Varicocele (Scrotum Varicose Veins) — Diagnosis and Treatment
Table of Contents
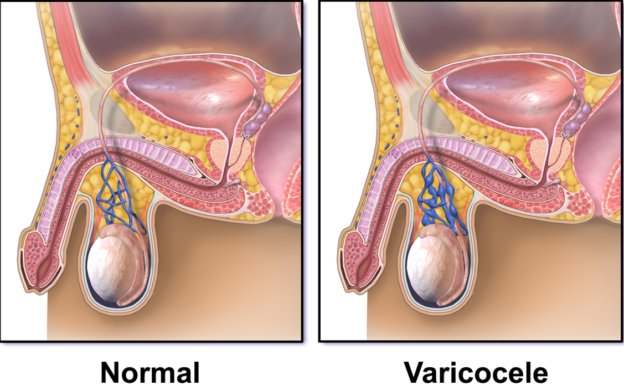
Image: “Normal pampiniform venous plexus, and varicocele.” by BruceBlaus – Own work. License: CC BY-SA 4.0
Definition of Varicocele
Varicocele is defined as the dilatation of the pampiniform venous plexus which is connected to the internal spermatic vein. Varicoceles are associated with impaired testicular hormonal function and infertility.
Epidemiology of Varicocele
To estimate the prevalence of varicoceles in males, it is good to differentiate between the general population and the subfertile population. While varicoceles can be identified in up to 20% of the general population, they are at least twice more common in subfertile men. Due to the relationship between varicoceles and subfertility, it has long been postulated that varicoceles are a common cause of poor sperm production and infertility.
Etiology of Varicocele
Varicoceles are left-sided in approximately 90 % of the cases and this can be explained by several anatomical features. The angle where the left testicular vein enters the left renal vein is steeper, and the increased renal vein pressure, due to its compression between the aortaand superior mesenteric arteries, both contribute to the increased risk of left varicoceles.
Also, of importance is that a one-sided varicocele can often affect the opposite testicle. Up to 35—40 % of men with a palpable left varicocele may have bilateral varicoceles that are discovered upon examination. A 2004 study by Gat et al suggested that up to 80 % of men with a left clinical varicocele had bilateral varicoceles revealed by noninvasive radiologic testing.
Classification of varicoceles
Varicoceles vary in size and can be classified into the following three groups:
- Large – Easily identified by inspection alone
- Moderate – Identified by palpation without bearing down (Valsalva maneuver)
- Small – Identified only by bearing down, which increases intra-abdominal pressure, thus impeding drainage and increasing varicocele size
Pathophysiology of Varicocele
Image: “Appearance of varicocele in 28-year-old’s scrotum.” by Jfday – Own work. License: CC BY-SA 4.0
Varicoceles are associated with subfertility in a significant number of patients. The direct physical pressure on the testicle, heat dysregulation and oxygen deprivation are commonly encountered in varicoceles and can lead to impaired testicular sperm production.
In addition to these direct effects on sperm production, large varicoceles are also associated with impaired testosterone production and this can also lead to infertility.
It is important to note that experimental designs in animal models failed to prove any of these theories except for heat injury which is now thought to be the most important factor that adversely affects sperm production in men with varicoceles.
Clinical Presentation of Varicocele
Most men with varicoceles present to the clinic with infertility issues as varicoceles are usually not large enough to be symptomatic. A careful analysis of the patient’s history can reveal scrotal pain and heaviness, both being symptoms known to be common in men with varicoceles.
Physical examination is essential to diagnose varicoceles. Palpation of the affected side can reveal a bag of worms structure. It is important to palpate the other side, as bilateral varicoceles on physical examination are common and occur in 80% of the cases. Men with bilateral varicoceles and infertility need both sides to be treated to improve sperm quality and production.
Additionally, men with varicoceles should undergo a semen analysis. A normal seminal analysis usually means that varicoceles are not the cause of infertility and it is not advisable to treat varicoceles in this group of patients.
Diagnostic Work-up for Varicocele
A physical examination revealing a bag of ‘worms’ associated with infertility is usually enough to make a diagnosis of varicoceles and indicates the need for surgical correction. Unfortunately, this is not possible in some patients. In patients without a clear clinical picture or whose varicoceles arise suddenly, advanced imaging studies are needed to confirm the diagnosis and exclude possible secondary causes such as a pelvic tumor.
Although varicocele diagnosis may be assisted with numerous methods (e.g., venography, radionuclide angiography, thermography, ultrasonography), the current standard of care is high-resolution color-flow Doppler ultrasonography. High-resolution real-time scrotal ultrasonography using a 7- to 10-MHz probe.
