period, ingestion of food via the gut is not yet possible. However, for the gut to be able to function after birth, the blind ends of the intestinal tube have to open up. The oropharyngeal membrane opens up during the fourth week, the anal membrane during the sixth week.
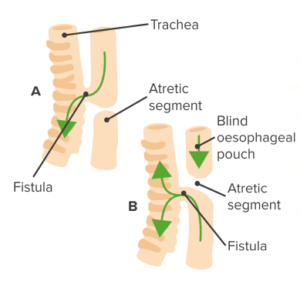
Tracheo-esophageal Fistula
-
Most common: 1:3000—4500 live births
- Polyhydramnios (excess amniotic fluid)
- Chokes on feeding
- Milk dribbles from mouth
- Not initially cyanotic but may develop pneumonia
- Abdomen distends as stomach fills with air
- Sometimes termed a H-type tracheo-esophageal fistula
- Approximately 4 % of all cases
- Milk my be “driven” into respiratory system
Development of the Bronchial System
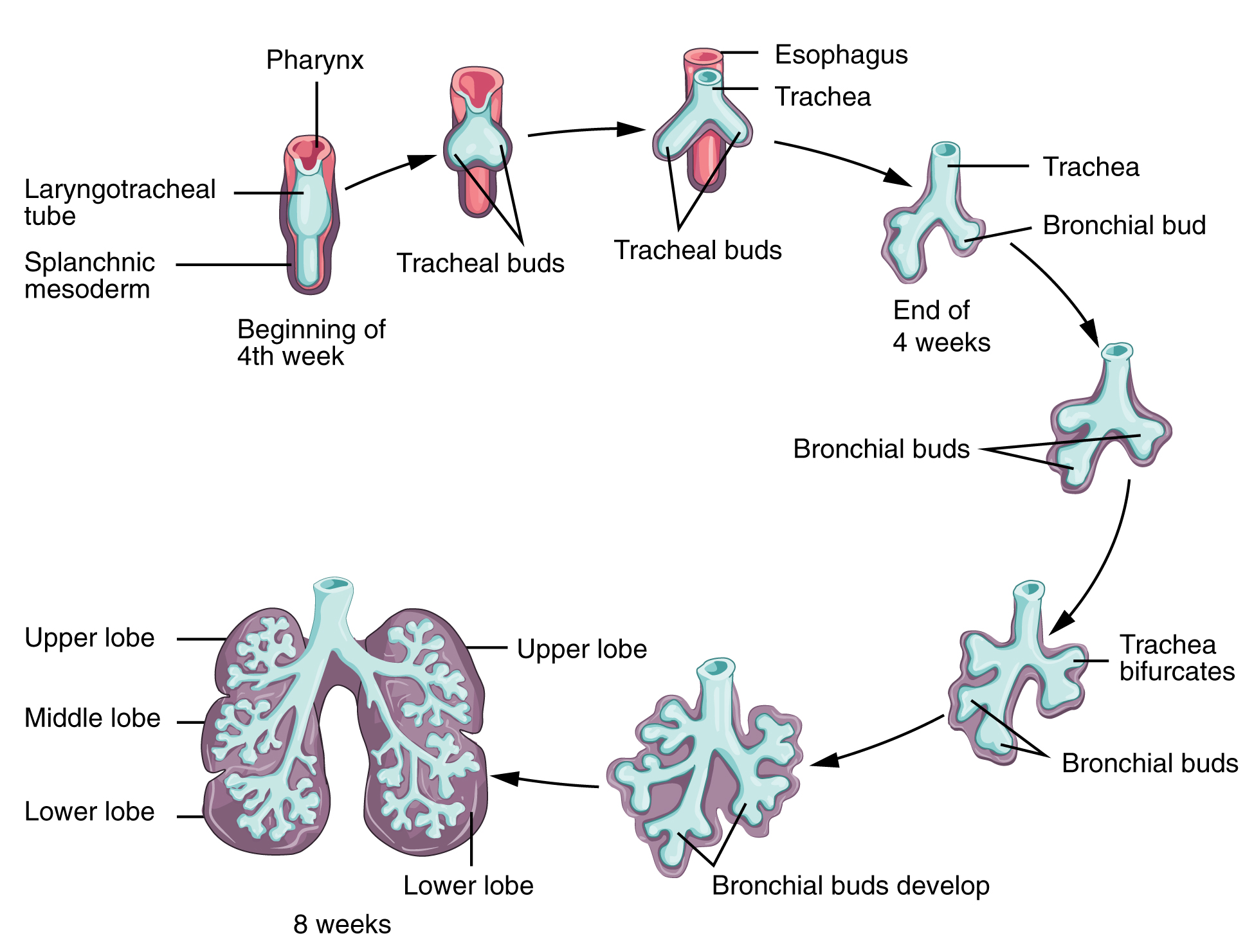
Although the lung is not needed before birth, its complex development begins during the embryonic stage. The lung emerges as the budding of a part of the embryonic gut tube and, therefore, from an evolutionary point of view, belongs to the endoderm. In the following section, the stages of lung development are presented concisely in 5 developmental stages:
Stage 1: Early Stage of Lung Development
The lower respiratory organs arise from the laryngotracheal groove. This median longitudinal epithelial groove begins to form during the fourth week at the bottom end of the pharyngeal gut. The epithelial layer, the glands of the endodermal respiratory tract and the alveolar epithelium of the lung arise from the endodermal epithelium of the laryngotracheal groove. Mesenchymal cells give rise to musculature, cartilage, and other connective tissue of the lung.
