Coronary Artery Disease (CAD, Atherosclerotic Heart Disease) — Risk Factors and Prevention
Table of Contents
- Definition of Coronary Artery Disease
- Epidemiology of Coronary Artery Disease
- Etiology of Coronary Artery Disease
- Classification of Coronary Artery Disease
- Pathophysiology of Coronary Artery Disease
- Symptoms and Clinical Diagnosis of Coronary Artery Disease
- ST-segment Elevation Myocardial Infarction (STEMI)
- Progression and Special Forms of Coronary Artery Disease
- Diagnostics of Coronary Artery Disease
- Pathology of Coronary Artery Disease
- Differential Diagnosis of Coronary Artery Disease
- Therapy of Coronary Artery Disease
- Prevention of Coronary Artery Disease
- Prognosis of Coronary Artery Disease
- Review Questions
- References
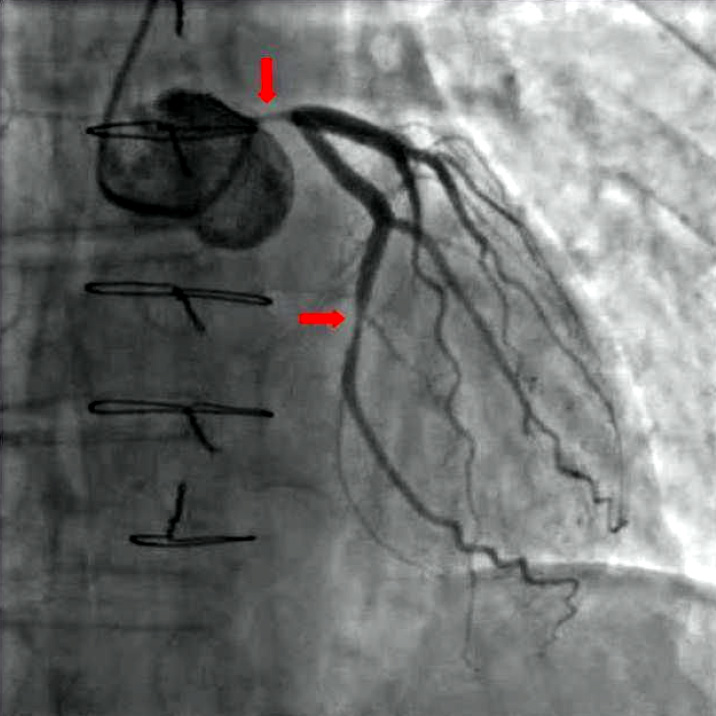
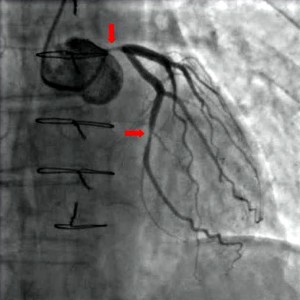
Image: “Coronary angiography of a critical sub-occlusion of the common trunk of the left coronary artery and the circumflex artery. (See arrows)” by Kuebi. License: CC BY 2.0
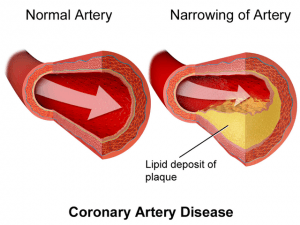
Definition of Coronary Artery Disease
Coronary artery disease is a term used to describe a wide range of clinical conditions in which there is imbalance between oxygen supply and the myocardial demands resulting in ischemia to a portion of the myocardium.
Coronary heart disease is the manifestation of atherosclerosis in the coronary arteries, so that the oxygen demand of the heart muscle cannot be sufficiently covered by the oxygen supply, because of stenotic coronary vessels. Thus, the myocardium becomes ischemic.
The most common cause of coronary heart disease is atherosclerosis of epicardial coronary arteries, resulting in partial or complete obstruction with subsequent inadequate perfusion of the myocardium supplied by the involved coronary artery.
Many risk factors have been involved in the pathophysiology of coronary heart disease. The most common are obesity, high-fat diet, insulin resistance, diabetes and smoking. Risk factor modifications delay the onset of the disease and its progression to later life.
