Anesthesia Machine — Safety Features
Table of Contents
Image: “Flow-I anesthesia machine, manufactured by Maquet, a division of Getinge Group, Getinge, Sweden.” by DiverDave – Own work. License: CC BY-SA 3.0
The Anesthetic Machine
From simple to complex over 100 years
Image: “The Schimmelbusch mask” by Jenny O’Donnell. License: CC BY-SA 2.0 uk
The earliest attempts to provide anesthesia was by dropping liquid anesthetic (Ether, Chloroform) on a cloth on the patient´s face. The figure shows a more sophisticated device (still used in developing countries where Ether is used), the Schimmelbusch Mask, on which Ether is dripped and dispersed assuring better evaporation and control of depth of anesthesia.
The modern machine
The modern machine is a highly sophisticated device with a number of safety features built in and required for safe administration of anesthetics. Machines are serviced at least annually. The vaporizers are separately calibrated annually. Monitors have become a part of the machine.
Safety Features
There are several international standards specifying the desired and absolutely essential safety features for anesthesia machines. The American Society for Testing and Materials (ASTM) Standard covers all anesthesia machines.
Failure of anesthetic machines is a rare event but the providers have to be vigilant at all times to ensure that there are no faults in the machine or in the entire anesthesia delivery apparatus.
The pneumatic systems in the anesthesia machines can be classified as high, intermediate and low-pressure systems. Every single component has a safety feature. A comprehensive description of all the safety features is beyond the scope of this article.
High-pressure systems are composed of cylinders with their yoke assemblies, cylinder pressure indicators, and pressure regulators.
The intermediate pressure systems are composed of an inlet pipeline, a master switch, pressure indicators, pressure regulators, ventilator auxiliary gas outlets, oxygen failure and oxygen pressure failure devices, oxygen flush and flow control valves.
The low-pressure systems consist of flow meters, hypoxia prevention devices, vaporizers, unidirectional valves and pressure relief devices.
Partial Rebreathing System
- Efficiency and cost savings—environmentally friendlier than older systems
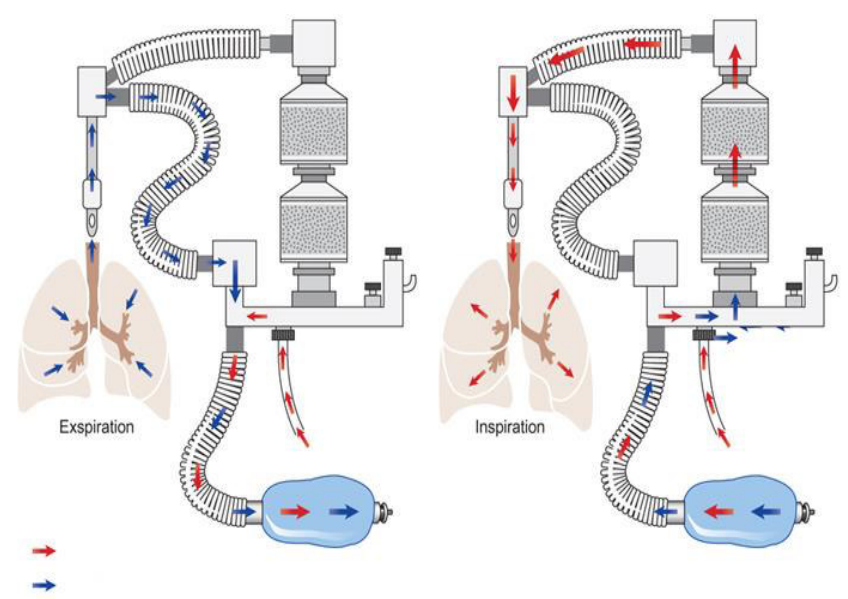
In the figure, “fresh gases” added by the machine are indicated by red arrows. Expired gas from the patient is indicated by blue arrows.
The anesthesiologist sets the machine to deliver more oxygen (usually about twice as much) as the patient is likely to need. The unused oxygen and anesthetic vapors are exhaled and then rebreathed thus saving the cost of excess oxygen of anesthetic. Expired carbon dioxide “scrubbed” from the expired gas before rebreathing occurs.
Removal of carbon dioxide
- Re-breathing of carbon dioxide causes acidosis and lowers oxygen content in the lung
The “soda-lime” canister
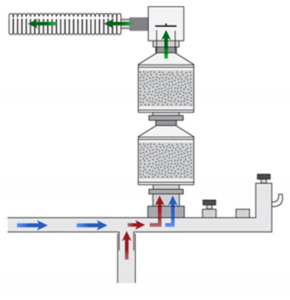
Expired gas (blue) and fresh gas (red) flows through a soda lime canister. The green gas flowing to the left at the top of the figure is a mixture of fresh gas and exhaled gas from which the carbon dioxide has been removed.
