Types of Headache — Migraine, Cluster Headache and more
Headache is one of the most common symptoms in the emergency department and outpatient clinics. It can be a sign for serious illness that needs immediate action to prevent fatal consequences e.g. subarachnoid hemorrhage, meningitis and temporal arteritis. Headache also can be a sign of chronic physical and mental illnesses. Careful history taking and physical examination should be performed to any patient complaining of headache for proper diagnosis and management.
Table of Contents
Are you more of a visual learner? Check out our online video lectures and start your neurology course now for free!

Image: “Man with headache.” by Phee – Pixabay. License: CC BY-SA 4.0
Overview
Headaches can be considered a protective mechanism that may indicate a serious underlying pathology. It can be primary with no pathological predisposition e.g. migraine and cluster headache or secondary to other disorders e.g. sinusitis, hypertension emergencies or brain tumors.Evaluation of patients with headache is directed towards elimination of serious life threatening conditions, then diagnosis.
Possible causes of subacute headache include brain tumors, CNS infections, CNS hemorrhage, hypertension and systemic inflammatory diseases.
More chronic headaches are usually tension headache, migraine, cluster headache, sinusitis, refractive errors and tempromandibular joint dysfunction. Patient history is the first diagnostic tool.
For exclusion of danger signs during evaluation, the mnemonic “snoop” is used. Presence of any of these manifestations prompts further investigations to know the exact pathology.
- Systemic disorders (fever, HIV state or pregnancy)
- Neurological deficit may suggest brain hemorrhage or meningitis. Conscious level, vision and cranial nerves should be checked in details.
- Onset headache (new or sudden) that needs to be fully investigated.
- Other associated conditions e.g. head trauma or intoxication.
- Change of present headache can be a sign of progression or another pathology. The most common type of headache among populations is tension headache but the most presentable type of headache to primary care physicians is migraine.
Red Flag Headaches
Giant cell arteritis
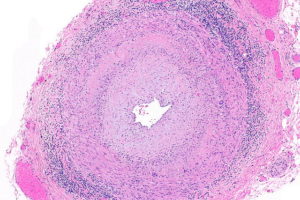
Image: “Micrograph of giant cell arteritis (also temporal arteritis). H&E stain.” by Nephron – Own work. License: CC BY-SA 3.0
Hypertensive emergencies
Elevated blood pressure with end organ damage can present with headache. Further investigation is required to prevent brain hemorrhage, retinal hemorrhage, renal failure and pulmonary edema. Sodium nitroprusside is used for rapid lowering of blood pressure in hypertensive emergencies.Subarachnoid hemorrhage
Subarachnoid hemorrhage refers to blood in the subarachnoid space due to rupture of brain aneurysm or arteriovenous malformation. It can be spontaneous or traumatic with severe headache that can be described as the “worst headache of my life”.Clinical presentation also includes altered mental status, focal neurological lesions according to the location of hemorrhage, meningeal irritation and sometimes coma. CT scan is the first step for the diagnosis specially in patients with altered mental status.
Lumbar puncture with CSF analysis can be done following CT to exclude any brain space occupying lesions. Management of subarachnoid hemorrhage varies according to clinical presentation with ABC for comatose patients. Lowering intracranial tension with mannitol and diuretics will improve the mental status of the patients. Blood pressure control, hydration, supportive measures and antiepileptic prophylaxis are indicated.
Venous sinus thrombosis
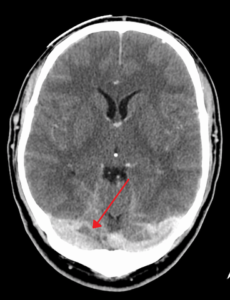
Image: “A dural venous sinus thrombosis of the transverse sinus. Greater on the right than left.” by James Heilman, MD – Own work. License: CC BY-SA 4.0
Brain infarction or hemorrhage can both be complications of sinus thrombosis due to blood congestion. It can be a complication of sinusitis, hypercoagulable states, lumbar puncture, brain surgery or medications e.g. steroids, oral contraceptives, tamoxifen and Epsilon-aminocaproic acid.
