Psychiatric Disorders in Pregnancy: Baby Blues, Postpartum Depression and Postpartum Psychosis
Table of Contents
- Definition of Psychiatric Disorders in Pregnancy
- Etiology and Pathophysiology of Psychiatric Disorders in Pregnancy
- Symptoms and Signs of Psychiatric Disorders in Pregnancy
- Tests and Investigations for Psychiatric Disorders in Pregnancy
- Pathology of Psychiatric Disorders in Pregnancy
- Treatment of Psychiatric Disorders in Pregnancy
- Complications and Prognosis of Psychiatric Disorders in Pregnancy
- Prevention of Psychiatric Disorders in Pregnancy
- Prognosis
- Review Questions
- References
Image: “Sorrow [section]” by Vincent van Gogh. License: Public Domain
Definition of Psychiatric Disorders in Pregnancy
Postpartum depression or the baby blues affects the vast majority of women after giving birth. This state is characterized bya low mood and irritability starting shortly after birth and lasting for up to two weeks. 40 to 80% newmothers suffer from this after child birth.The symptoms are mild and do not interfere with the activities of daily living or with the care of the infant
These are triggered due to physical changes occur in the body after child birth, hormones levels drop immediately, breast changes due production of milk by lactiferous tubules, due to exhausted body, emotions are another factor because of anxiousness to adjust to new routine, new responsibilities.
Postpartum depression involves having a low mood, irritability, sleep disturbances, and guilty feelings that occur after the delivery of an infant that last at least two weeks and interfere with activities of daily living and the ability of the woman to care for herself and her infant.
Postpartum psychosis is much rarer than the baby blues and postpartum depression. It involves the onset, usually within two weeks after delivery, of hallucinations, irritability, unusual thought patterns, mood swings and difficulty sleeping that last for at least two weeks.
Epidemiology
The baby blues, postpartum psychosis, and postpartum depression occur in all ages of women, in all parts of the world, and in all ethnicities. The incidence of the baby blues is about 80% of all women. Women who have had difficulties with the pregnancy or the birth, and women who are prone to low mood, have an increased likelihood of developing the baby blues.
About 10 to 20% of women will have postpartum depression. Women who were depressed in pregnancy, have high stress levels, upheavals in life events, low incomes, decreased social support, the absence of a job, rigid parental beliefs, anxiety disorders, past history of mental illness, and being a minority are all things that increase the chance of developing postpartum depression.
Postpartum psychosis occurs in 1 – 2 out of every one thousand pregnancies. Women at the greatest risk for this disorder are those with previous psychiatric illnesses, or those who suffered from psychosis during pregnancy. The disorder usually begins within two weeks after giving birth.
Etiology and Pathophysiology of Psychiatric Disorders in Pregnancy
There are some studies that have evaluated the etiology of the baby blues, postpartum depression and postpartum psychosis. It is believed that both internal and external factors play a role in the development of postpartum psychiatric disorders. Abrupt decreases in progesterone and estrogen occur after pregnancy, which is believed to trigger emotional changes in susceptible women.
Risk Factors
Women who have little social support, have a low socioeconomic status, a complicated birth, an unwanted gender of baby, are not working, have a history of mental illness, or had an anxiety, depressive, or psychotic disorder during pregnancy are at a greater risk of developing the disorder.
Pathophysiology
The pathophysiology of psychiatric disorders has been studied. There is little data on the pathophysiology of the baby blues, but some researchers have discovered that the sudden decline in estrogen and progesterone that occurs shortly after birth can trigger emotional symptoms in susceptible women. Even women without a past history of mental illness or pregnancy complications can suffer from the baby blues.
