Dysmenorrhea in Adolescents — Definition and Treatment
Table of Contents
Overview
The term dysmenorrhea is derived from three Greek words which literally mean bothersome monthly flow. Therefore, dysmenorrhea can be defined as a bothersome or painful monthly menstrual flow. Dysmenorrhea is more common during mid and late adolescence. Dysmenorrhea can be subdivided into primary and secondary based on whether a pelvic pathology can be identified as the cause with the former being more common than the latter among adolescents.
Epidemiology of Dysmenorrhea in Adolescents
Dysmenorrhea is a very common problem in adolescent girls and is the number one gynecological cause of recurrent short-term school absenteeism in this age group. Most cases of dysmenorrhea in adolescents are reported during mid and late adolescence when ovulatory menstrual cycles become established. Dysmenorrhea is less common in early adolescent years when most of the menstrual cycles are anovulatory.
The most commonly identified risk factors for primary dysmenorrhea in adolescents are early menarche and increased duration and amount of menstrual flow. Cigarette smoking is another important risk factor for primary dysmenorrhea in adolescents.
The most common cause of secondary dysmenorrhea in adolescents is endometriosis. The family history of endometriosis or bleeding disorders in an adolescent with dysmenorrhea points towards secondary dysmenorrhea rather than primary dysmenorrhea.
Pathophysiology of Dysmenorrhea in Adolescents
The pathologic process of primary dysmenorrhea is different from that of secondary dysmenorrhea which arises from pelvic or gynecological etiologies.
Primary dysmenorrhea usually happens in adolescents with established ovulatory cycles and is very unlikely to happen with anovulatory cycles. When ovulation happens, omega-6 fatty acids start building up in the phospholipids of the cell membranes of the uterus.
Progesterone withdrawal right before menstruation is a normal physiologic occurrence and is responsible for the release of omega-6 fatty acids, especially arachidonic acid. The release of these fatty acids triggers the activation of prostaglandins and leukotrienes in the uterine wall which initiates an inflammatory response. This inflammatory response is responsible for the localized symptoms of dysmenorrhea such as abdominal pain and cramps. Systemic symptoms such as nausea and vomiting in addition to a headache are also common.
Prostaglandin F2-alpha activity was found to be twice as high in adolescents with dysmenorrhea compared to those who do not have any pain during menstruation. Additionally, the severity of the symptoms of dysmenorrhea was found to be positively correlated with the level of this type of prostaglandin.
Additionally, girls with primary dysmenorrhea were found to have higher levels of serum vasopressin, another potent inducer of uterine contraction during menstruation.Continued contraction of the uterine muscles leads to oxygen deprivation that induces severe cramps/ pelvic pains.
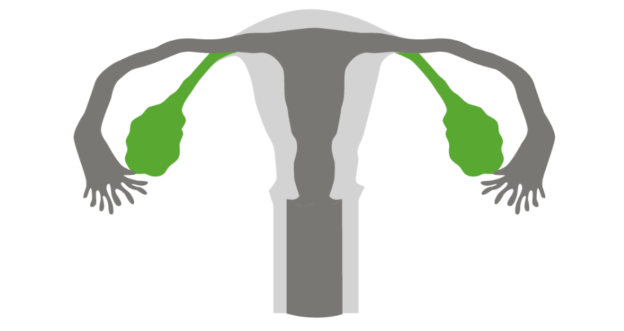
The most common cause of secondary dysmenorrhea in adolescents is endometriosis. Endometriosis is characterized by the presence and growth of uterine glands outside the uterine cavity. The most common sites for endometriosis implantation are the pelvic organs such as the ovaries or the rectum. The most probable cause of endometriosis is retrograde menstruation.
Estrogen receptors are abundant in endometriotic tissues. Additionally, aromatase is usually overly expressed in endometriotic tissues but not in the normal endometrium. Endometriotic tissues also express interleukin-1 and tumor necrosis factor alpha, both of which can influence the establishment and proliferation of the ectopic endometrial tissues.
Cycloxygenase-2 (COX-2) levels are also elevated in the endometriotic tissues compared to the normal endometrium. COX-2 is responsible for the synthesis of prostaglandin F2-alpha, which is believed to be related to the pathophysiology of dysmenorrhea. Additionally, the release of prostaglandin E2 is increased in patients with endometriosis. The accumulation of prostaglandins is responsible for cyclic and non-cyclic pelvic pain in patients with endometriosis. It is important to mention that the severity of the symptoms of endometriosis does not correlate well with the extent of the disease.
Another important cause of dysmenorrhea that is more specific to the adolescent age group is the presence of a Mullerian duct anomaly. Didelphic uterus with unilateral obstruction, imperforate hemivagina and the presence of a vaginal septum are all possible anatomical anomalies that can lead to dysmenorrhea during the early adolescent years. Sexually active adolescents might have an ectopic pregnancy which might present with acute abdominal pain and vaginal bleeding. This acute presentation should be differentiated from the recurrent abdominal cramps that are characteristic of true dysmenorrhea.