Treatment includes thrombolytic therapy, analgesics, lumbar puncture and antiepileptics.
Meningitis/encephalitis
Both refer to CNS infection. While meningitis is inflammation of the brain meninges due to viral, bacterial or fungal CSF infection, encephalitis is inflammation of the brain itself due to viral or autoimmune disorder. Clinical manifestations include fever, headache, photophobia, nuchal rigidity and focal neurological symptoms.Blood cultures, lumbar puncture and CSF analysis are used for confirming the diagnosis. According to the etiology, CSF sample differs in glucose content, WBCs infiltration, proteins and lactate concentration. Treatment is directed against the causative agent.
| Bacterial meningitis | Viral meningitis |
|
|
Glaucoma
Glaucoma is a common cause of headache due to elevated intraocular pressure. It can lead to optic atrophy and subsequent blindness. Acute angle glaucoma is acute in onset with eye pain, conjunctival injection, nausea and vomiting. Acute angle glaucoma is a medical emergency. Management is directed to lowering of the intraocular pressure.Primary Headache
Migraine
Migraines are usually paroxysmal, unilateral, throbbing headaches that can be accompanied by nausea, vomiting, phonophobia, and photophobia. It can be precipitated by many factors including visual stimuli, environmental factors, wine, stress, sleep disturbances, nitrites and aspartame.The pain can be moderate to severe lasting from 4 to 72 hours and localized to one lobe or an area of the head mainly the frontotemporal or the ocular area. It can also be associated with conjunctival injection, cardiovascular manifestations of hyper/hypotension, neurological symptoms of Horner syndrome, sensory abnormality and/or cranial nerve abnormality.
Migraine is usually proceeded by an aura which might be sensory or motor and usually lasts for less than one hour. Visual aura of scotoma is the most common and involves an arc or band of absent vision within the visual field.
Chronic migraine is defined as having 15 or more migraine headaches a month for at least 3 months.
Diagnosis of migraine is done clinically with no need for imaging studies in patients with typical recurrent attacks. Patients with migraines usually avoid sudden movement, which can precipitate the attacks unlike patients with cluster headache which is severe enough to make the patient restless and irritable.
Management is mainly abortive for the acute attacks and prophylaxis for prevention of future attacks. Acute managements include triptans, ergot alkaloids and NSAIDs. Preventive management includes beta blockers, tricyclic antidepressants, antiepileptics, calcium channel blockers, SSRIs and NSAIDs.
| Mild headache | Moderate to severe headache |
| Dopamine agonist or antiemetic medications
Intravenous fluids Depakote |
Tension headache
A tension type headache is usually bilateral headache with mild to moderate severity and can lasts between a few minutes to several days. It can be associated with pericranial muscle spasm or tenderness in the neck and scalp.The pain starts in the back of the head and neck, then spreads as tightness or pressure band. It is not usually associated with nausea or vomiting and no disability of the affected patients.
Chronic tension headache is diagnosed when the attacks occur for 15 or more days a month for at least 3 months. It is usually triggered by stressful events, depression and abnormal head posture. There is no aura or prodrome with tension headache and the neurological exam should be normal except for some tenderness or spasm of the neck muscles.
Management of tension headache is mainly to avoid the triggering stressors. Relaxation techniques, cold or hot packs, ultrasound, acupuncture, NSAIDs (Ibuprofen, naproxen), and diphenhydramine.
Cluster headache (Horton’s syndrome)
This is a form of severe unilateral periorbital headache in the trigeminal nerve distribution with conjunctival injection, lacrimation, nasal congestion and rhinorrhea. Sometimes it can be associated with miosis and ptosis. The pain usually lasts few minutes to hours.The attacks are commonly recurrent at the same time every night and awake the patient from sleep. The pain is severe and the patient is restless and irritable. Heavy smoking and alcohol use are risk factors for development of cluster headache as well as histamine and head trauma.