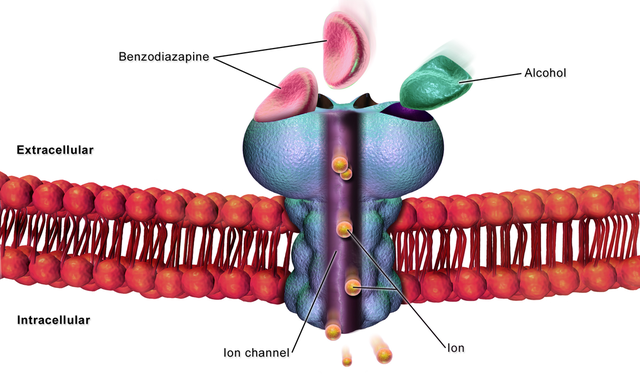
Postpartum depression has been extensively studied as to pathophysiology. Environmental and biological factors have been implicated. Some researchers have found that sudden decreases in estrogen levels will trigger mood changes that can be diagnosed as postpartum depression. Others suggest that difficulties in regulating the gamma-aminobutyric acid (GABA) receptor play a role in developing the disorder.
There is strong evidence that environmental influences have an impact on the pathophysiology of postpartum depression. Patients with depression during pregnancy, a difficult pregnancy, a history of any type of mental illness, a difficult childbirth, poor social support, low income and psychosocial stressors have a high incidence of developing postpartum depression, even in the absence of any biological or genetic factors.
The evidence for a genetic origin for postpartum psychosis is much stronger than for the baby blues and postpartum psychosis. Postpartum psychosis seems to run in families, although no specific gene or set of genes has been identified as being associated with postpartum psychosis.
Having a history of bipolar disorder prior to or during pregnancy contributes to the pathophysiology of postpartum psychosis. Women with psychosis during pregnancy have a greater incidence of postpartum psychosis.
Symptoms and Signs of Psychiatric Disorders in Pregnancy
The baby blues can develop shortly after pregnancy as the hormone fluctuations happen immediately after delivery. The main symptoms include the following:
- Rapid changes in mood
- Anxiousness
- Periods of sadness and irritability
- Feelings of being overwhelmed about mothering
- Episodes of crying
- Poor concentration
- Difficulty with eating too much or too little
- Insomnia or frequent awakenings at night
These symptoms last for only about one to two weeks after delivery.
The main symptoms of postpartum depression include the following:
- Low mood
- Periods of sadness
- Frequent episodes of crying
- Feeling insecure about being able to care for the infant
- Anxious symptoms related to caring for the infant
- Insomnia or frequent awakenings at night
- Eating too much or too little
- Having decreased ability to concentrate
- Having periods of confusion
- Being irritable
- Feeling isolated from others
- Feeling unwanted or worthless
- Feeling sensations of shame
- Feeling guilty about parenting skills
- Having increased anger outbursts
- Being unable to care for the infant because of symptoms
- Losing the ability to care for oneself because of symptoms
- A sense of isolation
- A feeling of worthlessness
- Sensations of shame
- Feelings of guilt, particularly around parenting
- Increased anger
- Having an inability to care for herself and her family
- Feeling suicidal or having frequent thoughts of death
These symptoms can occur at any time within the first year of childbirth and must last at least two weeks in order to have the diagnosis of postpartum depression.
Symptoms of postpartum psychosis include the following:
- Periods of paranoia
- Episodes of confusion
- Feelings of disorientation
- Being obsessed about caring for the infant
- Hallucinations, which are usually auditory in nature
- Insomnia or frequent awakenings at night
- Homicidal or violent thoughts related to the infant
- Suicidal thoughts or suicide attempts
- Irritability
- Hyperactivity
- Suspiciousness
- Difficulty in communicating
Because the symptoms of postpartum psychosis are severe, it is considered a psychiatric emergency and almost always results in hospitalization for psychiatric treatment.
Individuals with the baby blues show signs of sadness and can be observed as having frequent crying spells. These patients often have the ability to care for themselves and their infant so they are relatively well kept, being able to care for herself. She is competent in caring for her infant so there are no signs of child abuse or neglect.
