Genital Development and Sexual Differentiation
Table of Contents
At the beginning of the embryonic development, the embryo does not have any specific gender. The development of the male and female embryo is identical in the first seven weeks, although the gender is usually already determined at the chromosomal level since fertilization. Which gender the embryo is going to have and, consequently, which genitals are to develop depends solely on the existence of a Y-chromosome.
Psychological gender identity is to be distinguished from anatomical development. The two generally correspond with each other, however, malformations during genital development can have an impact on them.
Development of the Gonads
In the fifth week, sexually indifferent gonads start to develop. The onset of the gonadal anlage is identical in both genders. Medially of the mesonephros, the urogenital fold forms out of proliferating coelom epithelium and adjacent mesenchyme.
At the end of the fifth week, the primordial germ cells or primordial gametes migrate out of the endodermal wall of the yolk sac. by means of amoeboid movements, they pass the hindgut and finally reach the urogenital folds. From this point on, they are referred to as gonadal ridges. Gender-specific gonadal development begins at around week seven.
Male Gonad Development: Development of the Testicles
If the embryonic chromosome set contains a Y-chromosome, further development of the gonadal anlage forms the testicle. The testis-determining factor (TDF), a transcription factor, is responsible for this. This is encoded by the SRY-gene (the sex-determining region of the Y-chromosome) on the Y-chromosome.
Initially, the so-called primary sex cords, belonging to the coelom epithelium, grow into the mesenchyme, going deep into the marrow and losing contact with the surface. Here within the marrow, they condense, branch, and are surrounded by a connective tissue capsule, the tunica albuginea. The following primary sex cords form:
- convoluted seminiferous tubules
- straight seminiferous tubules
- rete testis
At first, the seminiferous tubules do not have a lumen. However, the septum of the tubules contains Sertoli cells, which consisting of germinal epithelium, next to the immigrated primordial germ cells. The Sertoli cells inhibit the germ cells, now called spermatogonia, from entering the prophase of meiosis. They produce the so-called anti-Müllerian hormone (AMH), a glycoprotein, which influences the development of the genital ducts.
Furthermore, this is where the testosterone-producing Leydig cells are found. These are intermediate cells, which have developed from mesenchyme and are of essential importance in the further development of genitals, due to their ability to produce testosterone. With the onset of puberty and the further development of the germ cells, the tubules are canalized.
When the mesonephros regresses, parts of its tubules remain. These tubules are referred to as efferent ducts of the epididymis and are connected to the rete testis. As when the mesonephros produces urine, they have access to the mesonephric duct or Wolffian duct, which transforms into the epididymal duct.
Development of the Female Gonads: Development of the Ovary
The development of ovaries is usually slower than the development of testicles. Similar to the development of testicles, it begins with the inward growth of primary sex cords from the germinal epithelium into the mesenchyme. Just as with the development of testicles, the rete ovarii form, which usually regress completely. Also, a tunica albuginea is formed in the ovary, but this is significantly thinner than in the testicle.
In the 12th week, additional, so-called secondary sex cords start to grow. However, they do not grow as deeply into the mesenchyme and separate the cortical from the medullary area. The oogonia, the germinal cells that have immigrated, proliferate greatly within this cortex.
In the 16th week, the sex cords begin to lose their coherence and form cell clusters, which surround the individual oogonia as flat follicular epithelium cells. The oogonia have been developing into primary oocytes since the 13th week. The complex formed from an oocyte and the surrounding layer of follicular epithelium is called a primordial follicle.
During the prenatal period, numerous primordial follicles form. However, a lot of these follicles regress before birth. At birth, roughly two million oocytes are present in the ovary. Postnatally,no more oocytes are created. The oocytes are kept in the diplotene of the prophase until puberty.