Epidemiology of Coronary Artery Disease
Coronary artery disease is one of the leading causes of death worldwide. It is considered the most common, serious chronic illness in the United States, as more than 13 million patients are suffering from coronary artery disease. More than 6 million have angina pectoris, and more than 7 million have myocardial infarction. Because of the large increase in the prevalence of IHD worldwide, it’s likely to become the leading cause of death by 2020.
Coronary heart disease has an incidence rate of 0.6 % per year with an increase in the elderly. Men are affected more often than women. Together with its manifestations, it is the leading cause of death in industrialized countries, making up almost 20 % of all deaths.
The international MONICA study (Monitoring of Trends and Determinants of Cardiovascular Diseases) records causes and trends of coronary heart disease.
Etiology of Coronary Artery Disease
Causes and risk factors of coronary artery disease
Significant risk factors can be recognized for the occurrence of coronary heart disease. Among the main risk factors, in addition to an increase of LDL cholesterol or a decrease of HDL cholesterol, include arterial hypertension, diabetes mellitus, smoking as well as family historyand male gender.
Other risk factors include an unhealthy, atherosclerosis favoring nutrition, severe obesity and too little physical activity. Metabolic disorders, such as impaired glucose tolerance or lipid metabolism disorder, also favor the emergence of coronary heart disease.
In patients who suffer a heart attack at a younger age (< 30 years) other causes may play a role. These include familial lipid metabolism disorders as well as hypothyroidism and vasculitis. Coronary anomalies, antiphospholipid syndrome and hyperviscosity syndrome should also be excluded. During history taking, possible drug abuse should be inquired about.
Since myocardial ischemia develops most commonly as result of obstruction of one or more coronary arteries in the form of coronary atherosclerosis, a number of risk factors predispose to this condition.
Classification of Coronary Artery Disease
We differentiate between asymptomatic and symptomatic coronary heart disease. While the asymptomatic form is a silent ischemia, symptomatic coronary heart disease manifests in different ways. This can range from an unstable angina pectoris to acute coronary syndrome and from coronary heart muscle damage to cardiac arrhythmia and sudden cardiac death.
Pathophysiology of Coronary Artery Disease
If damage to the coronary arteries already exists, for example due to arterial hypertension, endothelium platelets attach themselves to the damaged site. They attract macrophages, among others, with help of mediators. If macrophages take up LDL cholesterol, they are incorporated as so-called foam cells into the vessel wall.
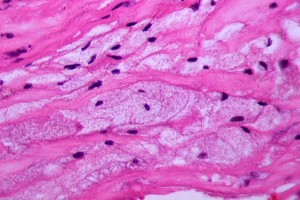
Image: “Foam cells in atherosclerotic plaque. Histology.” by Patho. License: CC BY-SA 3.0
Stenosis of the coronary arteries can lead to an insufficient supply of oxygen to the heart muscle tissue, starting with a narrowing of 50 % on exertion, because the oxygen demand increases by approximately fourfold on exertion.
The so-called coronary reserve, i.e., the difference between the minimum blood flow and the fourfold, increased, maximum blood flow during exercise, is so severely limited in patients with coronary heart disease, that often not even an increase of blood flow to two times the resting blood flow is possible. The result is coronary pain.
Angina occurs when there is imbalance between the oxygen supply and the myocardial demand, resulting in myocardial ischemia.
Myocardial oxygen demand
Four major factors determine the oxygen demand of the myocardium:
- Heart rate
- Systolic blood pressure (after load)
- Tension on myocardial wall (preload)
- Myocardial contractility.
Any clinical condition increasing one or more of these factors will also increase the myocardial oxygen demand and can result in ischemia, such as extreme tachycardia, hypertension, ventricular hypertrophy.
Myocardial oxygen supply
The capacity of the blood to carry oxygen to the myocardium is affected by different factors:
Hemoglobin and oxygen tension and the amount of extracted oxygen from hemoglobin to the tissue, and it is related to 2,3 diphosphoglycerate levels. Another factor is Coronary artery blood flow, which is affected by the following factors:
- Coronary artery diameter: Coronary atherosclerosis is the most frequent cause of narrowing and obstructing the coronary artery, and the clinical presentation differs according to the extent of obstruction.
- Coronary artery tone: Coronary vasospasm as in variant or Prinzmetal’s angina, reduces the oxygen supply without significant underlying artherosclerotic changes.
- Perfusion pressure: It’s determined by the pressure gradient from the aorta to the coronary artery.