Individuals with postpartum depression have more severe symptoms than the baby blues. They show signs of being disheveled because the symptoms interfere with the woman’s ability to care for herself. She shows signs of frequent crying and will be disinterested in activities she once enjoyed. She also shows evidence of child neglect, but rarely will show evidence of child abuse. This is a woman who is extremely overwhelmed and has some inability to care for her infant.
Individuals with postpartum psychosis have obvious signs of the disorder. She appears confused and delusional around issues related to parenthood. She may show evidence of hallucinations and has a marked inability to care for herself and her infant. The signs of this disorder are both obvious and severe, which is why hospitalization as soon as the signs appear is warranted.
Tests and Investigations for Psychiatric Disorders in Pregnancy
There are no lab tests that can diagnose the baby blues, postpartum depression or postpartum psychosis, although blood tests may be done to rule out any other physical illness that may mimic psychiatric diseases, such as hypothyroidism. There are psychological tests that can identify postpartum mental illnesses. Most obstetricians will do a Patient Health Questionnaireor PHQ-9, which helps identify women at risk for postpartum depression.
If the symptoms appear to be severe, an Edinburgh Postnatal Depression Scale or EPDS can be done. This is a longer written question test that has a high correlation with postpartum depression if the woman shows evidence of being depressed.
Another test, called the Postpartum Depression Screening Scale or PDSS, has a high correlation with postpartum depression if the woman shows evidence of being depressed. These tests are done if the Patient Health Questionnaire indicates problems suggestive of depression.
There are ongoing research studies on the etiology, pathophysiology and treatment of postpartum psychiatric disorders. The etiology and incidence of the disease have already been well-established in the literature; however, recent research is delving into the biological causes of these disorders. By understanding the biological cause of the disorder, treatments can be developed based on biology, rather than on symptoms.
Pathology of Psychiatric Disorders in Pregnancy
There are no pathological tests that can diagnose the baby blues, postpartum depression, or postpartum psychosis. There are no routine tests or used on a regular basis to diagnose postpartum psychiatric diseases using CT scanning, MRI scanning or SPECT imaging. There is ongoing research on the use of SPECT scanning in depression that may, one day, be used to find brain pathology indicative of depression.
Differential diagnosis
The differential diagnosis of baby blues includes postpartum depression, major depressive disorder, seasonal affective disorder, acute stress disorder and dysthymia.
The differential diagnosis of postpartum depression includes major depression, hypothyroidism, anemia, bipolar disorder, dysthymia, baby blues, seasonal affective disorder, acute stress disorder, and postpartum psychosis.
The differential diagnosis of postpartum psychosis includes baby blues, postpartum depression, acute stress disorder, seasonal affective disorder, bipolar disorder, acute psychosis, delirium, and schizophrenia.
Treatment of Psychiatric Disorders in Pregnancy
There is no treatment for the baby blues. They tend to resolve spontaneously and only supportive measures such as reassurance and brief talk therapy are warranted if the woman feels she needs these things to support her in the few weeks that this disorder lasts.
Image: “Fluoxetine structural formula.” No machine-readable author provided. Sunridin assumed (based on copyright claims). License: CC BY-SA 4.0
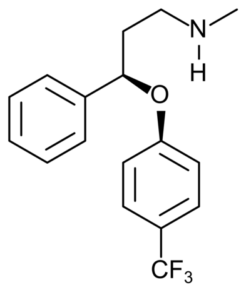
Women with postpartum depression can be treated with selective serotonin reuptake inhibitors, such as fluoxetine, paroxetine, escitalopram, sertraline and fluvoxamine. There are risks to taking these drugs in breastfeeding mothers so the risks need to be weighed against the benefits before using these drugs.
Some women benefit from electroconvulsive therapy as this has no risks for the infant. Psychotherapy is also a first-line treatment for postpartum depression, with cognitive behavioral and family-centered therapies being the best options.
