Neuroblastoma — Symptoms, Classification and Survival Rate
Table of Contents
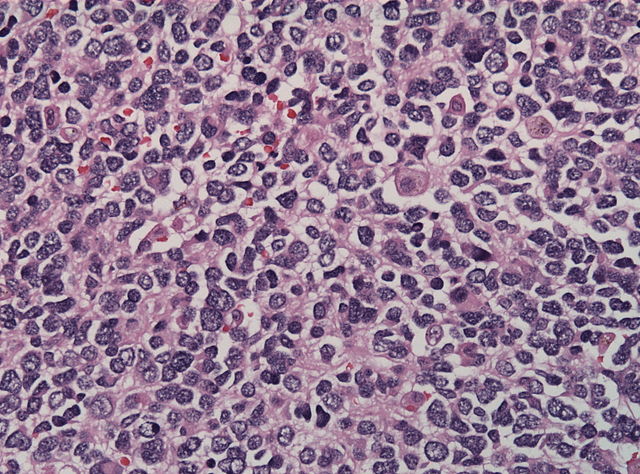
Image: “Histopathology specimen of neuroblastoma” by . License: CC BY-SA 3.0
Definition of Neuroblastoma
Neuroblastoma is an embryonal tumor of the post-ganglionic sympathetic nervous system. It mostly occurs during infancy and originates from stem cells of the sympathetic nervous system (neuroblasts).
Approximately half of all neuroblastomas have already metastasized at the time of diagnosis, yet the prognosis is promising, and spontaneous remission is common.
Epidemiology of Neuroblastoma
Neuroblastoma as an extracranial malignant solid tumor
Second to brain tumors, neuroblastoma is one of the most common extracranial malignant solid tumor during infancy and accounts for 10 % of childhood-associated cancers. There are about 700 new cases of neuroblastoma each year in the United States, with 90 % of patients falling ill before school age. The prevalence sits at 1 in 7000 children.
It is more common among white children. the disease has a slight male preponderance with a male: female ration of 1.2:1.The average age of onset is two years, but older children may develop neuroblastoma as well. Especially in infants, spontaneous remissions can occur even with metastatic cancer.
Etiology of Neuroblastoma
Causes of neuroblastoma
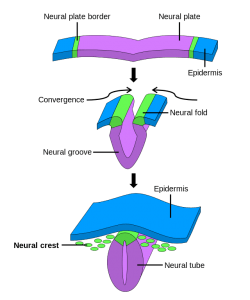
Image: “Neural crest formation during neurulation.” By . License: CC BY-SA 3.0
The tumor is thought to be genetic and inherited in an autosomal dominant pattern of inheritance with germinal mutation being the main pathologic lesion.
The tumor is thought to arise because of the Knudson’s two hit hypothesis theory where two hits in DNA are involved in the causation of the disease.
The distribution of the tumor involves the pattern taken by migration of neural crest cells since the origin of neuroblastoma are the cells of the neural crest, which later develop into the sympathetic ganglia and adrenal medulla. The neuroblasts remain in an immature state instead of differentiating and mutate into malignant cells. It is assumed that the amplification of the cellular oncogen N-myc contributes to the progression of the neuroblastoma.
This amplification, which is observed in 20 % of tumors, is the consequence of a 1p-deletion, a loss of the p-arm of the first chromosome. It was observed that spontaneous tumor regression does not occur when a MYCN (= N-myc) amplification is present. Hence the MYCN amplification makes a deep impact on treatment decisions.
About 50 % of neuroblastomas develop in the adrenal medullary. Other locations are the cervical, thoracic and abdominal areas along the sympathetic trunk, with the abdominal cavity making up about 70% of the cases.
Metastases primarily appear in the bone marrow, bones and locoregional lymph nodes. If metastases appear in the liver, the condition is referred to as Pepper syndrome. In rare cases, an intracranial metastasis is found.
