Pericardial Effusion And Cardiac Tamponade — Symptoms and ECG
Table of Contents
- Epidemiology of Pericardial Effusion
- Etiology of Pericardial Effusion
- Pathology and Pathophysiology of Pericardial Effusion
- Symptoms of Pericardial Effusion
- Diagnosis of Pericardial Effusion
- Differential Diagnoses of Pericardial Effusion
- Therapy of Pericardial Effusion
- Progression and Prognosis of Pericardial Effusion
- Review Questions
- References
Image: “A coronal CT showing a pericardial effusion identified by a white arrow” by James Heilmann, MD. License: CC BY-SA 3.0
Epidemiology of Pericardial Effusion
Widespread pericardial effusion
Asymptomatic pericardial effusions have been shown in about 3 % of patients at autopsy. The groups at greatest risk of developing pericardial effusion include patients with cancer and patients with HIV and AIDS. Tamponade, requiring a large effusion, is less common.
Etiology of Pericardial Effusion
Effusions and tamponades mainly caused by pericarditis and malignancy
Effusions and tamponade can occur as a result of pericarditis of any type. Malignancy, especially lung and breast cancer, is the most common cause of effusion and tamponade followed by uremia and infectious disease. Effusion is also common after cardiac surgery while an effusion due to a myocardial rupture is rare.
Pathology and Pathophysiology of Pericardial Effusion
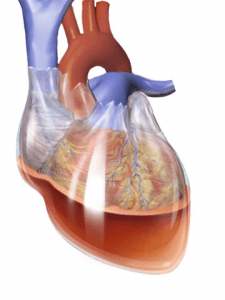
The pericardial space normally contains a small volume of serous fluid. Under normal circumstances it cushions the heart and allows for a low friction environment so the heart can move easily. If fluid were to fill the pericardial space rapidly, as in a penetrating chest trauma, as little as 150 ml could lead to tamponade. If fluid were to slowly accumulate, then the pericardial sac could stretch to accommodate about 2 l of fluid without symptoms.
Pericardial effusions can be serous, hemorrhagic or serosanguinous (a pink mixture of serous and hemorrhagic).
As the pericardial effusion continues to grow diastolic fillingwill be affected. The physiologic response is to increase the heart rate in order to maintain cardiac output. Venous return is also hampered by the gathering fluid, resulting in intravascular buildup in the superior and inferior vena cava and a collapse of the right atrium and ventricle and then left ventricle and a drop in cardiac output. Insufficient cardiac output eventually leads to shock.
Causes of pericardial effusion and cardiac tamponade:
- Neoplasm i.e. breast, lung
- Postmyocardial infarction
- Postpericardiotomy syndrome
- Hypothyroidism
- Viruses like coxsackie group B, influenza, echo
- Bacterial infection
- Connective tissue disease SLE
- Trauma
- Uremia
- Drug induced
Symptoms of Pericardial Effusion
Signals of pericardial effusion
Symptoms of a cardiac effusion include the following:
- Chest pain or pressure
- Palpitations
- Cough
- Additionally the patient may present symptoms related to the underlying cause of the effusion.
Symptoms of cardiac tamponade
As the effusion grows into a tamponade other symptoms become accumulate:
- Tachycardia
- Tachypnea
- Dyspnea
- Hypoperfusion leads to cold/clammy extremities
On physical look for Beck’s Triad:
- Low blood pressure
- Distended neck veins
- Muffled heart sounds on auscultation
Also look for pulsus paradoxus, an abnormally large drop in systolic blood pressure (normal drop is < 10 mm Hg) during inspiration with a lack of palatable radial pulse and Kussmaul’s sign, a paradoxical increase in venous pressure during inspiration.
On x-ray the pericardial silhouette is enlarged and takes on a “water-bottle” shape.

Image: “Water bottle” by Jer5150. License: CC BY-SA 3.0
Diagnosis of Pericardial Effusion
How to detect pericardial effusions and cardiac tamponades
Small effusions that are found incidentally are usually worked up to determine their etiology. An echocardiogram is used to verify the effusions size. It presents as an anechoic space between the layers of the serous pericardium. This will appear black (remember bone appears white, fluid appears black on ultrasound and echocardiogram).
If the effusion is small and the patient is asymptomatic then the underlying condition is treated and the effusion is monitored. A large effusion may cause the pericardium to “swing” on echo, as the motion of the heart is transmitted through the fluid to the pericardium.
