Temporal Arteritis (Giant Cell Arteritis) and Carotid Artery Stenosis — Symptoms and Treatments
Table of Contents
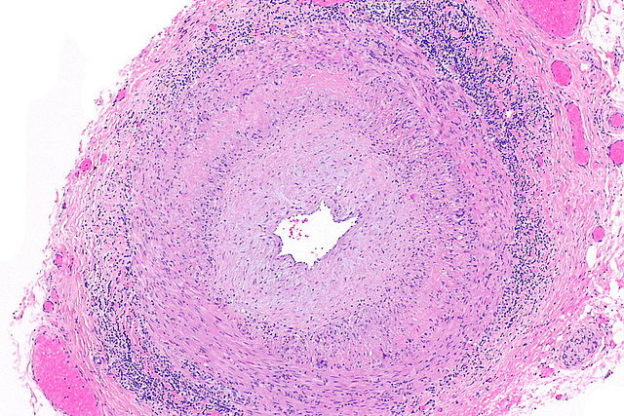
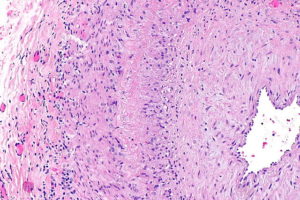
Image: “Micrograph of giant cell arteritis (also temporal arteritis). H&E stain.” by Nephron – Own work. License: CC BY-SA 3.0
Temporal Arteritis
Temporal arteritis, also known as giant cell arteritis (GCA), is a systemic inflammation of the vessel with no known cause. In other words, it is the vasculitis of the superficial temporal artery. It usually affects people of old age. Inflammation of the vessel wall produces systemic, neurologic and ophthalmologic signs and symptoms.
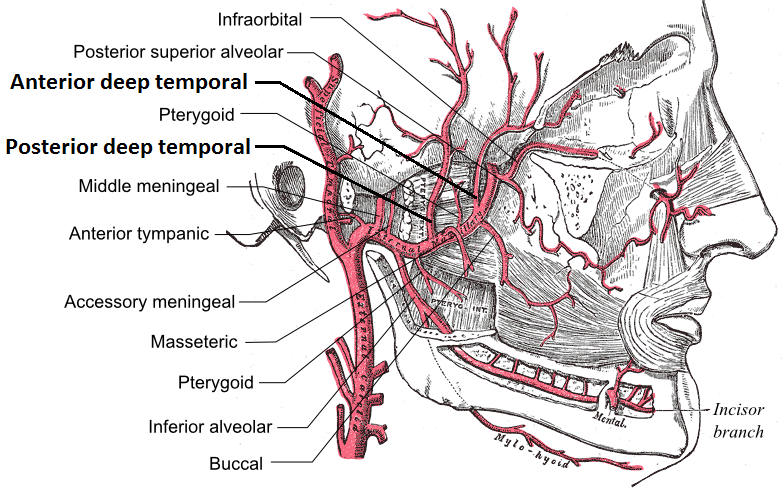
Image: “Branches of the maxillary artery” by Mikael Häggström – File: Gray510.png, License: Public Domain
GCA is the most common form of systemic vasculitis in adults. It is also called arteritis cranialis, Horton disease and granulomatous arteritis. Giant cell arteritis can involve other vessels as well like ophthalmic, occipital, vertebral, posterior ciliary and proximal vertebral arteries; but it commonly involves the superficial temporal artery.
Sometimes large vessels like aorta, carotid arteries, subclavian arteries and iliac arteries are also involved. Untreated temporal arteritis can complicate into aneurysms, strokes, and even death.
Histopathology of temporal arteritis
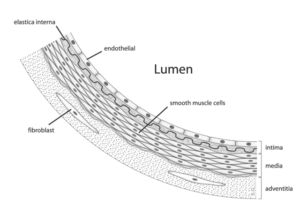
Image: “Arterial anatomy” by Stijn A.I. Ghesquiere www.applesnail.net – Own work. License: CC BY-SA 2.5
Trans-mural inflammation of the layers of the blood vessels, i.e. of the intima, media, and adventitia of affected arteries leads to the signs and symptoms of this disease.
Immune response to the disease leads to infiltration by lymphocytes, macrophages and multinucleated giant cells.
Hyperplasia of the layers of the vessels can lead to luminal narrowing, causing distal ischemia.
Pathophysiology of temporal arteritis
Giant cell arteritis (GCA) is a cell-mediated immune response to endothelial injury, i.e. abnormal response of the injury.
