Placenta – Functions and Insufficiency
Table of Contents
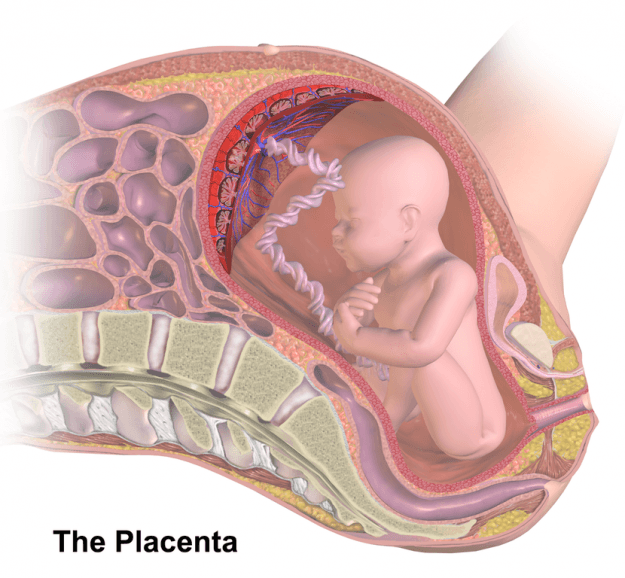
Image: “Placenta” by BruceBlaus. License: CC BY-SA 4.0
The Placental Circulation
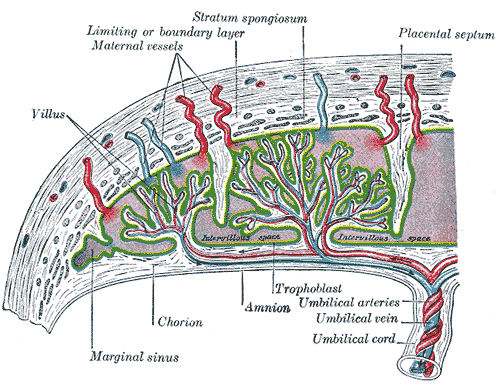
Image: “Maternal blood fills the intervillous space. Nutrients, water and gases are actively and passively exchanged, then deoxygenated blood is displaced by the next maternal pulse.” by Henry Gray. License: Public Domain
The placenta is a connection between mother and child. An exchange of gas and substances takes place via the so-called placental barrier. This consists from the end of the 3rd gestation week from the endothelium of the fetal blood vessels, the mesoderm and the cyto- and syncytiotrophoblast. This barrier ensures that there is, at no time, a direct link between the blood circulations. The exchange surface of the placenta is the surface of the chorionic tree. Maternal blood flows around this surface and facilitates the exchange of substances with it.
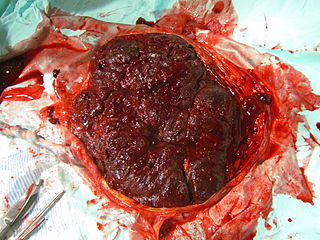
The maternal placenta is then expelled after the termination of pregnancy as afterbirth.
Placental Function
The placenta has, in addition to the metabolic function, an endocrine and immunologicalfunction.
A major task is the exchange of substances through the placental barrier. Most substances are transported in accordance with their concentration gradient. Other molecules, such as water, lactate and glucose, are transported actively.
During pregnancy, the placenta represents another major, endocrine gland. It is related to the mother’s pituitary gland and the childish adrenal glands. As the placenta is not hormonally active at the beginning of early pregnancy, hormone production is maintained first by the ovaries and the pituitary. They produce steroids (estrogen, progesterone) and human chorionic gonadotropin (hCG) and human placental lactogen (hPL).
The estrogen concentration increases steadily in the course of pregnancy. The hormone causes the uterus growth and supports at the end of pregnancy the birth preparedness. Progesterone is an important hormone for obtaining early pregnancy. In the first weeks, the progesterone is produced by the corpus luteum graviditis; this is then usually taken before the 12th week of pregnancy by the syncytiotrophoblast. The progesterone lowers the uterinemuscle tonus.
The hCG is produced by syncytiotrophoblasts. The hormone concentration rises continuously until the end of the 1st trimenon. In the first weeks of pregnancy, the hCG concentrations should double every 2 days.
The hPL is also formed by the trophoblast. It has structural similarity to the somatotropin and has thus growth hormone-like effects. Besides, it has an insulin-stimulating effect. On the one hand, this promoted the supply of glucose and amino acids – on the other hand, this is often the cause of gestational diabetes.
The placenta also has an immunological function. It favors the supply of the child with maternal IgG. Even after the child’s birth, the immunoglobins exist in the blood of the child.
Image: “Maternal side of a whole human placenta, just after birth” by תמרה דהן – דולה. License: CC BY-SA 3.0
The Placental Insufficiency
The placental insufficiency corresponds to an insufficient supply of the child with nutrients. The placental insufficiency can be distinguished in an acute and chronic form.
The acute form occurs after a few minutes or hours and the chronic placental insufficiency after weeks to months, whereby the chronic form corresponds with intrauterine growth retardationof lack of development.
Pathogenesis of placental insufficiency
Causes of a malfunction of the placenta in the acute form may be a vena cava compression syndrome or intrapartum an inferior placental abruption.
The chronic placental insufficiency arises in maternal systemic diseases such as anemia, diabetes mellitus or the presence of uterus myomatosus. In addition, the pregnancy-related disorders play a role, including the multi-parity, rhesus incompatibility and abortions.
Clinic of placental insufficiency
Symptoms of acute placental insufficiency depend on the cause. In placental abruption, severe pain right up to board hard uterus are possible. Typically, it comes in acute placental insufficiency to a change of the CTG.
The chronic placental insufficiency manifests itself less with maternal symptoms; it leads the child to a growth restriction and intrauterine asphyxia. The symptoms may develop up to a sudden death of the child.
Diagnosis of placental insufficiency
The diagnosis of acute placental insufficiency is provided by the CTG. Typical findings are late decelerations, a silent type of oscillation or a persistent bradycardia. Frequently, a sonography is performed to confirm the diagnosis.
The chronic placental insufficiency is secured by sonography. Particular attention in the sonography applies the amount of amniotic fluid. A small amount of amniotic fluid would be a typical sign.
Therapy of placental insufficiency
Treatment is initially causally and causes of the insufficiency should be eliminated. The choice of treatment also depends on the week of pregnancy.
Acute causes can be eliminated, for example, by a left lateral position (vena cava compression syndrome). In chronic forms, the risk and benefit should be weighed. Among other things, this involves the risk of prematurity against the risk of a chronic shortage supply. Accordingly, it is then decided whether a section is recommended or not.
Review Questions
The answers can be found below the references.
1. Which of the following hormones are not produced by the placenta?
- Somatotropin
- Human chorionic gonadotropin
- Human placental lactogen
- Progesterone
- Estrogens
2. Which is a common cause of acute placental insufficiency?
- Left lateral position
- Vena cava compression syndrome
- Insertio velamentosa
- Uterine rupture
- Obstipation
3. Which testing provides the diagnosis security of chronic placental insufficiency?
- Leopold handle
- Sonography
- CTG
- Doppler sonography of the kidneys
- Blood pressure measurement
Comentários
Enviar um comentário