Clinical Presentation and Symptoms of Neuroblastoma
Site-related symptoms of neuroblastoma
Image: “Horner syndrome” by Davplast. License: CC BY-SA 4.0
Depending on the localization, typical symptoms can be observed.
Neuroblastoma in the cervical region can provoke Horner’s syndrome, which involves miosis, ptosis hemifacial anhidrosis and enopthalmos. That arises from compression and involvement of the sympathetic chain.
Cervical or thoracic localization leads to Cough and dyspnea.
Characteristic of an hourglass tumor is paraplegia and lesions of nerves, since the tumor infiltrates through the neuroforamina into the intraspinal room.
A protruding abdomen is frequently associated with an abdominal localization.In this presentation hypertension may arise from renal artery compression and not hormone secretion.
General symptoms of neuroblastoma
General symptoms like fever, pain, loss of appetite, fatigue, bone pain, fractures and deformities are signs of metastases.
Due to the tumor’s production of hormones, symptoms which indicate a sympathetic overactivation, like arterial hypertension or diarrhea, can occur. This diarrhea is resistant to therapy and is the result of the higher secretion of vasointestinal peptide (VIP); even though it occurs rarely, it is characteristic of neuroblastoma.
Neuroblastoma as opsoclonus-myoclonus-ataxia (Kinsbourne syndrome)
In rare cases, approximately 2 %, the neuroblastoma is associated with the paraneoplastic syndrome of a cerebellar ataxia with myoclonus of the trunk and extremities and spontaneous nystagmus (opsomyoclonus). For this reason, it is also referred to as dancing feet and dancing eye syndrome. Sometimes, yet for unkown reasons, this so-called opsoclonus-myoclonus-ataxia syndrome leaves permanent neurological and cognitive deficits associated with psychomotoric retardation—even if the neuroblastoma is successfully cured.
Diagnostics of Neuroblastoma
Sonography and radiology of neuroblastoma
If a neuroblastoma is strongly suspected, sonographic and radiological imaging of the tumor should be taken in order to rule out an hourglass tumor due to the imminent development of paraplegia.
Image: “Neurblastoma, CT of the Abdomen” by . License: CC BY-SA 3.0
Scintigraphy of neuroblastoma
Scintigraphically, a neuroblastoma can be displayed using iodine-131-meta-iodobenzylguanidine (MIBG), which is an analogue to noradrenaline, since the adrenergic tissue absorbs this substance. Scintigraphy is also a convenient method for assessing the progression of the disease because reduction in size can be well observed.
Urine can be used to detect higher excretion, while serum is convenient for detection of higher concentration of vanillylmandelic acid and homovanillic acid. These are metabolites of the increased metabolism of catecholamines and represent evidence for a neuroblastoma since neuroblastoma produce catecholamines (as do the chromaffin cells of the adrenal medulla).
As differential diagnosis, nephroblastomas and lymphomas are a possibility; however, these tumors do not cause an increased level of degradation products of catecholamines. Often, unspecific tumor-associated parameters (such as lactate dehydrogenase, ferritin and the neuron-specific enolase) are elevated as well.
Importantly, an infiltration of the bone marrow must always be ruled out by confirming the amplification of the N-myc oncogen using tumor material and bone marrow punctures at 4 puncture sites, since this would require a different treatment approach.
Classification of Neuroblastoma
Histological classification of neuroblastoma according to Hughes
The histological classification of neuroblastoma is made in 3 degrees of malignancy according to Hughes. 50 % of all cases are grade 3 neuroblastoma. If the neuroblastoma differentiates by forming numerous mature ganglionic cells, it is called a benign ganglioneuroblastoma.
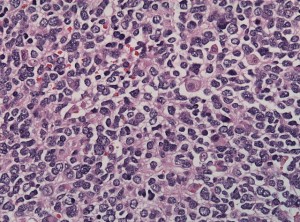
Histological characteristics of neuroblastoma
Image: “Histopathology specimen of neuroblastoma” by . License: CC BY-SA 3.0
At macroscopic level, a dark, sanguineous cross-section with calcifications can be seen. The most common degree of malignancy, the undifferentiated neuroblastoma, does not show any forms of differentiation such as Neuropil or ganglionic cells. Sometimes, neuroblasts are arranged in rosette patterns with a Neuropil-center, the so-called Homer Wright rosettes.