Etiology of temporal arteritis
The underlying cause is still not exactly known. Research in the field of inflammatory response of the body is being carried out to understand the pathophysiology of the disease. Triggering factors responsible for the inflammatory response are still under study. Various genetic, environmental and autoimmune factors have been identified.
Epidemiology of temporal arteritis
Temporal arteritis is more common in older females. The female-to-male ratio is roughly 3.7:1.
Risk factors include:
- Smoking
- Old age
- Depression and stress
- Family history of temporal arteritis
- Female gender
Smoking increases the risk of temporal arteritis by 6-fold in women. It has been seen in many studies that diabetic patients have a lesser risk of giant cell arteritis.
Old age is the major risk factor for this disease. It is common in females of more than 50 years and rare in people below 50 years age. Maximum chance of developing temporal arteritis is at the age of 80 or above.
Signs and Symptoms of Temporal Arteritis
Temporal arteritis commonly has a sudden onset. In some patients, prodromal symptoms may also be present as anorexia, fever, malaise, general body ache and pains, night sweats as well as weight loss. These may last a few days or persist for weeks, along with other symptoms of the disease.
Major signs and symptoms
- Headache: This is the major symptom. It is usually localized in occipital or temporal region of the head. This complaint is either a new symptom for the patient or of a new type of headache in patient with previous history of chronic headaches. The duration of headache can be short or longer and is usually throbbing and continuous in nature. Some people may describe it as a dull or burning pain in the head.
- Neck, shoulder, and pelvic girdle pain along with polymyalgia rheumatica
- Fatigue and malaise with generalized body aches and pains
- Jaw claudication: the feeling of fatigue or tiredness of the jaw muscles while eating solid food or even during periods of prolonged speaking. This feature is diagnostic for giant cell arteritis because it occurs due to ischemia in the vessel supplying the masseter muscle.
- Fever
- Visual loss: this is the most significant cause of morbidity in this disease. Permanent loss or disturbance can occur in roughly 20% of the patients and, in some patients, bilateral blindness is also reported.
Some other lesser common symptoms
- Cramping arms after exertion
- Audible pulsations or bruits over the axillary region
- Cramping or aching legs while walking which improves with resting
- Dry cough
- Double vision
Other complications
- Limb claudication
- Transient ischemic attacks (TIAs) or stroke
- Scintillating scotoma
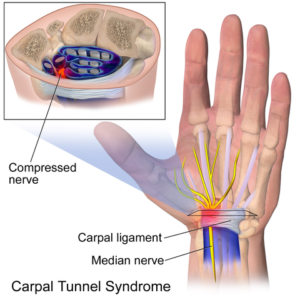
- Carpal tunnel syndrome (5 %) or other peripheral neuropathies
Physical examination of temporal arteritis
Various signs are produced depending on the organ or vessel involved with inflammation of the vessel wall. Consultant opinion should be taken from ophthalmologist, head and neck specialist and neurologist.
Blood pressure should be taken bilaterally from the arms to rule out aortic arch involvement. Carotodynia, i.e pain during palpation of the carotid artery, is common in about 15% of patients of temporal arteritis. Cranial nerve examination for cranial nerve palsies should be done especially for the sixth nerve palsy. The carotid, axillary, and brachial arteries should be assessed for bruits.
Ophthalmic examination
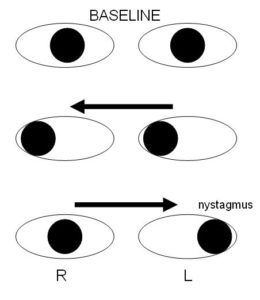
Image: “Internuclear ophthalmoplegia” by Samir at the English language Wikipedia, License: CC BY-SA 3.0
A complete eye examination including visual acuity, visual field check and fundoscopy with slit lamp examination should be done. Neuro-ophthalmic manifestations of GCA include the following:
- Diplopia
- Ptosis
- Nystagmus
- Intranuclear ophthalmoplegia
- Pupillary abnormalities
Diagnosis of Temporal Arteritis
Early diagnosis and early treatment is the key to a better prognosis. It is recommended that treatment should be started before confirmation of treatment. The diagnosis is made by following investigations:
Image: “Micrograph of temporal arteritis” by Nephron – Own work. License: CC BY-SA 3.0
- Color duplex ultrasonography: Duplex ultrasound of the temporal artery is an alternative to temporal artery biopsy (TAB).
- C- reactive proteins (CRP): This originates in the liver and is a more reliable prognostic factor as compared to the ESR. It is not affected by age, gender and other hematologic parameters.