- Heart rate: Coronary artery flow occurs mainly during diastole, therefore extreme tachycardia will decrease the duration of diastole, and thus will decrease the blood flow into the coronary arteries.
Any clinical condition affecting one or more of the above mentioned factors will reduce the myocardial oxygen supply and can result in ischemia.
Symptoms and Clinical Diagnosis of Coronary Artery Disease
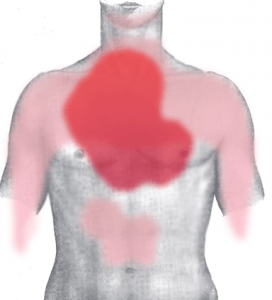
Image: “Pain in acute myocardial infarction (front),” by J. Heuser. License: CC BY-SA 3.0
The main symptom of coronary heart disease is angina pectoris, which can be divided into a stable and an unstable form.
The symptoms are often indicated as retrosternal painor pressure. Tightness in the chest is also typical. A radiating pain in the left (or right) arm, reaching up to the lower jaw and neck, is a common symptom.
Patients with coronary heart disease (IHD) can present with either:
Chronic artery disease (CAD), which most commonly presents as stable angina, or
Acute coronary syndromes (ACSs), which is a term that encompasses:
- Unstable Angina (UA)
- Myocardial infarction
- ST-segment Elevation Myocardial Infarction (STEMI)
- Non-ST-segment Elevation Myocardial Infarction (NSTEMI)
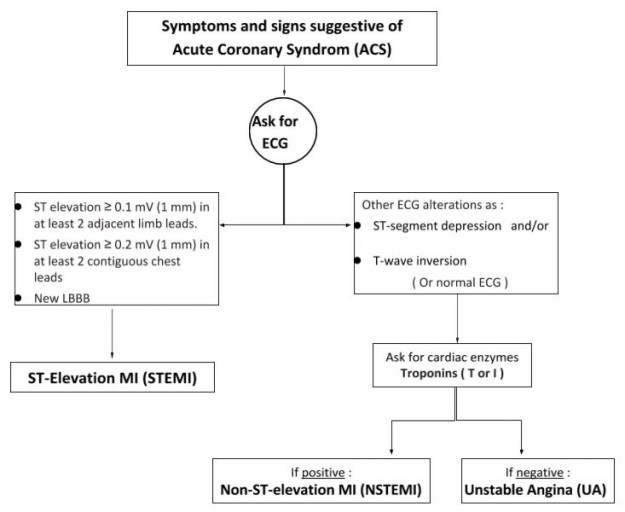
Acute Coronary Syndrome
ST-segment Elevation Myocardial Infarction (STEMI)
Diagnosis
Diagnosis of STEMI also depends on history, abnormalities on ECG and the cardiac biomarkers.
History
Chest pain is similar in character to stable angina pectoris, but more severe, lasts longer (usually > 20 minutes) and not fully relieved by rest or nitroglycerin.
Abnormalities on ECG
ST elevation, followed by T-wave inversion if no reperfusion was achieved, followed by Q-wave development over several hours. The ECG criteria for ST-elevation MI (a, b or c) are:
- ST elevation ≥ 0.1 mV (1 mm) in at least 2 leads of either:
- Inferior group: II, III, aVF
- Lateral group: I, aVL, V5, V6
- ST elevation ≥ 0.2 mV (1 mm) in at least 2 contiguous anterior leads (V1–V4)
- New LBBB.
Cardiac biomarkers
Troponin I and T are more specific than CK-MB cardiac enzymes. Normally, Troponin enzymes are not detectable in the blood of healthy individuals, but they are increased to levels more than 20 times higher than upper reference limit in myocardial infarction (MI).
Treatment
Management of patients with suspected ST-Elevation MI in the emergency department should focus on relieving the coronary pain, identification of candidates, urgent reperfusion therapy and avoiding the discharge of a patient with suspected STEMI.
- Patients should be immediately admitted in a hospital with ECG rhythm monitoring due to risk of sudden death.
- Take targeted history and examination.
- Intravenous access and blood sample for cardiac markers.
Immediate treatment:
- Aspirin: should be administered immediately.
- Sublingual glyceryl trinitrate, repeat if no effect in 5 min.
- Begin oxygen by nasal cannula or mask if hypoxia is present.