The effusion becomes a cardiac tamponade when sufficient fluid has accumulated in the pericardial space to inhibit proper heart function. Cardiac tamponade is a clinical diagnosis, an enlarged pericardial silhouette on chest x-ray is insufficient to make the diagnosis. If there is a concern for tamponade a patient will be evaluated for Beck’s triad, pulsus paradoxus, echocardiograph and EKG.
On echocardiogram the tamponade will demonstrate the following:
- A large pericardial effusion
- A collapse of the right ventricle during diastole
- Dilation of the inferior vena cava
- Compression of the left atrium and ventricle
This will result in poor left heart filling with a drop in cardiac output and venous stasis in the superior and inferior vena cava.
Image: “Pericardial effusion with tamponade” by Jer5150. License: CC BY-SA 3.0
Signs of tamponade on ECG include sinus tachycardia, low-voltage QRS complexes and electrical alternans, consecutive QRS complexes that alternate in height.
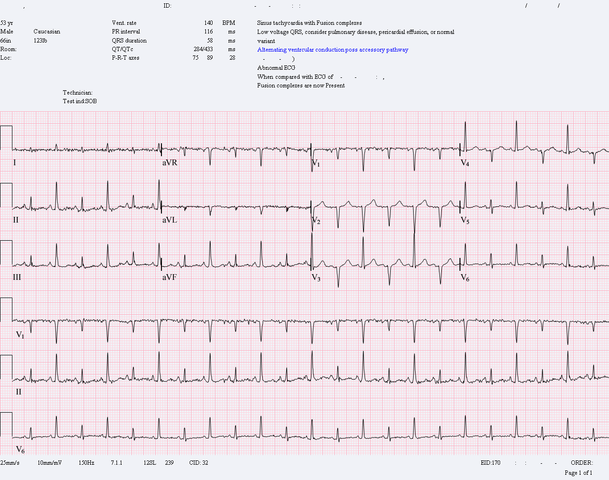
Image: “Pericardial effusion with tamponade” by Jer5150. License: CC BY-SA 3.0
Differential Diagnoses of Pericardial Effusion
To be distinguised from effusion and tamponade
- Cardiogenic Shock
- Constrictive Pericarditis
- Pneumothorax
- Pulmonary Embolism
Therapy of Pericardial Effusion
How to treat pericardial effusions and cardiac tamponades
Cardiac effusion will focus on removing the effusion, preventing further effusions and treating the underlying cause. Medical treatment depends on etiology includes
- NSAIDs, first line therapy
- Colchicine
- Antibiotics, if caused by infection
Small effusions are monitored by echocardiography. Larger effusions are removed via pericardiocentesis. If recurrence is a concern a pericardial window may be installed, a permanent catheter that drains the any pericardial fluid into the peritoneal cavity.
Cardiac tamponade is a medical emergency and is treated with oxygen, volume expansion (IV fluids) to increase cardiac output, inotropic drugs (eg, dobutamine) to increase cardiac output, and elevating the legs to improve venous return. Pericardiocentesis should be performed as soon as the patient is stable.
“Treatment of Pericardial Effusion” Image created by Lecturio
Progression and Prognosis of Pericardial Effusion
Etiology defines prognosis of effusions and tamponades
Prognosis of pericardial effusion depends on the etiology. Treating the underlying cause may be curative. Small effusions are simply monitored. However, untreated cardiac tamponade is rapidly fatal. Long term survival depends on etiology. Tamponade induced by malignancy has the worst long term prognosis.
Review Questions
The answers are below the references.
1. A 55 year old female with progressive dyspnea over last three weeks and a sharp chest pain over last two days. On physical exam she shows jugular vein distention and a drop of 12 mm Hg in systolic blood pressure during inhalation. EKG shows sinus tachycardia with diffuse and nonspecific ST changes. What is the next step in the management of this patient?
- Ventilation-Perfusion scan
- Bronchoscopy
- Paracentesis
- Echocardiography
2. Which of the following is NOT part of Beck’s triad:
- Low blood pressure
- Pulsus paradoxus
- Muffled heart sounds
- Jugular vein distention
3. Which conditions must be met to classify a patient with pulsus paradoxus?
- A drop in systolic blood pressure greater than 10 mm Hg during instpiration
- An increase in jugular veinous pressure with inspiration.
- A lack of radial pulse though you can detect beats on cardiac auscultation.
- A and C

Comentários
Enviar um comentário