Thymoma — Staging and Treatment
Table of Contents
A physician’s hands are seen performing a needle biopsy to determine nature of lump either fluid-filled cyst or solid tumor.
Definition and Background
Thymus: This is a part of the immune system that is located in the anterior mediastinum. It is more prominent in children and often extends from 4th costal cartilage to the lower poles of the thyroid gland. It shrinks during adulthood and is slowly replaced by the fat tissue. The thymus plays an important role in the production and maturation of T-lymphocytes that protect the body from various infections.
The thymus is pink to brownish in color and consists of two lobes, which are further subdivided into smaller lobules. Internally, thymus consists of three layers (medulla, cortex, and capsule).
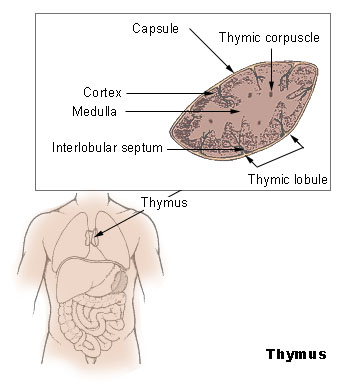
The thymus is supplied by the inferior thyroid and internal thoracic arteries and the venous drainage is by the corresponding veins. The thymus does not receive afferent lymphatics but has the efferent lymphatics that drain into parasternal, tracheobronchial and brachiocephalic lymph nodes.
Thymoma: As the name indicates, it is a neoplasm of the thymus that may be benign or malignant. Thymomas are often linked with myasthenia gravis and other autoimmune diseases. In some studies, thymoma is present in about one-fifth of all cases of myasthenia gravis.
Epidemiology of Thymoma
Thymoma accounts for one-half of the cases of anterior mediastinum neoplasms. It has no sex predilection, with an equal incidence in both males and females. It commonly occurs in fifth and sixth decades, with the mean age of 52 years at the time of presentation.
Etiology of Thymoma
Etiological factors of thymomas are not clearly known, however, some of the common condition associated with the thymomas are:
- Myasthenia gravis (approximately one-third of cases)
- Autoimmune and systemic disorders such as SLE, dermatomyositis, Cushing syndrome, and SIADH.
- Inflammatory processes of the anterior mediastinum (cysts)
- Congenital pathology in the thymus development and embryogenesis
- Ectopic thymic tumors occur due to the abnormal formation of the thymus cells in other parts of the body: the neck, pericardium, pleura, and lung.
Classification of Thymoma
Thymomas are divided into the two main groups benign (non-invasive) and malignant (invasive) neoplasms.
WHO classification
The World Health Organization (WHO) has classified thymoma into different types based on the histology.
Clinical Presentation of Thymoma
History and physical examination
About one-third of thymomas are asymptomatic and are found accidently on imaging done for other conditions. Another one-third of patients with thymoma present clinically due to local compressive effects of enlarged thymoma. These symptoms may be:
- Cough
- Breathlessness
- Chest pain
In advanced forms there also may be:
- Superior vena cava syndrome
- Phrenic nerve paralysis
- Hoarseness due to the involvement of recurrent laryngeal nerve
- Persistent pleural effusions
- Oncogenic set: weight loss, fever, fatigue, and night sweats
On physical examination, the most evident signs are those that are associated with myasthenia gravis, systemic disorders (SLE, dermatomyositis etc), hypogammaglobulinemia or red cell aplasia.
Diagnosis of Thymoma
The thoracic imaging (CT scan and/or MRI) are part of the initial evaluation of a patient with a suspected thymoma. It confirms the presence of an anterior mediastinal mass. The biopsy of the anterior mediastinal mass is necessary to confirm the diagnosis of thymoma.
The important differential diagnoses of anterior mediastinal mass include lymphoma, retrosternal goiter, and mediastinal germ cell tumor. Thus, germ cell tumor markers (beta-HCG and alpha fetoprotein) and thyroid function tests are also included in the initial workup.
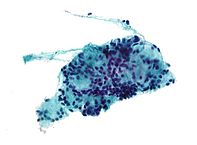
Fine-Needle Aspiration (FNA) and Biopsy
- The preoperative biopsy is compulsory for the diagnosis of thymoma.
- Limited anterior mediastinotomy (Chamberlain approach)
- Thoracoscopic approach
- Core biopsy in conjunction with FNA
Imaging studies
- Radiography detects the majority of thymomas which appear as the space occupying formations in the upper half of the chest overlapping the cardiac shadow close to the heart and large vessels.
- CT determines smaller tumors, which were not detected in radiography
- Positron emission tomography
Staging of Thymoma
The staging is an important part of management and prognosis stratification of cancer, including thymoma. The Masaoka system is the most common staging system used to stage thymomas. This system, was initially proposed in 1981 and has been modified several times over the years, it divides thymoma into four stages. The stages along with the corresponding treatment options are summarized in the table below:
Management of Thymoma
The surgery (thymectomy) is the main treatment option for thymoma, provided there is an appropriate access to the tumor, which makes it possible to remove it completely. If surgery cannot be performed due to any reason then chemotherapy, radiotherapy, and close monitoring are the other available options.
Corticosteroids have been proved to contribute in regression of the neoplastic cells in the affected thymus.
The chemotherapeutic regimen consisting of cisplatin/ vincristine/ doxorubicin/ cyclophosphamide is used for incompletely resected invasive thymomas or cases with unresectable disease.
The long-term monitoring is a vital part of management and should last throughout the patient’s life. Relapse after primary diagnosed and cured thymoma may occur after 10-20 years.
Review Questions
The correct answers can be found below the references.
1. A 77-year-old female presents to you complaining of breathlessness, dizziness, cough, and feeling of” heaviness” in the chest after mild exertion. On physical examination, there is cervical or axillary lymphadenopathy. The skin is dry but with no cyanosis. ECG reveals normal age findings, Full blood counts, electrolytes, and LDH are within normal limits. Radiography indicated a smooth mass in the anterior part of the mediastinum overlaying the heart shadow. Histological study (after FNA) indicates numerous adipose cells overlapping a number of thymic cells, which looks absolutely normal. What is the most probable diagnosis?
- Benign thymolipoma
- Medullary thymoma
- Mixed thymoma
- Predominantly cortical thymoma
- Cortical thymoma
2. An 81-years white man complains of cough, chest pain, hoarseness, fever, night sweats, fatigue on minimal exertion, and weight loss. Physical examination reveals pallor and axillary lymphadenopathy. CT scan chest detected a formed mass in the mediastinum with an uneven surface, embracing heart on its front surface. FNA delivered some biomaterial where numerous epithelial cells were found, which hardly reminds normal thymic cells. CBC: elevated ESR. What is the most probable diagnosis?
- Benign thymoma.
- Thymic carcinoma
- NHL
- HL
- Tuberculosis
3. Biomaterial obtained from FNA of thymus revealed spindle-shaped or oval epithelial cells of usual appearance. What are the most probable diagnosis and disease-free survival rate at 10 years for the assumed condition?
- Medullary thymoma, survival, 100 %.
- Predominantly cortical thymoma, 83 %.
- Cortical thymoma 83 %
- Well-differentiated thymic carcinoma 35 %
- Thymic carcinoma 28 %


Comentários
Enviar um comentário