- Intravenous opiates (such as Morphine).
- Beta-Blocker (if no contraindication) for ongoing chest pain, hypertension, tachycardia.
Reperfusion therapy:
Primary percutaneous coronary intervention (primary PCI):
Primary PCI refers to angioplasty and/or stenting without preceding fibrinolysis. It is more effective and preferred than IV fibrinolysis, especially when:
- Diagnosis is in doubt;
- Cardiogenic shock is present;
- There is an increased risk of bleeding;
- Symptoms have been present for > 3 hours.
Fibrinolysis:
IV fibrinolysis is indicated if:
- Primary PCI is not available, or
- Delay to PCI would be > 1 hour longer than initiation of fibrinolysis.
Before starting fibrinolytic drugs, assess for contraindications:
- Prior intracranial bleeding;
- Intracranial malignancy or vascular malformation;
- coronary stroke or head trauma in previous 3 months;
- Aortic dissection;
- Active bleeding (with exception of menses);
- Internal bleeding in previous 4 weeks;
- Severe hypertension (systolic > 180 or diastolic > 110);
- Prolonged (> 10 min) CPR chest compressions;
- INR ≥ 2.0 on warfarin or known bleeding diathesis;
- Pregnancy.
Coronary angiography after fibrinolysis (rescue PCI) is indicated in case of:
- Failure of reperfusion (as evidenced by < 50 % resolution of ST segment elevation > 90 min after completion of fibrinolytic treatment);
- Spontaneous recurrent ischemia while in a hospital;
- High-risk features, e.g., extensive ST-segment elevation, signs of heart failure and hypotension (systolic blood pressure < 100 mmHg).
Progression and Special Forms of Coronary Artery Disease
Progressive forms of coronary artery disease
In addition to typical angina pectoris, with the retrosternal discomfort that is triggered by stress and gets better at rest, we have atypical angina pectoris, which involves only two of the three typical criteria.
Angina at rest describes a form, in which the symptoms occur at rest. There is also nocturnal angina, where complaints manifest only at night.
Special forms of coronary artery disease
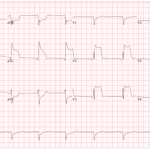
Image: “EKG of a patient with Prinzmetal’s Angina,” by Gogradgme. License: CC BY-SA 3.0
Silent myocardial ischemia can also be a form. Here, the typical symptoms are missing. It occurs frequently in diabetics (due to neuropathy), patients with renal insufficiency, women and elderly patients. The symptoms can be very nonspecific here. Dizziness and nausea, as well as shortness of breath and symptoms that radiate into the epigastrium, are often at the foreground.
Another special form is postinfarction angina which may occur within two weeks after a myocardial infarction.
Diagnostics of Coronary Artery Disease
History and laboratory diagnosis of coronary artery disease
In Lecturio ;) - For the diagnosis, a history that covers the symptoms and their time of onset, triggering factors and the presence of risk factors has to be explored first. In the physical examination, factors such as hypertension and obesity stand out, but auscultation can also detect an indication of heart disease.
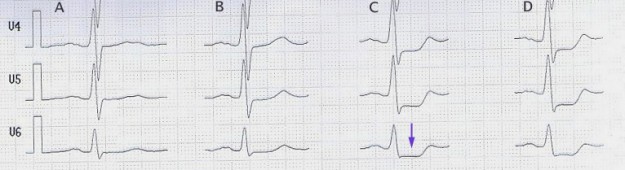
In the laboratory, markers such as CK, CK-MB, and troponins indicate myocardial damage, which, however, is not present in stable angina pectoris. Furthermore, an ECG can be taken at rest, which often remains unchanged, even with severe coronary heart disease. A stress testtypically shows a descending or horizontal ST depression of 0.1-0.2 mV.
Image: “Stress-ECG with ST-segment-depression (arrow) beginning at 100 W (column C),” by J. Heuser. License: CC BY-SA 3.0
A holter monitor can be useful as well if for example, the symptoms occur in everyday situations. A transthoracic echocardiography can exclude other causes of angina, such as aortic stenosis, and wall motion abnormalities can give an indication of a myocardial infarction.