- Temporal artery biopsy (TAB): After using a local anesthetic, a piece of temporal artery from under the scalp is taken as a sample for biopsy. The histopathology of the biopsy sample can confirm the diagnosis. A temporal artery biopsy leaves a small scar and causes almost no pain.
- CBC with ESR: Raised TLC and raised ESR will show the presence of inflammation. Raised ESR is very significant in the diagnosis of this disease. ESR commonly exceeds 50 mm/h and may exceed 100 mm/h or it can be normal in 7-20% of patients. Patients with temporal arteritis often present with normochromic and normocytic anemia. TLC is usually normal in all patients whereas the platelet count is often elevated.
- Liver function test (LFT): Liver function tests are also elevated in about 20% of the patients.
- CT scan and MRI of the head and neck: These investigations are done to look for complications due to ischemia. Cervico-cephalic arteritis can lead to multiple infarctions. These infarctions can be seen on CT or MRI.
American College of Rheumatology diagnostic criteria
A diagnostic criterion for giant cell arteritis was issued by the American College of Rheumatology. Presence of three of the following will be considered having giant cell arteritis:
- Age of the patient: 50 years or more
- New-onset localized headache or localized head pain of different pattern
- Temporal artery tenderness on palpation or decreased pulsation
- ESR of 50 mm/h or higher
- Positive arterial biopsy results, i.e histological features of vasculitis characterized by mononuclear infiltration or granulomatous inflammation, usually with multinucleated giant cells.
Treatment of Temporal Arteritis
The treatment of giant cell arteritis (GCA) is high-dose corticosteroid therapy and it is accepted worldwide. Steroid therapy is started as soon as a physician suspects temporal arteritis due to the danger of blindness if kept untreated.
Those patients who present initially with visual symptoms have more chances of improvement when steroid therapy is started on the first day. After 48 hours, visual symptoms are irreversible sometimes, even after steroid treatment. Typically, treatment begins with 40–60 mg of prednisone orally, once daily. Patient starts to improve in 2-3 days. If blindness develops, it is irreversible.
British guidelines recommend the following schedule for tapering of standard-regimen corticosteroids:
- Continue prednisolone, 40-60 mg (not <0.75 mg/kg) for 4 weeks (or until symptoms and laboratory abnormalities resolve), then
- Reduce dose by 10 mg every 2 weeks to 20 mg, then
- Reduce dose by 2.5 mg every 2-4 weeks to 10 mg, then
- Reduce dose by 1 mg every 1-2 months, provided no relapse occurs.
Low-dose aspirin and immunosuppressants may also be used to reduce the risk of the condition recurring and complications developing.
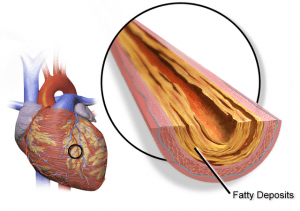
Carotid Artery Disease
Carotid artery disease, also called carotid artery stenosis, is the narrowing of the lumen of the carotid arteries due to fat and cholesterol deposition. This deposition of fat, which leads to stenosis, is called plaque. The term carotid artery occlusion means the complete blockage of the artery. Carotid artery occlusion can worsen into cerebral ischemia and stroke.
The carotid arterial system is the major arterial supply to the brain. The arch of the aorta gives off the left common carotid artery and the brachiocephalic trunk gives off the right carotid artery which later on divide into internal and external carotid arteries. These split into the external and internal carotid arteries at the upper border of the thyroid cartilage at around the level of the fourth cervical vertebra. Atherosclerosis of these arteries can lead to disturbance of blood supply to the major organs and tissues and can even lead to stroke.
Causes of carotid artery disease
Atherosclerosis is the main cause leading to carotid artery disease. Plaque can also deposit in other major blood vessels like in the coronary arteries. Plaque deposited in the blood vessels contains debris made of:
- Cholesterol
- Fat
- Cellular waste
- Protein
- Calcium
Atherosclerosis leads to the narrowing of the lumen of the involved vessels and making them stiff and less flexible with time. These changes decrease blood flow leading to a lower oxygen supply and more CO2 accumulation. Hypoxia leads to ischemia at the organ level.
CAD can also be the result of other diseases that cause arterial damage.
