Amebicidal Drugs
Table of Contents
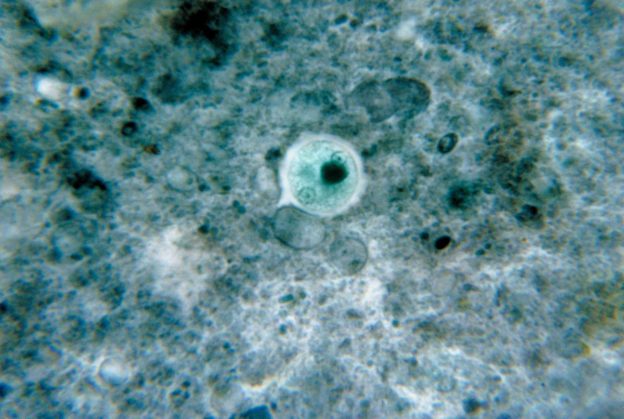
Image: “This micrograph stained with chlorazol black revealed an Entamoeba histolytica cyst.” by CDC/ Dr. George Healy – This media comes from the Centers for Disease Control and Prevention’s Public Health Image Library (PHIL), with identification number #1474. License: Public Domain
Overview of Amebiasis
Amebiasis is an infection of the intestine caused by Entamoeba histolytica. It is a protozoan parasite. Human beings and other non-human primates are the main hosts. Infection occurs by ingestion of water and food contaminated with feces. The contaminated food/water contains the cysts of Entamoeba histolytica. It can cause extra-intestinal invasive infections.
E. dispar and E. histolytica are the only pathogenic amoebas known to humans. The protozoan enters the digestive tract and multiplies in the terminal ileum or colon to the trophozoite stage. Trophozoite of E. Histolytica is a motile form.
Inside the intestine, it causes necrosis and perforation of the intestinal wall. It can also penetrate the intestinal wall and reach the liver via the portal vein, where it may cause a fatal liver abscess.
Cysts are excreted into the feces. The life cycle of E. histolytica is completed at this stage. It can survive in the environment for weeks to months. Factors that increase the chances of amebiasis are travel to an endemic area, consumption of contaminated food/water and anal intercourse. The infection can cause an asymptomatic disease to mild to moderate intestinal cases (ulcers, dysentery) to severe or chronic cases.
Amebiasis is prevalent highly in developing countries where general sanitation hygiene is not available.
The classic symptoms of amebiasis are bloody or watery diarrhea, fever (10—30 % patients), anorexia, and weight loss. Rectal bleeding can occur without diarrhea in children. It remains asymptomatic in most individuals and resolves on its own. Invasive infections result when E. histolytica reaches organs such as the liver via the systemic circulation. If the infection is limited to the intestine it is called non-invasive infection.
Treatment is therefore directed at disinfecting luminal trophozoites (non-invasive infection), as well as those in the tissue (invasive infection) if the infection has spread to that extent. Not all drugs can disinfect the cysts of E. histolytica. Drugs are usually active either in the tissues or in the intestinal lumen, thereby necessitating a combination therapy for symptomatic amebiasis.
Patients should be educated to avoid contaminated food/water or undercooked food.
Functional and Chemical Classification of Amebicides
Tissue amebicides
- Nitro-imidazoles: Metronidazole, Tinidazole, etc.
- Alkaloid derivatives: Emetine and Dehydroemetine
Luminal amebicides
- Amide: Diloxanide furoate, Nitazoxanide
- 8-Hydroxyquinolines: Iodoquinol
- Antibiotics: Tetracycline and Erythromycin
Amebicidal Drugs
Tissue amebicides
Metronidazole
- A nitro-imidazole
- Selectively toxic to anaerobic microorganisms
- Half-life of metronidazole is 7.5 hours.
Tinidazole
Tinidazole is a second-generation nitro-imidazole. Its efficacy equals that of metronidazole, but it has a shorter course of treatment (3 days vs. 10 days for metronidazole), has a longer half-life (12—14 hours), and is more expensive.
Other nitro-imidazoles
- Secnidazole, ornidazole, and satranidazole
- They are similar to metronidazole/tinidazole but with a longer half-life.
- Satranidazole has much better tolerability (lower side effects).
Nitazoxanide
Nitazoxanide is a new nitrothiazole antiparasitic drug and Prodrug – gets converted to tizoxanide. Effective against numerous intestinal protozoa and helminths
Emetine & Dehydroemetine
Because of toxicity concerns rarely used. For example, severe amebiasis when metronidazole cannot be used. These act only against the trophozoites but not against the cysts.
In the setting of severe amebiasis, these drugs should be administered s.c. or i.m. (and not i.v.) for at least 3—5 days.
Luminal amebicides
Diloxanide furoate
- Amide
- Directly kills luminal trophozoites
- It does not kill the tissue trophozoites.
- No antibacterial action
- Prodrug (releases free diloxanide as the active metabolite)
Iodoquinol
Directly kills amebic trophozoites, thereby inhibiting cyst production. Ineffective as tissue amebicide.
Paromomycin
- Aminoglycoside
- May be superior to diloxanide in asymptomatic infection.
- It is only active as luminal amebicide.
Other antibiotics
Some antibiotics can be used in the treatment of intestinal amebiasis. Examples include erythromycin and tetracycline.
Summary of Antiamebicidal Drug Treatment
*Diloxanide furoate is not available in the United States.
Review Questions
The correct answers can be found below the references.
1. Which of the following statements regarding amebicides is correct?
- Diloxanide furoate is the drug of choice in hepatic amebiasis.
- Iodoquinol inhibits the protein synthesis of E. histolytica.
- Paromomycin is a diaminopyrimidine derivative.
- Tinidazole is ineffective in cases of metronidazole resistance.
- Metronidazole is used for amebiasis as well as postoperative prophylactic antibiotic therapy.
2. Which of the following is the mechanism of action of metronidazole?
- Prevents the conversion of heme to hemozoin
- Inhibits the nucleic acid synthesis
- Inhibits the pyruvate synthesis
- Damages the plasma membrane of amoeba
- Inhibits the ATP synthesis in amoeba
3. Which of the following is the first-line drug for invasive amebiasis?
- Metronidazole
- Paromomycin
- Diloxanide Furoate
- Nitazoxanide
- Iodoquinol
Comentários
Enviar um comentário