Gold standard of diagnostics
Image: “Coronary angiography of a critical sub-occlusion of the common trunk of the left coronary artery and the circumflex artery (see arrows).” by Kuebi. License: CC BY-SA 2.0
The gold standard of diagnostics is coronary angiography with access via the femoral artery, the brachial artery or the radial artery, to determine the degree of stenosis of the coronary artery. Representations via a multislice spiral CT or dual-source CT or MR angiography are also possible.
To investigate stress-related ischemia, a stress echocardiography or stress MRI with dobutamine can be performed.
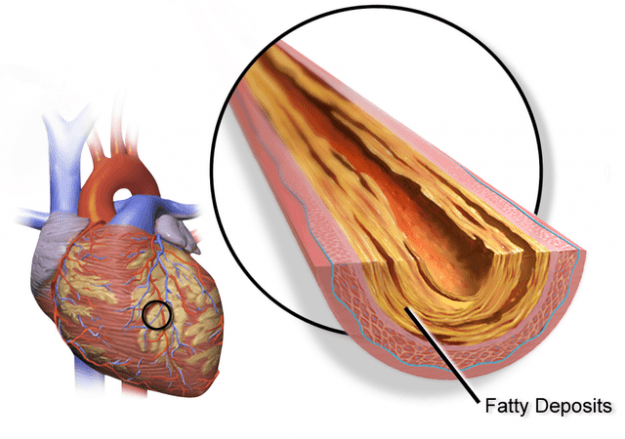
Pathology of Coronary Artery Disease
The pathology of coronary heart disease is primarily based on an increased resistance in the coronary arteries. These also include intracoronary additional factors such as cardiac disease or other increased O2 demands, for example during a fever, as well as a reduced amount of O2, among other things, in lung diseases.
The increased resistance of the coronary vessels can be explained by coronary artery stenosis due to atherosclerosis in 90 % of all cases.
Image: “Gross pathology of atherosclerosis, aorta,” by Patho. License: Public domain
These so-called microangiopathies initially only narrow the vessels. But if one of these plaques ruptures, it can lead to the formation of clots that close the vessel completely, which in turn leads to a heart attack.
In few cases, microangiopathies, where small coronary vessels are located intramural, are responsible for coronary artery disease. Consumption of cocaine, for example, can cause coronary spasms, which can lead to angina pectoris, just like coronary anomalies, coronary fistulas or congenital myocardial bridges.
The resistance of the coronary vessel may also be increased incardiac hypertrophy, hypertension, tachycardia or increased end diastolic valve flow. Thus, these factors may be responsible for angina pectoris as well.
Differential Diagnosis of Coronary Artery Disease
Similar clinical pictures to coronary artery disease
Since the symptom of coronary artery disease is angina pectoris, the differential diagnosis are numerous. The five most important differential diagnoses to be excluded quickly—as they are immediately life-threatening are acute coronary syndrome, pulmonary embolism, aortic dissection, tension pneumothorax and spontaneous rupture of the esophagus (Boerhaave’s syndrome).
In general, the differential diagnosis of chest pain can be divided into cardiac and non-cardiac chest pain:
Differential diagnoses of cardiac chest pain, in addition to acute coronary syndrome, include, for example, hypertensive crisis, valvular heart disease, perimyocarditis or hypertrophic cardiomyopathy, but also Dressler’s syndrome following a myocardial infarction or coronary anomalies.
Non-cardiac causes of chest pain include diseases of the lungs or the pleura, such as pulmonary embolism and lung carcinoma or pleurisy. An aortic dissection may also be present. Furthermore, there may be diseases of the esophagus or the mediastinum, and diseases of the spine and the ribs or abdominal discomfort.
Therapy of Coronary Artery Disease
Acute therapy
Therapy can initially be divided into acute therapy and long-term therapy. In acute cases, nitro compounds that are acting as a vasodilator and thus improve the coronary circulation are suitable. They are contraindicated for patients who are taking PDE-5 inhibitors (e.g., sildenafil, Viagra) or who have HOCM, hypotension or present aortic stenosis.
Long-term therapy
Image: “Drug-based therapy,” by e-Magine Art. License: CC BY-SA 2.0
Long-term therapy can be divided into causal and symptomatic therapy. The causal approach is directed towards the main risk factors that support the emergence of coronary heart disease. Lifestyle changes such as weight reduction, smoking cessation, dietary changes to a Mediterranean diet, controlled physical activity and courses on stress management and relaxation are crucial.
