Allergies in Children — Types, Diagnosis and Treatment
Table of Contents
- Types of Hypersensitivity Reactions
- Overview of Urticaria, Angioedema, and Anaphylaxis
- Epidemiology of Urticaria, Angioedema and Food Allergies
- Pathophysiology of Urticaria, Angioedema and Food Allergies
- Clinical Presentation of Urticaria, Angioedema and Food Allergies
- Diagnostic Workup for Urticaria, Angioedema and Food Allergies
- Treatment of Urticaria, Angioedema and Food Allergies
- References
Types of Hypersensitivity Reactions
Type 1 hypersensitivity reactions
Requires exposure to a protein that is large enough to serve as an antigen.
Initial exposure ⇒ Production of an antigen-specific IgE ⇒ IgE binds to mast cell ⇒ Subsequent exposure ⇒ Mast cell degranulation
Common causes of type 1 hypersensitivity reactions
Foods
- Food additives
- Legumes
- Tree nuts
- Seafood
- Eggs
- Dairy
- Shellfish
- Berries
Medications
- Penicillins
- Sulfas
- Salicylates
- Vaccines
- Anesthetics
Environmental
- Bee/wasp stings
- Temperature changes
- Exercise
- Latex
Overview of Urticaria, Angioedema, and Anaphylaxis
Urticaria
Urticaria or hives are well-circumscribed areas of raised and erythematous skin due to edema involving the dermis and epidermis. The lesions are usually very pruritic. For diagnosing urticaria if it’s acute, recurrent or chronic, some information is necessary, such as the history of previous rash duration and itching duration of rash and itching.
Angioedema
Angioedema is a more severe form of urticaria where there is an extension of the edema into the subcutaneous tissue. Angioedema is therefore characterized by a deep swelling within the subcutaneous that is less discrete.
These two conditions can be considered as on the spectrum of allergies in children. Food allergies are immune-mediated responses that are triggered by certain foods. The allergic reaction is usually due to a certain protein within the food. Some common products that are known to be associated with food allergies are eggs, milk, peanuts, fish, and wheat.
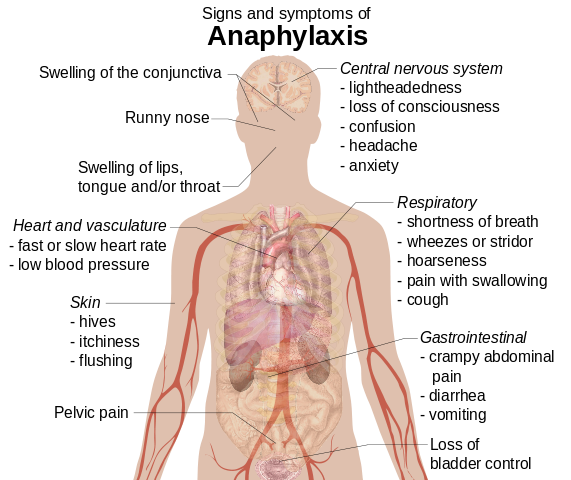
Anaphylaxis
Dermatologic
- Hives
- Itching
- Angioedema
Respiratory
- Shortness of breath
- Wheezing
- Throat swelling
Cardiac
- Tachycardia
- Hypotension
Epidemiology of Urticaria, Angioedema and Food Allergies
Urticaria
Urticaria can be classified as acute (< 6 weeks’ duration) or chronic. Acute urticaria has an estimated incidence of 15—20 % in children in a lifetime, making it a very common presentation to the emergency department.
Chronic urticaria has an incidence of 3 % over the children’s lifetime. While acute urticaria has a similar incidence in men and women, chronic urticaria is considerably more common in women. Chronic urticaria is rarely seen in children.
Angioedema
Image: “Angioedema2013” by James Heilman, MD. License: CC BY-SA 3.0
Angioedema associated with urticaria has been reported in up to half of the cases of urticaria. Hereditary forms of angioedema exist and collectively they affect 1 in 10,000 to 50,000. Hereditary angioedema type 1 is reported in approximately 5,000 to 25,000 in patients from the United States. Other forms of acquired angioedema are very rare and only a small number of cases have been reported in the literature.
Urticaria-related angioedema has been reported in children and adults and is commonly seen in both sexes without any significant differences. Hereditary angioedema is an autosomal dominant disorder without any sex predominance and is very rarely seen in children.
Food allergies
The prevalence of food allergies depends on the methodology of the researcher. When the methodology is mainly based on questionnaires and inquiries about the individual and his or her family members, the prevalence can be as high as 30 % of the population. On the other hand, when more accurate methods are used to confirm the food allergy, such as an oral food challenge, the prevalence is reported to be only 1 to 10.8 %. Boys are more likely to have food allergies. Food allergies are more common in infants compared to older children.
Diagnosis
Reactions related to food allergies are tingling or itchy sensations in the mouth, swelling of the face, lips, tongue, and throat or any other parts of the body certainly. Wheezing of the chest and nasal congestion, or any sort of difficulty in breathing, are symptoms of an allergic reaction to food. Pain in the abdomen, diarrhea, vomiting, dizziness, lightheadedness or fainting might prevail.
Pathophysiology of Urticaria, Angioedema and Food Allergies
Urticaria
Image: “Urticaria on feet” by Verysmallkisses. License: CC BY-SA 3.0
Urticaria is usually caused by an allergic reaction to an antigen which might be a protein from a food source. Type 1 allergic reactions involving the immunoglobulin E are believed to be responsible for a significant number of urticaria cases. Mast cells and basophils are activated and they release histamine, bradykinin, leukotriene C4 and prostaglandin D2. The result of the release of these mediators is the extravasation of plasma and fluid into the dermis and the development of circumscribed areas of edema or hives. Other forms of urticaria can be caused by type 2 allergic response mediated by cytotoxic T cells. Patients with systemic lupus erythematosus can develop urticaria due to a type 3 immune-complex response. Viral and bacterial infections, in addition to blood transfusion, have been associated with complement-mediated urticaria.