Clinical Presentation of Dysmenorrhea in Adolescents
The presentation of primary dysmenorrhea is characterized by low abdominal cramping in an adolescent. Other associated symptoms include headaches, nausea and vomiting. The symptoms are cyclic and usually start with the onset of the menstrual flow. The symptoms of primary dysmenorrhea usually last for one to two days.
On the other hand, the symptoms of secondary dysmenorrhea depend on the cause and the site of the pelvic abnormality. For instance, adolescents with pelvic endometriosis usually present with chronic pelvic pain, mid-cycle pain, dyspareunia and metrorrhagia. Pelvic endometriosis-associated dysmenorrhea is usually both cyclic and acyclic in the same patient. Familial history of secondary dysmenorrhea is commonly identified.
Sexually active adolescents who present with chronic pelvic pain, dysuria and dyspareunia might have a chronic pelvic inflammatory disease. A pelvic examination might reveal cervical motion tenderness or cervical fragility, both considered as specific signs of pelvic inflammatory disease. Additionally, the possibility of an ectopic pregnancy should be excluded in any sexually active adolescent who presents with acute abdominal cramping pain and vaginal bleeding.
Diagnostic Workup for Dysmenorrhea in Adolescents
A proper history and physical examination are usually sufficient in establishing the diagnosis of dysmenorrhea, but there are few points to take into consideration. The differentiation between primary and secondary dysmenorrhea is essential as the treatment might differ.
The first step in the diagnostic workup of dysmenorrhea is to exclude acute and life-threatening conditions such as an ectopic pregnancy when appropriate. Therefore, pregnancy should be excluded by ultrasonography and an appropriate serum or urinary beta-human chorionic globulin (beta-HCG) test. The most common site for an ectopic pregnancy is the fallopian tube, hence the visualization of the tubes by ultrasonography can exclude ectopic pregnancy as the cause of acute abdominal pain in a patient with vaginal bleeding.
The next step would be to understand whether the dysmenorrhea is purely cyclic, acyclic or both. Purely cyclic dysmenorrhea is very likely to be a primary condition, and it is unlikely to uncover any pelvic pathology. Purely acyclic chronic pelvic pain might be caused by a chronic pelvic inflammatory disease. Patients with both cyclic and acyclic dysmenorrhea most likely have endometriosis. Pelvic ultrasonography is required to confirm the diagnosis of endometriosis.
TThe most common sites of endometrial tissue location include the ovaries and the cul-de-sac which can be easily visualized and examined with a proper pelvic ultrasonographic scan. Ultrasonography can also help in the exclusion of anatomical anomalies of the uterine cavity or the Mullerian ducts which contribute to a considerable number of dysmenorrhea cases in young adolescents.
Treatment of Dysmenorrhea in Adolescents
The management of primary dysmenorrhea in adolescents can be classified into non-pharmacologic and pharmacologic treatment. Herbal preparations and acupuncture might relieve some of the symptoms of dysmenorrhea in few cases. Additionally, increasing the intake of fish or other sources rich in omega-3 fatty acids tend to decrease the symptoms of dysmenorrhea in some patients. Most cases of primary dysmenorrhea, however, need some sort of a pharmacologic intervention for adequate symptomatic relief.
The most commonly used medications for primary dysmenorrhea in adolescents are ibuprofen, naproxen, mefenamic acid and celecoxib. These four medications belong to the non-steroidal anti-inflammatory drugs family except for celecoxib which is a specific COX-2 inhibitor. The efficacy, safety and tolerability of the four medications are similar.
Oral combined contraceptive pills are also considered as first-line therapy for the management of primary dysmenorrhea in adolescents. Seasonale, Seasonique and Lybrel have been all used in adolescents with dysmenorrhea and showed excellent results. The active ingredients in these pills are levonorgestrel and ethynyl estradiol.
Adolescents who do not respond to the previously mentioned pharmacologic interventions are more likely to have secondary dysmenorrhea, and further diagnostic workup is indicated to exclude less common causes of dysmenorrhea. Laparoscopy is indicated after six months of conservative management of dysmenorrhea to exclude the possibility of endometriosis.
If endometriosis implants can be visualized by laparoscopy, they should be removed or obliterated by laser vaporization. Low-dose monophasic oral contraceptives can be also administered to adolescents with endometriosis in a non-cyclic fashion. Medical management of endometriosis also includes the administration of nafarelin and leuprolide, both are gonadotropin receptor agonists. GnRH agonists should be avoided whenever possible in young adolescent girls. Aromatase inhibitors can be also used in adolescents with endometriosis-associated dysmenorrhea, but they should be combined with a progestin to prevent the development of ovarian folliculogenesis.
Comentários
Enviar um comentário