Chronic cluster headache occurs when the headache free interval is less than one month or when it lasts for more than one year. Abortive management of cluster attacks include oxygen inhalation therapy, triptans e.g . sumatriptan, ergot alkaloids, caffeine and instillation of local anesthetics into the nostrils.
Prophylactic management includes calcium channel blockers e.g. verapamil & diltiazim, lithium, prednisolone and antiepileptics.
New daily persistent headache
Primary headache that is unremitting daily for more than 3 months. It is usually bilateral, mild to moderate headache, tightening in quality and can be associated with photophobia, phonophobia and mild nausea.The etiology is unknown but most patients report infection or flu-like illness and sometimes stressful life event. Patients usually remember the exact date it started.
This is a diagnosis of exclusion. Various medications have been tried for management of new daily persistent headache including propranolol, amitriptyline, gabapentin and pregabalin.
Hemicranias continua
Primary unremitting persistent headache that can have severe exacerbations. The pain is unilateral and associated with miosis, ptosis, conjunctival injection or rhinorrhea. It responds well to indomethacin.Idiopathic/benign intracranial hypertension
Also called pseudotumor cerebri, this is a known cause of chronic headache characterized by symptoms of increased intracranial tension i.e. headache, vision loss, nausea, vomiting and papilledema without any evidence of space occupying lesion in neuroimaging.The symptoms can also include pulsatile tinnitus, and abducens nerve and other neurological deficits. The symptoms are relieved after lumbar puncture to relieve the pressure, or medications which lower CSF pressure.
The disease is common in women of child bearing age. Lumbar puncture should be proceeded with MRI to avoid brain stem herniation in case of space occupying lesion.
Elevated CSF opening pressure with normal CSF composition is both diagnostic and therapeutic. Carbonic anhydrase inhibitors, acetazolamide is used effectively to lower the CSF production.
Headache with increased intracranial tension can also be present with space occupying lesions including tumors, CNS abscess or hemorrhage.
Miscellaneous
Pheochromocytoma is characterized by intermittent hypertension with headache, palpitations and sweating. It is due to hypersecretion of the adrenal medulla.
Image: “Subarachnoid hemorrhage in CT. One can see the blood hyperattenuating in the basal cisterns.” by Hellerhoff. License: CC BY-SA 3.0
Thunderclap headache refers to a severe form of headache that arises suddenly. It can be due to subarachnoid hemorrhage, stroke, cervical artery dissection, pituitary apoplexy or hypertensive crisis.
Chronic subdural hemorrhage is chronic hemorrhage localized within the subdural space specially in old age due to brain atrophy and minor head trauma. The blood accumulates over a long period with symptoms of headache, cognitive disability and focal neurological abnormality. Treatment is usually surgical evacuation of the hematoma.
Acute and chronic sinusitis can be associated with headache which mimics migraine or tension headache. Other sinus symptoms include fever, nasal congestion and rhinorrhea. The headache is usually pressure-like and periorbital and lacks other manifestations of migraine or tension headache. Treatment involves decongestant, antibiotic and analgesics.
Medication overuse headache is a chronic headache with repeated analgesic use, which may lead to rebound headaches.
Cranial neuralgias include herpetic neuralgia and trigeminal neuralgia, which are stabbing sharp pain at the nerve distribution. Medical management with gabapentin or pregabalin and surgical management can be done to decompress the nerve origin to prevent the attacks.
Diagnostic Tests
- Blood draws e.g. CRP, CBC, ESR are first indicated to exclude systemic inflammatory conditions which might precipitate the headache.
- Brain imaging using CT and MRI for brain tumors or lesions, hemorrhage, stroke, trauma and benign intracranial hypertension.
- Lumbar puncture and CSF analysis in case of infection, subarachnoid hemorrhage and benign intracranial hemorrhage.
- Fundal examination for cases of headaches due to brain tumor, hypertension, benign intracranial hypertension glaucoma and HIV.

Comentários
Enviar um comentário