Risk factors for carotid artery disease
Similar to most heart diseases and stroke, the risk factors for carotid artery disease are:
- Age
- Smoking
- Hypertension (high blood pressure) — the most important treatable risk factor for stroke
- Abnormal lipids or high cholesterol
- Insulin resistance
- Diabetes
- Obesity
- Sedentary lifestyle
- Family history of atherosclerosis, either coronary artery disease or carotid artery disease
Men of age less than 75 years are at more risk than women younger than 75 years. This means carotid artery disease is more common in males than females below 75 years age, however, females older than 75 years have more chances of development of carotid artery disease than males older than 75.
People with coronary artery disease are more prone to develop carotid artery disease. Most often the carotid artery disease develops few years after coronary artery disease.
Signs and Symptoms of Carotid Artery Disease
Symptoms of carotid artery disease develop late after one of the carotid arteries is almost blocked. Blockage of carotid artery means when 80% or more of the lumen of the artery is blocked.
Blocked carotid artery can lead to stroke or TIA – transient ischemic attack any time in life. Embolization is the mechanism by which a small clot from the deposited plaque dislodges toward the brain and suddenly blocks one of the cerebral arteries, leading to a stroke. A TIA is basically the precursor of a future stroke and should be regarded as such, since a third of people who experience TIA go on to have a stroke within a year. Symptoms of a TIA last for only few minutes to few hours. These symptoms include:
- Sudden weakness or numbness in the face, arms, or legs (usually on one side of the body)
- Difficulty in speech (garbled speech) or understanding
- Sudden vision loss in one or both eyes
- Dizziness or drowsiness
- Sudden, severe generalized or localized headache
- Weakness in your limbs
- Numbness in one side of your face
- Drooping on one side of your face or eyelids
Atherosclerotic disease of the carotid artery is often associated with amaurosis fugax (transient ipsilateral visual loss), transient ischemic attacks (TIAs), crescendo TIAs, stroke-in-evolution, and finally cerebral infarction.
Diagnosis of Carotid Artery Disease
Early diagnosis and treatment can save the patient from many complications. High risk patients should be evaluated and examined routinely. An abnormal swishing sound can be auscultated over the blocked artery, called a bruit. Following investigations are done to diagnose this disease.
Image: “70% blockage of the right internal carotid as seen on ultrasound. Arrow marks plaque inside the artery.” by James Heilman, MD – Own work, License: CC BY-SA 4.0
Baseline blood tests
- CBC
- PT and APTT
- BUN and creatinine
- Lipid profile
Carotid ultrasound
Duplex ultrasound is the test of choice for screening purposes. The extent of carotid arterial stenosis can be estimated before doing any invasive procedure.
Computed tomography angiography (CTA or CT angiography)
CT scan after injecting contrast material is done to check the flow of the blood and patency of the blood vessels. CT angiography is also diagnostic in regard to the carotid artery disease.
Head CT scan
This is done in order to look for infarctions or intracranial lesions formed recently or older ones. This procedure takes pictures of the brain tissue to check for any bleeding or abnormalities.
Magnetic resonance angiography (MRA)
This test also uses a contrast to highlight arteries in the neck and brain to look for stenosis.
MRI scan
Sometimes some intracranial lesions are not visible on CT but can be seen on the MRI.
Cerebral angiogram
A catheter is passed into the carotid artery to inject dye in the artery followed by serial X-raysin search of abnormalities. This is an invasive test and it can lead to complications. It is usually avoided.
Treatment of Carotid Artery Disease
Following steps are taken to reduce the risk of complications and as treatment of the carotid artery disease:
- Quit smoking
- Exercising daily
- Eating healthy food
- Taking medications as prescribed
- Considering a procedure to improve blood flow
These steps include lifestyle changes which can improve blood cholesterol level and reduce episodes of raised blood pressure.
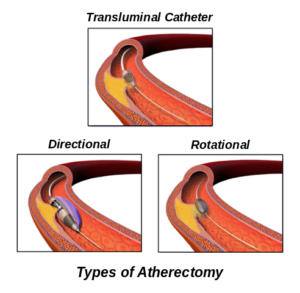
Image: “Types of atherectomy” by Jmarchn – Own work. License: CC BY-SA 3.0
Medical treatment
Taking aspirin, anticoagulants, antiplatelet therapyand platelet aggregation inhibitors along with lifestyle changes and regular monitoring through follow-up visits can improve the condition of the patients.
Invasive procedures
- Carotid endarterectomy (CEA)
- Carotid angioplasty and stenting
Complications of carotid artery surgery
Cardiac ischemia, cranial nerve injury (CNI), hematoma with or without airway compromise, hypertension or hypotension, perioperative stroke or recurrent stenosis.


Comentários
Enviar um comentário