In contrast, the diffuse ganglioneuroblastoma consists of a mixture of neuroblasts, Schwann cells and ganglion cells. The nodular ganglioneuroblastoma shows a nodose structure consisting of neuroblastic foci and tumor parts made of ganglioneurons.
International Neuroblastoma Staging System (INSS) of neuroblastoma
Furthermore, the classification in 5 clinical stages according to the International Neuroblastoma Staging System (INSS) is important. More than 60 % of children are diagnosed in stage IV.
Stage I: Tumor is confined to the organ of origin.
Stage II: The neuroblastoma is localized, but infiltrates the surroundings, yet without infiltrating across the midline.
Stage III: Tumor infiltrates across the midline.
Stage IV: Hematogenic metastases in other organs are present.
Stage IV-S: The neuroblastoma is detected during early infancy and metastases can be found in the liver, skin, and bone marrow. There are no metastases in the skeleton (better prognosis than stage IV).
Treatment of Neuroblastoma
Types of treatment for neuroblastomas
The treatment of neuroblastoma depends on the age of onset and on the stage of diagnosis. In cases of local foci without MYCN amplification, a spontaneous regression of the tumor is not uncommon so that treatment can be temporizing at first. In stages I and II, surgery would be the first step to be followed, just as in stage III, by a combined chemotherapy and possibly radiation. In Stage IV, an additional 131J-MIBG-therapy and an autologous bone marrow transplant become necessary.
For maintenance treatment, retinoids and arsenic trioxide are administered. Retinoles trigger a decreased proliferation and MYCN expression. Additionally, topoisomerase-I inhibitors like topotecan are used more and more frequently.
Prognosis for neuroblastoma
Prognosis in stage I and II is promising with a cure rate above 90 %. In stage III and IV-S, the 5-year survival rate is about 60 – 70 %. For stage IV, prognosis is very bad.
Negative prognostic factors include high lactate dehydrogenase, age > 1 year, bad resectability of the tumor and amplification of N-myc.
Follow-up diagnostics and aftercare of neuroblastoma
Follow-up diagnostics use radiological procedures to track a reduction in size and to thus see if the patient responds to the treatment. Also, the tumor markers homovanillic acid and vanillylmandelic acid can be used to assess the progress of therapy. In aftercare, tumor markers and radiologocial tests are used to not only rule out a relapse but also to notify about delayed side-effects of chemotherapy like cardiotoxic effects and audiologic damages.
Review Questions
Solutions can be found below the references.
1. What is the definition of a stage III neuroblastoma?
- Hematogenic metastases are present in organs.
- The tumor is infiltrating across the midline.
- The tumor has an intraspinal part, called hourglass tumor.
- The tumor is infiltrating adjacent areas but does not cross the midline.
- The tumor is infiltrating the bone marrow.
2. The parents of a 4-month-old girl notice the infant displays the features of raccoon eyes. They present the child in the children hospital, where the tentative diagnosis of a neuroblastoma with orbital metastases is made, stage IV-S. Consequently, a complete resection of the 5 x 4 x 4 cm intraabdominal tumor is performed. Immunohistochemical methods confirm the tentative diagnosis of the tumor being a neuroblastoma. A MYCN amplification cannot be found. Which further steps should be arranged?
- High-dose chemotherapy because of the metastases.
- Radiation of the area of resection.
- Radiation of both orbitae.
- Mega-chemotherapy with myelotoxic doses and consecutive bone marrow transplantation.
- Waiting for spontaneous regression.
3. The Kindbourne syndrome is NOT defined by…
- …cerebellar ataxia.
- …opsomyoclonus.
- …neuroblastoma.
- …myoclonia of trunk and extremities.
- …spontaneous nystagmus.



Comentários
Enviar um comentário