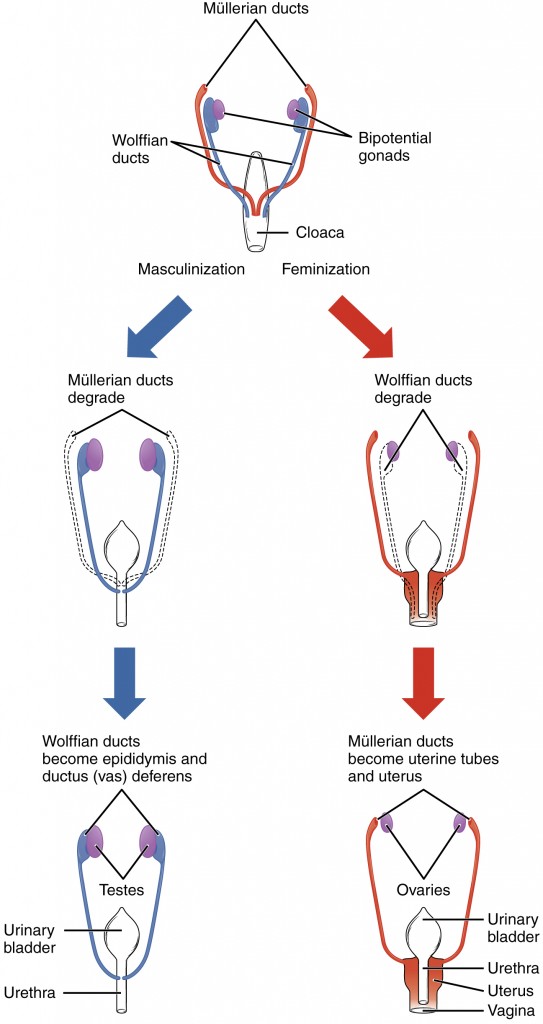
Development of the Genital Ducts
Initially, the development of the genital duct likewise exhibits a sexually indifferent stage. During this stage, the Mullerian ducts or paramesonephric ducts develop out of the epithelium laterally to the Wolffian ducts. At the end of the seventh week, they fuse caudally to form the utero-vaginal canal, and are connected to the dorsal wall of the urogenital sinus. This is where the so-called sinus tubercle or Mullerian tubercle develops. The influence of testosterone, emanating from the Leydig cells and the anti-Mullerian hormone emanating from the Sertoli cells, is crucial for further gender-specific development.
Development of the Male Genital Ducts
The production of testosterone induces the formation of male genital ducts. The following structures develop from the mesonephric duct:
- the epididymal duct: from the proximal sections of the Wolffian duct
- the deferent duct: from the distal sections of the Wolffian duct
- the seminal vesicle: from epithelial budding, directly in front of the entrance to the cloaca
- the ejaculatory duct: from the section between the junction of the seminal vesicle and the urethra
The epididymal duct is the convoluted duct system of the epididymis, which is surrounded by mesenchyme and is located at the cranial pole of the testicle. The efferent ducts lead to the epididymal duct. The distal section, which becomes the deferent duct, is surrounded by a layer of smooth muscles.
The prostate develops out of the epithelium of the urethra by growing into the attached mesenchyme. This also forms the smooth muscles of the prostate. The bulbourethral glands, or Cowper’s glands, develop in the same way; they are epithelial buddings of the urethra, which grow into the surrounding mesenchyme.
Under the influence of anti-Mullerian hormone, the Mullerian ducts regress almost completely. Frequent remains are:
- appendix testis: cranial remnant of the Mullerian duct at the testicle
- prostatic utricle: small remnant of the vagina in the prostatic part of the urethra
- seminal colliculus: rudimentary equivalent to the Mullerian tubercle
Although in men the mesonephric duct develops completely, some remnants may remain. This includes the appendix of the epididymis from the cranial end of the duct, and the paradidymis, the caudal remains of the mesonephric tubules, which have not developed into efferent ducts.
Development of the Female Genital Ducts
The development of the female genital ducts can be traced back to the absence of the Y-chromosome and, hence, to the absence of testosterone and the anti-Mullerian hormone. Further development of the Mullerian ducts occurs, along with regression of the mesonephric ducts, leading to the formation of the female genital ducts.
The unfused proximal sections of the Mullerian ducts form the fallopian tube, whose proximal section opens into the abdominal cavity. With the onset of puberty, ovulated oocytes are accommodated here.
The fused caudal part of the Mullerian ducts becomes the utero-vaginal canal, which goes on to form the upper part of the vagina and the uterus. The utero-vaginal canal leads to the urogenital sinus at the Mullerian tubercle. This is where two epithelial buds or the sinu-vaginal cusp of the endoderm of the urogenital sinus grow together into a solid, completely closed vaginal plate. This separates the utero-vaginal canal from the urogenital sinus.
The subsequent vagina is formed by means of the development of a lumen via degeneration of numerous cells in the center. The vagina is separated from the urogenital sinus by a thin hymen.
When the Mullerian ducts fuse, they drag their peritoneal attachment with them. A peritoneal fold, referred to as the broad ligament of the uterus, is thus formed. Between the two sheets of tissue belonging to this structure, the so-called parametrium is found, which is made of mesenchyme. Two important pouches form at this location and are bordered by peritoneum:
- the recto-uterine pouch (pouch of Douglas)
- the vesico-uterine pouch
The female embryo also develops glands from epithelial buds, which grow into the mesenchyme. These are the urethral glands, the equivalent of the prostate and the associated paraurethral ducts, or Skene’s ducts, and the major vestibular glands, or glands of Bartholin, which correspond to the bulbourethral glands.