Women with postpartum psychosis represent a psychiatric emergency as these women are significantly symptomatic and are at a high risk of suicide and homicide. These women are often treated aggressively with atypical antipsychotic medications, such as ziprasidone, quetiapine and risperidone. Other antipsychotics, such as olanzapine, haloperidol and clozapine have been used and have been found to be effective in treating these patients.
Psychotherapy generally only helps psychoses after the initial crisis has been averted, and family-centered therapy can help the patient and her family pick up the pieces left behind as the patient recovers from this severe disorder. Electroconvulsive therapy can be used to decrease any depressive symptoms.
Complications and Prognosis of Psychiatric Disorders in Pregnancy
Fortunately, there are no complications of the baby blues, which resolves spontaneously without treatment. The care of the infant is generally not affected, and the mother and infant do well after the disorder has resolved.
Women with postpartum depression generally resolve their symptoms over several weeks or months after being treated for the disorder. The major complication of this disorder is impaired maternal child bonding, which may not be reversible.
Infants of mothers who have had postpartum depression show behavioral problems and developmental delay during early childhood. Suicide can be a complication of postpartum depression as well.
Children of women with postpartum psychosis also show behavioral problems and developmental delay in early childhood because of the breakdown of the maternal child bond. The most significant complication of this disorder is homicide or the killing of the infant and maternal suicide.
The prognosis of the baby blues is excellent although some of these women will go on to develop postpartum depression and have a greater than average risk of developing the disorder.
Women with postpartum depression usually resolve their symptoms within 6-12 months after treatment. They are at a higher risk of developing major depressive disorder later in life when compared to women who do not have postpartum psychosis. There is also a disruption of the maternal infant bond, which can leave lasting changes in the child’s behavior and developmental progress.
The prognosis of postpartum psychosis is excellent, with good response to antipsychotic medication, brief hospitalization, and family-centered supportive therapy after they resolve their psychosis. There is a temporary disruption of the maternal infant bond, which can lead to developmental delays and behavioral problems in the infant that can last through early childhood. Suicide and homicide are possible, but do not happen after adequate treatment.
Prevention of Psychiatric Disorders in Pregnancy
All of the postpartum psychiatric disorders can be prevented through the use of the Patient Health Questionnaire or PHQ-9. Most obstetric and family practice clinics who do obstetrical care will do a questionnaire similar or identical to the PHQ-9 in order to detect early changes in mood that can reduce the incidence of psychiatric disease and its sequelae by offering early supportive treatment for the mother, the infant and her family.
Prognosis
The prognosis of postpartum disorders is good if treated properly. 75–86% remained symptom-free after a single episode. The relapse rate in subsequent pregnancies can be as 25–40%.
Review Questions
The correct answers can be found below the references.
1. The patient presents to the office a week after delivering an infant and tells you she has frequent crying spells and mood swings, but is able to care for herself and the infant. What test might identify mood changes warranting further investigation?
- The Minnesota Multiphasic Personality inventory
- The Patient Health Questionnaire-9
- The Edinburgh Postnatal Depression Scale
- The Postpartum Depression Screening Scale
2. The patient is referred to you by her husband, who is desperately worried about her. She is four weeks postpartum and has persistent thoughts that the baby is trying to tell her to kill herself. She hears the baby talk to her and is contemplating suicide. What is the best intervention?
- Give the patient the Edinburgh Postnatal Depression Scale
- Start a selective serotonin reuptake inhibitor
- Refer the family to a family-centered therapist
- Hospitalize the patient and start antipsychotics
3. The patient is a woman who is two months postpartum. She has persistent feelings of sadness, guilty feelings, and a lack of interest in caring for herself and her infant. She is breastfeeding and does not want to stop, but requests some kind of treatment. What treatment might be best for this patient?
- A selective serotonin reuptake inhibitor
- Electroconvulsive therapy
- A tricyclic antidepressant
- Psychoanalytic-based therapy

Comentários
Enviar um comentário