Intimate Partner Violence (IPV) and Sexual Assault
Sandra CruzPresidente da ApeartdFica o artigo elaborado nos USA;)
Physicians, especially family physicians, are often the first contacts for survivors of intimate partner violence and occasionally for sexual assault victims too. Both these problems are prevalent worldwide with both sexes being affected, although women are more affected than men. Besides physical harm and death, intimate partner violence (IPV) and sexual assault can also cause psychological and psychiatric problems. Family physicians should be prepared to identify and provide supportive care to these patients.
Table of Contents
- Definition of Intimate Partner Violence and Sexual Assault
- Epidemiology of Intimate Partner Violence and Sexual Assault
- WHO guidelines for Intimate Partner Violence and Sexual Assault
- Identification and Care for Survivors of Intimate Partner Violence
- Clinical Care for Survivors of Sexual Assault
- Recommendations for Sexual Assault Evaluation
- What Can a Family Physician do?
- References
Image: “eye” by hans van den berg. License: CC BY-SA 2.0
Definition of Intimate Partner Violence and Sexual Assault
Intimate partner violence is a pattern of assaultive behavior and coercive behavior. It may include:
- Physical injury
- Psychologic abuse
- Sexual assault
- Progressive isolation
- Stalking
- Deprivation
- Intimidation
- Reproductive coercion
Sexual assault is a crime of violence and aggression. It ranges from sexual coercion to contact abuse (unwanted kissing, touching, or fondling) to rape.
Epidemiology of Intimate Partner Violence and Sexual Assault
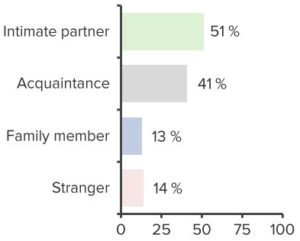
“Epidemiology of Sexual Assault” Image created by Lecturio
Approximately, 25 % of women and 7.6 % of men in the United States are estimated to have been survivors of IPV during their lives. Physical assault or rape by an intimate partner is reported in approximately more than half a million men and 1.5 million women every year. Women are more likely to suffer IPV compared to men.
Following IPV and sexual assault, women also have a higher incidence of urinary, gynecologic, gastrointestinal, neurological, musculoskeletal issues with sexually transmitted infections (STIs), chronic pain syndromes, abortions or poor outcomes of gestations. Approximately 20% of women seeking care in family planning clinics who had a history of abuse also experienced pregnancy coercion and 15% reported birth control sabotage.
Special population at risk of IPV:
- Adolescents
- Immigrant women
- Women with disabilities
- Older women
WHO guidelines for Intimate Partner Violence and Sexual Assault
The World Health Organization has recommended guidelines for identifying and managing IPV. Their recommendations include:
Women-centered care focuses on providing confidential, supportive and non-judgmental careto patients who disclose a history of IPV. The healthcare provider should listen closely, without pressurizing the patient, about the violence. In addition, the healthcare provider should help provide information to access legal and supportive services to protect the victim and his/her children. If a healthcare provider is unable to provide the support, then they should arrange for someone who can provide it.
Identification and Care for Survivors of Intimate Partner Violence
Routinely, a healthcare provider is not expected to inquire about IPV, but should ask about exposure if the patient has conditions which suggest IPV. Mental health care, support, and cognitive behavior therapy should be offered the patients with a history of IPV.
Clinical Care for Survivors of Sexual Assault
Interventions within 5 days of assault obtain a thorough history of time, duration, and type of assault, pregnancy risk, a risk of STIs and mental health. Emergency contraception should be offered to victims within 5 days of the IPV or sexual assault. A single dose of 1.5mg levonorgestrel is recommended.
A safe abortion should be offered if the woman presents after 5 days of sexual assault and is found to be pregnant. Post-exposure HIV prophylaxis: should be considered if women present within 72 hours of the sexual assault.
Survivors of sexual assault should be offered prophylaxis for STIs like chlamydia, gonorrhea, trichomonas, and syphilis.
Hepatitis B vaccine
Obtain a blood sample for determining immune status. If the survivor is not immune, then the first dose of Hepatitis B vaccine may be administered. Supportive care and written information on coping strategies should be offered. Supportive care should be offered up to 3 months after IPV/sexual assault. Interventions for mental health problems may be required in survivors even beyond 3 months after IPV/sexual assault.
Mandatory reporting of IPV
Mandatory reporting of IPV is not recommended; however, the healthcare provider can, at the request of the survivor of IPV/sexual assault, report the incident to the appropriate authorities or police.
Recommendations for Sexual Assault Evaluation
Medical issues:
- Obtain informed consent
- Assess and treat physical injuries
- Obtain past gynecologic history
- Perform a physical examination, including pelvic examination, with an appropriate chaperone
- Obtain appropriate specimens and serologic tests for STI testing
- Provide appropriate infectious disease prophylaxis as indicated
- If the assailant´s HIV status is unknown, evaluate the risks and benefits of nonoccupational postexposure prophylaxis
- Provide or arrange for the provision of emergency contraception as indicated
- Provide counseling regarding findings, recommendations, and prognosis
- Arrange follow-up medical care and referrals for psychosocial needs
Legal issues
- Provide accurate recording of events
- Document injuries
- Collect samples as indicated by local protocol or regulation
- Identify the presence or absence of sperm in the vaginal fluids and make appropriate slides
- Report to authorities as required
- Ensure security of chain of evidence
What Can a Family Physician do?
Family physicians, due to the nature of their profession, play a pivotal role in identifying survivors of IPV/sexual assault and intervening and treating their physical and psychological problems. In addition, family physicians can provide continuous support and access to resources to help survivors of IPV and sexual assault.
Awareness
Non-judgmental and respectful screening and questioning by the family physician helps to obtain sensitive information about IPV, as well as sexual assault. Confidentiality and awareness of the unique relationship dynamics e.g. gays, lesbian, transgender, bisexuals, immigrants and elderly couples is essential.
The family physician can include a history of violence in routine questioning and ask questions like “have you been hit by someone recently or during the past 6 to 12 months”; or “are you, or have you been in a relationship in which you have felt afraid of being hurt.”
Identification
To identify IPV and sexual assault survivors, many screening tools and protocols have been devised. The tools include 3 to 8 questions on safety, coercion, physical, emotional and sexual abuse. The American Academy of Pediatrics recommends routine inquiry in all cases of suspected IPV, while the American Medical Association and the American Congress of Obstetricians and Gynecologists recommend IPV inquiry in all patients.
Screening can be performed during routine well-adult examinations or prepartum and postpartum visits or specifically when patients present with signs of IPV or sexual assault. Validated patient self-report questionnaires, prompts in the electronic health records or the patient’s paper chart can assist in the identification of IPV.
Intervention
The family physician can use statements like “no person deserves to be abused” or “you have a right to be respected and be safe” to convey concern. Physicians are required to formulate a plan and assist survivors of IPV and sexual assault, besides discussion options, documenting findings and offering continuity of care.
The patient will require support in deciding whether to stay with the abusive partner or to leave and be safe. It is recommended that couples counseling should be avoided if there is a history of active violence, fear, intimidation etc.
Prevention
Educational posters and brochures can be made available, as well as prominently displayed in the physician’s office to provide information on IPV and sexual assault, along with available resources for the survivors. Information about healthy relationships should also be included in the educational materials.

Comentários
Enviar um comentário