During regression of the mesonephric ducts, due to the absence of testosterone, some parts may remain, namely the appendix vesiculosa at the cranial end, the epoophoron with the remains of the mesonephric tubules in the mesovarium between the ovary and the fallopian tube, and the paroophoron with remains of the mesonephric tubules close to the uterus in the mesovarium. Gartner’s duct is a rudimentary equivalent of the deferent duct and the ejaculatory duct. Gartner’s duct cysts sometimes form here.
Rudimentary remains of the Mullerian duct are also sometimes seen in women. They develop at the cranial end, which is not employed by the fallopian tube. This vesicular structure is referred to as hydatid of Morgagni.
Development of the External Genitals
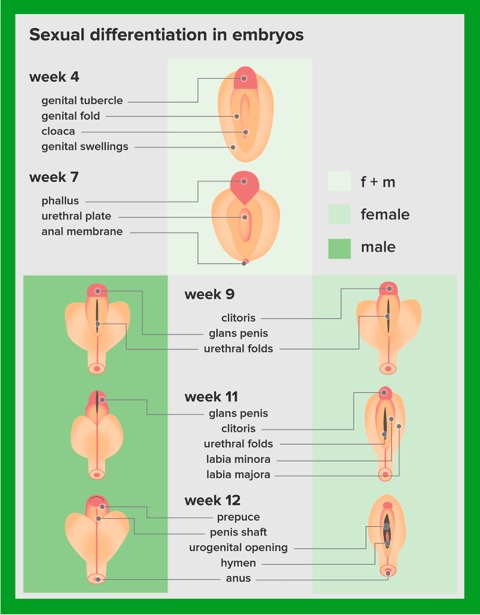
In a like manner, the development of the external genitals begins with a sexually indifferent phase. By the 12th week, differentiation of the two genders is complete. In both genders, the following structures develop during the indifferent phase:
- the genital tubercle: ventral to the cloacal membrane
- the genital or urethral folds: on both sides of the cloacal membrane
- the labioscrotal swelling: lateral to the genital folds
The urogenital membrane, which seals what will become the urogenital orifice, is found between the genital folds. It ruptures about one week after the urorectal septum has developed together with the cloacal membrane, and leaves the orifice open. In both genders, the genital tubercle initially grows in length, to become the phallus.
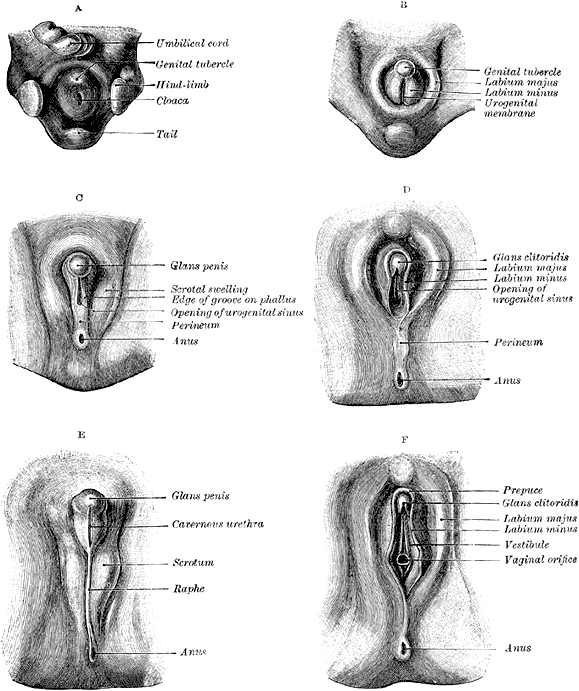
Development of the Male External Genitals
The development of the male external genitals can also be traced back to the influence of testosterone on gender. First of all, the phallus develops into a penis. After this, it drags with it the genital folds, which have not yet fused at the lower side. The resulting groove is called the urethral groove. At this point the urethra does not end at the tip of the penis but instead at its inferior surface.
The genital tubercle forms the glans penis at the tip of the penis. Out of the glans, ectodermal cells grow towards the urethra. Eventually, this cell cord becomes canalized, with the genital folds growing together on the lower surface, and the elongated urethra gaining its new orifice at the tip of the penis.
The cavernous bodies, as well as the spongy body originate from the mesenchyme. The foreskin or preputium develops by means of circular growth of the glans penis. It is therefore of ectodermal origin, and it covers the glans penis. By means of fusion, the labioscrotal swellings become the scrotum. This is divided by the scrotal septum. The descent of the testicles into the scrotum normally occurs before birth.
No satisfactory answer has been found as to why this so-called testicular descent occurs. It is believed that body temperature is too high to allow maturation of sperms, leading to the testicles being relocated to the outside. During the testicular descent, the testicles take along all the layers of the abdomen, which explains the complexity of the testicular layers. The gubernaculum testis, a cord made of connective tissue situated between the testicle and the scrotum, guides the descent.