Soda lime:
- Calcium hydroxide: Ca(OH)2 (about 75 %)
- Water: H2O (about 20 %)
- Sodium hydroxide: NaOH (about 3 %)
- Potassium hydroxide: KOH (about 1 %)
Action of soda lime
- Removal of exhaled carbon dioxide
- The overall reaction is: CO2 + Ca(OH)2 → CaCO3 + H2O + heat (in the presence of water)
- Water, calcium carbonate, and heat collect in the soda lime
There is a colored dye in the soda lime which changes color when the material is exhausted and indicates it is time to replace the soda lime. Modern anesthetic machines also have monitors which alarm if carbon dioxide is being re-breathed. Baralyme (contains barium hydroxide) can be used instead of soda lime. The heat produced by the scrubbing of the expired gases may be sufficient to cause partial breakdown of sevoflurane with the release of compound A which causes kidney damage in rats. The recommended flow through the anesthetic machine when using sevoflurane is 2–3 liters per minute to maintain lower temperatures in the soda lime. Excess gases in the circuit are released through an adjustable valve mechanism and are “scavenged” to the outside atmosphere
High-Pressure System
Gas cylinders
To prevent the wrong gas from being used, the gas cylinders are color-coded according to International Safety Standards and a PIN index system:
- Oxygen cylinder: black body with white shoulders
- Nitrous oxide: blue
- Air: black and white
- Carbon dioxide: gray
- Helium: brown
- Entonox: black with blue-white shoulders
The same color codes are also used on all the hoses, caps, knobs, connectors and pressure gauges of the respective gases.
The PIN index system prevents the incorrect gas cylinder from being attached to the hanger yokes of the anesthesia machine.
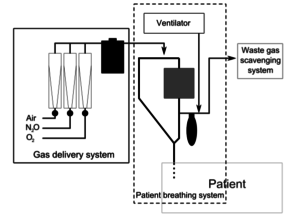
Image: “A simple schematic of an anesthesia machine showing three main subsystems: gas delivery, patient breathing circuit (showing both the absorber and ventilator), and waste gas scavenger. Not shown are safety and monitoring devices.” by TwoOneTwo – Own work. License: CC BY-SA 3.0
Pressure relief devices are fitted on all cylinders to vent cylinder contents in case there is built up pressure within the cylinder (with over-filling or mis-filling of gas).
Pressure regulators are specific for each gas to provide a constant low pressure to match the anesthesia machine.
Intermediate Pressure System
Schrader probe: to prevent pipelines of different gases crossing over or being connected wrongly, a Schrader socket assembly is fitted only for the same gas.
Hose pipes: kink proof, color-coded and flexible hose pipes are used.
Gas Pipelines at the machine end: a unidirectional valve at the machine end ensures that a color-coded hose pipe delivers gas specifically to the gas service.
Pipeline pressure indicators with color-coded dials are fitted for each gas.
Oxygen failure system: A loud audible (minimum 60dB), a non-mutable alarm is sounded for at least 7 seconds whenever the oxygen pressure falls below a certain pre-determined safe threshold. Older machines had the “Ritchie whistle” to alert when the oxygen pressure decreased to 260 kpa or less. The alarm is linked to a gas shut off valve to cut off the patient from anesthetic gases.
Oxygen flush is a switch located in a shallow recess. It is activated by a finger to activate emergency oxygen directly from the cylinder or pipeline. The switch is turned off as soon as the finger is removed.
Low-Pressure System
Flow meters: for ease of identification, the knobs (on/off) on the oxygen flow meters are fluted and larger than the ones on the nitrous oxide or air flow meters. In addition, the oxygen flow meters are always located downstream from the nitrous and air flow meters. This prevents a leak in the low-pressure system by diluting the oxygen and leading to a mixture of hypoxic gases.
The nitrous oxide flow meter is set up so that it is automatically disabled whenever the oxygen flow meter is set to less than 21 % or if the oxygen supply fails.
Vaporizers have a stiff button which has to be pushed prior to turning on the vapor. To prevent all vaporizers from working simultaneously, there is an interlocking system to ensure that only one vaporizer works at a time.
Pressure relief device is located between the common gas outlet and the vaporizer. It protects the anesthesia machine by venting gas to the atmosphere if high pressures develop within the system.
Common gas outlet (CGO): newer anesthesia machines often have more than one CGO. Therefore, machine standards ensure that in such machines, only one CGO is functioning at any given time.
Hypoxia prevention device ensures that there is a pre-decided level of oxygen flow e.g. the mandatory minimum oxygen flow is 150 -250ml/min.
Scavenging System
There are strict international regulations for scavenging system standards. All scavenging system connections have 30 mm diameter to prevent any misconnections as airway accessories have 15/22 mm diameter.
Negative and positive pressure relief valves are incorporated into the scavenging systems to prevent transmission of high pressures in the breathing system, in case the system malfunctions.
Every anesthetic machine is installed with a standard oxygen analyzer, a low-pressure analyzer, a high-pressure analyzer and a spirometer.
Monitoring System
It is mandatory for every anesthesia machine to have the following monitors:
- ECG: preferably five lead
- Blood pressure cuff: automated and regularly calibrated
- Pulse oxygen saturation monitor
- Carbon dioxide end-tidal monitor which measures the expired carbon dioxide
- Tidal volume and airway pressure monitor
Other monitors which can be installed depending on the anesthesia provider are:
- Temperature monitor, which is required in the United States
- Peripheral nerve stimulator for monitoring the status of the muscle relaxation
- End-tidal vapor monitor
- Ultrasound to detect pneumothorax or abdominal problems
Monitors required for high-risk patients include:
- Invasive blood monitors for blood pressure, central venous pressure, and pulmonary arterial pressure
- Intracranial pressure monitor
- Trans-esophageal echocardiography (TEEC)
- Sensory and motor potentials
- EEG
- Fetal heart monitor
- Uterine contraction monitor
- Cerebral monitors (BIS, cerebral oximetry)


Comentários
Enviar um comentário