This approach aims to control blood pressure and cholesterol as well as triglyceride levels via a non-drug therapy. Symptomatic treatment, on the other hand, includes medication and invasive approaches. Drug-based therapy aims to prevent myocardial infarction and reduce mortality. It includes aspirin, beta-blockers, statins and ACE inhibitors.
Antianginal therapy
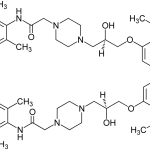
Image: “(±)-Ranolazine Structural Formula,” by Jü. License: Public domain
Antianginal therapy offers several options: beta-blockers to reduce myocardial oxygen demand, nitrates, which hardly find application during long-term treatment, Molsidomine and calcium antagonists, as well as ivabradine and ranolazine.
Revascularization as invasive therapy
Revascularization offers an invasive treatment option. This may also be achieved by means of PTCA (percutaneous transluminal coronary angioplasty) during which dilation via a balloon catheter, followed by stenting, is performed. Impending closures can then be eliminated and the permeability of the vessel can be improved.
A second possibility of revascularization is offered via coronary artery bypass surgery (CABG = coronary artery bypass graft). This can be done via the traditional method with sternotomy access and the use of a heart-lung apparatus. An alternative is the minimally invasive way. The last possibility of therapy that is indicated for coronary heart disease in combination with terminal heart failure is the heart transplant.
Prevention of Coronary Artery Disease
Prevention of coronary heart disease includes the elimination of risk factors, especially the main risk factors of cholesterol, arterial hypertension, diabetes mellitus and nicotine abuse. The approaches should initially manifest in the patients’ behavior, for example, the diet and sporting behavior. Pharmacological support of these approaches is possible, and it may include statinsfor the regulation of lipid metabolism.
Prognosis of Coronary Artery Disease
Several prognostic indicators determine the outcome of coronary heart disease (IHD):
- Function of the left ventricle: increased left ventricular end-diastolic pressure, increased ventricular volume and reduced ejection fraction are associated with poor prognosis.
- Location and severity of coronary artery stenosis: stenosis of the main left anterior descending coronary artery is associated with greater risk and poor prognosis.
- Number and severity of risk factors: large number of risk factors for atherosclerosis are associated with increased risk of myocardial infarction with worse prognosis.
Review Questions
The answers are below the references.
1. The term coronary heart disease describes…
- …a classic chest pain with radiating pain into the left arm.
- …heart disease of the elderly, in general.
- …the manifestation of atherosclerosis in the coronary arteries.
- …an increased blood flow to the coronary arteries during exercise with resulting chest pain.
- …stable angina pectoris.
2. The gold standard for the diagnosis of coronary heart disease is…
- …the ECG at rest.
- …the stress test.
- …the holter monitor.
- …the cardiac MRI.
- …the cardiac catheterization.
3. Which mechanism is most likely based on the pathophysiology of coronary heart disease?
- Plaque formation with stenosis of the coronary arteries and the risk of rupture
- A limitation of the mechanics of the myocardial tissue.
- Terminal heart failure, due to which the coronary arteries are no longer sufficiently supplied with blood.
- Atrial fibrillation with the risk of thrombosis and acute closure of a coronary vessel.
- Increased HDL cholesterol levels, which alter the structure of the coronary arteries.
4. A patient with a recent myocardial infarction (MI), few days after hospital admission, started to suffer from a new episode of chest pain. Which cardiac marker is appropriate to ask for this patient?
- Troponins I and T
- CK-MB
- Myoglobin
- LDH
5. A patient came to the Emergency Department with a typical coronary chest pain. The ECG shows: ST-segment depression with T-wave inversion, and the cardiac markers are negative. The most probable diagnosis is…
- …stable Angina.
- …unstable Angina.
- …ST-Segment Elevation Myocardial Infarction (STEMI).
- …non-ST-Segment Elevation Myocardial Infarction (NSTEMI).
6. IV fibrinolysis is preferred to be given in a patient with ST-Elevation MI if:
- symptoms have been present for > 3 hours.
- cardiogenic shock is suspected/observed.
- increased risk of bleeding.
- delay to PCI would be >1 hour longer than initiation of fibrinolysis.


Magnificent website. Everyone should read. For more amazing info you can find it from this link
ResponderEliminarColonary illness