The best modality to visualize varicoceles is high-resolution color-flow Doppler ultrasonography. Color-flow Doppler ultrasonography defines the anatomic and physiologic aspects of varicoceles by using real-time ultrasonography and pulsed Doppler in the same scan. The color of the signal identifies the blood flow and direction within the varicocele. The characteristic reverse flow of varicoceles is confirmed by prolonged flow augmentation within a colored flow area; the flow changes color (i.e., reverses) on real-time imaging.
Additionally, ultrasonography of the scrotum usually shows a tubular lesion that increases in size when the patient does Valsalva maneuver.
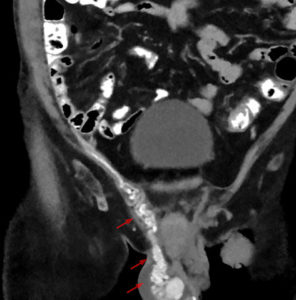
Image: “CT scan of a varicocele.” by Hellerhoff – Own work. License: CC BY-SA 3.0
Computed tomography scans can be used to visualize varicoceles but are not routinely used.
As part of routine workup for infertility in men, a seminal fluid analysis is usually indicated. Seminal fluid analysis can show impaired seminal qualities such as abnormal configurations, shapes or motility in addition to a decreased number of viable sperms, indicative of poor production. Testosterone may be low in men with varicoceles.
Treatment of Varicocele
The primary form of treatment for varicoceles is surgery. Because of the potential to cause significant testicular damage, evaluate the varicocele during the physical examination. The presence of a varicocele does not in itself mean surgical correction is necessary.
When varicoceles are symptomatic or associated with infertility and an abnormal seminal fluid analysis, the only possible treatment is surgical correction.
Several surgical and interventional radiological approaches exist for correction of varicoceles. Subinguinal microsurgical approaches are safe and effective for the treatment of symptomatic varicoceles associated with infertility. Patients with bilateral varicoceles should undergo bilateral surgical correction.
If a surgical approach is advised, care must be taken to preserve the testicular artery,otherwise, testicular necrosis can happen and infertility can become worse.
Other possible surgical approaches include inguinal and abdominal. Abdominal correction of varicoceles can be performed laparoscopically but is associated with a high recurrence rateand hydroceles can form after surgery. This procedure is preferred in pediatric populations.
The ultimate goals of varicocele repair should include occlusion of the offending varicosity, preservation of arterial flow to the testis, and minimization of patient discomfort and morbidity. Viable options for repair include radiographic obliteration and surgical repair of various approaches. The efficacy of the myriad techniques is nearly equivalent. Therefore, special attention must be paid to the morbidity of the individual procedure and the expertise of the operating surgeon.
More recently, percutaneous embolization has been used to treat varicoceles. Cannulation of the femoral vein is performed after which the internal spermatic vein is accessed. Varicoceles are then occluded by a balloon or any other occluding approach.
Percutaneous embolization is known to be the most effective method to preserve the testicular artery but still carries its own risks such as contrast allergy or thrombophlebitis.
Additionally, this approach usually needs an experienced interventionist radiologist and access to the internal spermatic vein is not always easy. Due to these limitations, the subingional or infrainguinal approaches remain the best options to treat varicoceles in symptomatic or infertile men.
Patients who are asymptomatic or who have varicoceles but whose seminal fluid analysis is normal should not be treated for varicoceles. Several studies have shown that such patients are unlikely to have future deterioration in their seminal quality if left untreated, hence no treatment is recommended.
Large symptomatic varicoceles that are not associated with infertility should be treated with the least invasive procedure, i.e. percutaneous embolization, to lower the risks associated with conventional surgery.
Complications
The prevalence of adverse effects following varicocele repair is remarkably low. Hydrocele or increased fluid around the testicles occurs in 2-5% of patients. Successful surgery often increases conception rates in infertile couples. The overall recurrence rate for varicoceles has been reported as high as 10%.
Injury to the testicular artery has been reported in 0.9% of microsurgical varicocele repairs. This incidence may be higher when optical magnification is not used for varicocele repair. Because the testis typically has additional arterial supplies from the vasal and cremasteric arteries, testicular atrophy is uncommon (5%) after division of the testicular artery. Smaller atrophic testes may be at greater risk for accidental testicular artery injury because of the smaller size of the artery in these cases.
In a patient in whom a varicocele is first identified during a vasectomy reversal, varicocelectomy at the time of the vasectomy reversal is controversial. Delaying the varicocelectomy preserves some venous return in these patients and avoids possible injury to the testicular artery. Consider varicocele repair 6 months later, after new vascular channels form.

Treatment of varicose veins . Thanks for sharing!
ResponderEliminarThank you for providing the information. I am learning so much now.
ResponderEliminarImportant Facts About Varicose Veins You Should Know