The laryngotracheal groove gives rise to the lung or respiratory bud (respiratory diverticulum), which expands into the pericardioperitoneal canals that later form the pleural cavity and are derived from the pericardial cavity. The medial serous membrane of the canal forms the visceral pleura, the lateral serous membrane the parietal pleura.
The lung bud divides into two primary bronchial buds, later corresponding to the left and the right lung. At this stage, the right bronchial bud is already bigger and facing caudal – as is later the right lung lobe stronger than the left lung lobe. Gradually, as a result of uneven, dichotomous divisions, the main bronchi, lobar bronchi and segmental bronchi develop.
By the end of the 5th week, the necessary cavities for directing the air have been developed. Now, the anatomical and histological structures develop, which allow the exchange of gas between air and blood.
Stage 2: Pseudoglandular Phase of Lung Development
From the 6th – 16th week, the lobules (acini) and terminal bronchioles, which form the bronchial tree of the lungs, develop. The lobules are structurally similar to a gland, which is why this stage is referred to as pseudoglandular. At this stage, the blood-air barrier has not yet been formed; the fetus would not be viable at birth.
Stage 3: Canalicular Phase of Lung Development
In the 16th – 26th week, the respiratory part of the lung, the respiratory bronchioles, form. From here, the canaliculi or tubules branch, which are later referred to as alveolar ducts. Simultaneously, a vascularization of the surrounding mesenchymal tissue takes place. At the end of the canaliculi, first primitive alveolar sacculi develop. This development continues into the next stage.
Stage 4: Saccular Phase of Lung Development
From the 26th week until birth, more and more terminal saccules are formed. Their epithelium is initially cubic, and then differentiates into thin squamous epithelium and ultimately into the typical thin type I pneumocytes. In addition to type I pneumocytes, sporadically type II pneumocytes are formed, which are responsible for the secretion of surfactant. Surfactant reduces the surface tension of the alveoli and prevents the lung from collapsing. Sufficient production of surfactant, however, is achieved only shortly before birth. It is vital and a lack of it often creates a problem for premature babies. At the same time, the capillary network grows quickly and forms dense networks around the terminal saccules, as a result of which the blood-air barrier develops.
Stage 5: Alveolar Phase of Lung Development
From the 32nd week, the epithelium of the alveolar sacs thins further. Now, the capillaries push into ductus and sacculi, while the primitive alveoli bulge into the connective tissue. They form the functional respiratory membrane, but they only turn into mature alveoli once they have been exposed to air. The lung continues to develop after birth. Whilst there are 50 million alveoli at birth, the immature alveoli multiply during the first 8 years of life to about 300 million mature alveoli.
Pulmonary Function during and after Pregnancy
Respiration is not required intrauterine, yet the lung fulfills an important task. It produces part of the amniotic fluid. Every day, about 15 ml of amniotic fluid per kilogram of body weight is generated within the embryo. From birth, a healthy lung is responsible for oxygen supply; its maximum capacity is reached during the first few years of life.
Review Questions
Solutions can be found below the references.
1. The endoderm does not give rise to…
- …the lower part of the descending colon.
- …the alveoli of the lungs.
- …the exocrine pancreas.
- …the hyaline cartilage of the bronchi.
2. At what stage of lung development are pneumocytes being produced?
- Canalicular phase,
- Pseudoglandular phase,
- Saccular phase,
- Alveolar phase,
3. The dorsal mesentery does not include…
- …celiac trunk.
- …superior mesenteric artery.
- …inferior mesenteric artery.
- …hepatic artery.

Comentários
Enviar um comentário