Development of the Female External Genitals
No complete explanation has been found as to what leads to the formation of the female genitals. Estrogen may be responsible. In a female fetus, the phallus does not grow any longer and remains as the clitoris. The genital folds fuse only in their posterior section to form the frenulum of labia pudenda. They become the labia minora.
The labioscrotal swellings fuse at the front and back, where they form the anterior and posterior commissure of the labia and the mons pubis. They become the labia majora. The ovaries also make a descent, which is guided by the gubernaculum. This descent, however, finishes within the lesser pelvis. The gubernaculum becomes:
- the suspensory ligament of ovary
- the proper ovarian ligament
- the round ligament of uterus
Pathological Genital Development
Malformations of the genitals may either have a chromosomal basis or may occur during various phases of development. The consequences may consist of small changes or, in rare cases, complete agenesis of the external genitals. The most important malformations are described below.
Klinefelter-Syndrome: XXY
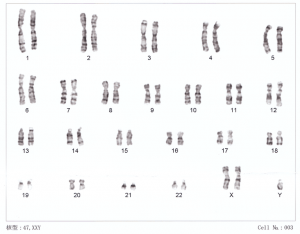
In Klinefelter-Syndrome, the developing organism has two X and one Y chromosome. Those affected have a male phenotype, but exhibit, for example, female breast growth and are sterile due to the incorrect development of testicles.
Turner Syndrome: X0
People affected with Turner syndrome have only one X chromosome, so that their genotype is described as X0. The phenotype is female. However, the female gonads are incapable of functioning. Typical indicators are dwarfism, pterygium colli, low hairline, and sterility.
True Hermaphroditism
In this case, both XX and XY sets of chromosomes and XX/XY mosaics can be present, with the first scenario being the most common. Humans who have this set of chromosomes developboth ovaries and testicles. Sometimes a condition called ovotestis is present, whereby both ovarian and testicular features occur in the same gonad . The phenotype and the external genitals can be female, male, or intersexual. True hermaphrodites often have a female physiological identity.
Pseudohermaphroditism
Both masculine and feminine forms exist. The feminine form describes people with an XX-set of chromosomes, and whose adrenal gland produces too much testosterone. Despite having normally-developed ovaries, these women can develop male external genitals in different manifestations. On the other hand, the masculine form relates to people with a XY set of chromosomes who produce too little AMH or testosterone. This results in varying degrees of insufficient development of the testicles and the external genitals.
Hypospadias and Epispadias
If the genital folds do not fuse around the urethra in the development of the penis, a urethral orifice at the lower surface of the penis results. This is referred to as hypospadias. Malformations in mesenchyme and ectoderm can lead to a dorsal location of the genital tubercle, with the urethra terminating at the dorsal side of the penis. This is referred to as epispadias.

Different types of hypospadias
Cryptorchidism
This means undescended testicles, which can in principle occur at any point during the descent of the testicle. One frequent ectopic location for a testicle is in the inguinal canal. Until shortly before birth, this does not constitute a pathological state! Only after completion of the first year of life does this state impair further development and result in sterility.
Androgen Insensitivity
Also referred to as testicular feminization, androgen insensitivity is the absence or lack of androgen receptors. Thus, the female genital ducts regress, whereas the male genital ducts do not develop correctly. The clitoris and labia majora develop as external genitals, resulting in an inconspicuous female phenotype, despite the presence of XY chromosomes. In puberty, however, menarche does not occur. Despite the presence of the Y-chromosome, the physiological identity of these individuals is female.
Uterus Duplex and Uterus Bicornis
If the two Mullerian ducts do not fuse or do not completely fuse, a more or less separated utero-vaginal canal is present. Uterus duplex refers to the formation of a double uterus with one or two vaginas. If only the upper part of the uterus is doubled, it is termed as uterus bicornis.
Review Questions
The answers can be found below the references.
1. Which is statements below is correct? The genital tubercle…
- …lies dorsal to the cloacal membrane.
- …later becomes the labia majora.
- …is a pathological structure.
- …becomes the scrotum.
- …becomes the phallus in both genders.
2. The epididymal duct…
- …develops from the proximal section of the Wolffian duct.
- …is situated in the testicle.
- …develops from the distal section of the Wolffian duct.
- …is a remnant of the mesonephric tubules.
- …develops from the Mullerian duct.
3. Which of the statements below is false?
- The gubernaculum guides the descent of the testicle.
- The body temperature is probably too high for maturation of sperm.
- The suspensory ligament of the ovary develops from the epoophoron.
- The expression of sexually indifferent gonads refers to the equivalent development of the gonads in the beginning of embryonic development.
- The primordial germ cells migrate into the gonads across the intestine.

Comentários
Enviar um comentário