Angioedema
Urticaria-related angioedema has the same pathophysiology of simple urticaria but with the involvement of deeper skin layers such as the subcutaneous tissue. Patients with hereditary angioedema might have persistent activation of complement factor 1 which results in the activation of the complement cascade. This is believed to be associated with a kinin-like molecule that can also cause extravasation of fluid and edema within the subcutaneous. Acquired cases of angioedema might be an extremely rare complication to lymphomas.
Food allergies
Food allergies are caused by immunoglobulin E antibody-mediated responses, or by T cell-mediated responses. Patients with a pre-existing history of asthma or a previous history of anaphylaxis are at the highest risk of developing a fatal food-induced anaphylactic reaction.
Clinical Presentation of Urticaria, Angioedema and Food Allergies
Urticaria
Patients with urticaria usually present with skin wheals that are red in color, well-circumscribed, and very itchy. These lesions come and go rapidly. In some cases, the cause of the urticaria can be identified, such as the ingestion of a certain food the patient is known to be allergic to, exposure to some plants in the wild, or a previous history of systemic lupus erythematosus.
Angioedema
Image: “Allergic angioedema. Note that this child is unable to open his eyes due to swelling.” By James Heilman, MD. License: CC BY-SA 3.0
Patients with urticaria-related angioedema have a very similar presentation to simple urticaria but with more diffuse swelling that is localized deeper in the skin. The family history of angioedema might be positive in the hereditary forms of the disease. Patients might present with stridor and difficulty breathing due to the involvement of the throat. The most common trigger of angioedema is trauma, especially with dental procedures. Emotional stress has been also described as a possible cause of an episode of angioedema in some patients.
Food allergies
Patients with food allergies can present with urticaria or angioedema. Other possible presentations include stridor, cough, wheezing, nausea, vomiting, and ocular injection with conjunctival edema. Patients can also develop cardiovascular collapse and can go into an anaphylactic shock which might be fatal if not recognized early enough.
Diagnostic Workup for Urticaria, Angioedema and Food Allergies
The diagnosis of these conditions is highly dependent on clinical history taking and physical examination skills. Patients might have an elevated erythrocyte sedimentation rate when they have chronic urticaria. Patients with acute urticaria rarely undergo any imaging, laboratory or biopsy studies of the lesions.
Urticaria
Patients with severe urticaria or with angioedema should undergo an immunoglobulin E antibody skin test. This is usually helpful in patients with a documented history of possible food, drug or animal allergies.
Angioedema
Patients with angioedema might have a persistently activated C1 level. C1 inhibitor might be reduced in cases of acquired angioedema. C-reactive protein, erythrocyte sedimentation rate, and antinuclear antibody testing are indicated for cases of urticaria-related angioedema in patients with a history suggestive of systemic lupus erythematosus.
Patients with hereditary angioedema type 1 usually have low levels of C1 inhibitor; always have low levels of C4 and normal levels of C1 and C3. On the other hand, patients with hereditary angioedema type 2 might have normal or even elevated levels of C1 inhibitor. Patients with hereditary angioedema type 3 are always females and they have a normal complement profile. Those with acquired angioedema usually have low C1 inhibitor and C4 levels.
Food allergies
Patients with a suspected food allergy might undergo immunoglobulin E antibody testing. Patients with food allergies might have normal or elevated levels of immunoglobulin E and eosinophils in the serum. The only diagnostic test for food allergies is following an elimination diet. The elimination of the most common foods, followed by the introduction of one food at a time, is a common method to identify what is the most likely food allergy the patient has.
Treatment of Urticaria, Angioedema and Food Allergies
Urticaria
Patients with acute urticaria without any life-threatening symptoms or signs should be closely monitored until they reach the hospital. Those with a life-threatening anaphylactic reaction should receive intramuscular epinephrine as soon as possible. Patients with a wheezy chest should receive prehospital albuterol. Newer histamine receptor 1 blockers, such as loratadine, fexofenadine, and cetirizine are first-line therapies for the management of acute urticaria. Patients with severe urticaria that is not responsive to histamine receptor blockers should receive oral corticosteroids for a short period. Prednisone, 1 mg/kg/d, for five days is recommended for children with severe urticaria.
Angioedema
Patients with hereditary forms of angioedema might benefit from the elevation of C1 inhibitor levels by using a C1 inhibitor concentrate before undergoing a surgery. Once a patient develops an acute attack of angioedema, treatment should be based on the alleviation of the symptomatology. Berinert, which is a C1 esterase inhibitor, has been approved for the treatment of abdominal, facial, and laryngeal hereditary angioedema episodes in children. Other possible treatments for acute attacks of hereditary angioedema include the C1 esterase inhibitor Ruconest and Ecallantide which inhibits the release of bradykinin by inhibiting plasma kallikrein activity.
Food allergies
The treatment of a patient suspected to have a food allergy starts during the elimination diet for the diagnosis of the condition. Patients who have food allergies should wear bracelets or any other warning sign, especially when dining outside. It should be noted to them that open buffets carry an especially high risk of accidental ingestion of a food allergen and caution should be followed when they are at such events. Injectable epinephrine should be available to the patient and the patient should learn to take the epinephrine pen with them whenever they go out so that anaphylactic food reactions can be always treated early and promptly. Unfortunately, there are no known curative therapies for food allergies. Luckily, though, most children become tolerant to the food that is causing the allergic reaction or can outgrow their allergies.




Comentários
Enviar um comentário