Practical Guide to Cardiovascular Examination (Cardiac Exam)
Table of Contents
Vital Measurements
You will likely require vital measurements for every patient you clinically examine. This will normally include heart rate, respiratory rate and blood pressure. These can be measured in most situations with basic equipment (a watch, a sphygmomanometer and a stethoscope) and constitute a part of a physician’s basic skill set.
It is very important that you learn to perform these examinations as well as the basic rules associated with each measurement. Some establishments (such as a hospital) will readily provide this data to you. Some establishments will provide temperature and oxygen saturation as well. Record this data and think about it as you complete the clinical examination of the heart.
The patient should be resting comfortably in the supine position. Access to the chest, arms, and legs is essential. Do not perform the exam through clothing; exposed skin is necessary. Having the patient dress in a hospital gown with a draping sheet available is recommended but not required.
Observation
With the anterior chest exposed, observe your patient’s thorax and the rest of their body. Look for the following: thorax, eyes, upper and lower extremities and jugular venous distention.
Thorax
- Scars indicative of cardiac surgery. A vertical scar down the sternum is an indication of an open heart surgery.
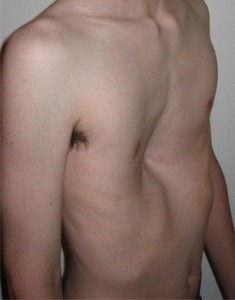
- Chest deformities including pectus excavatum (a sunken sternum and ribs, a symptom of several connective tissue diseases such as Marfan syndrome) and pectus carinatum(“pigeon chest”, a protrusion of the sternum and ribs).
Eyes
- Yellow plaques around the eyes and eyelids, called xanthelasma, are a sign of hypercholesterolemia; these are a risk factor for cardiovascular disease.
- Roth’s spots are observed on the retina with an ophthalmoscope. They appear as a red ring surrounding a white center. These are indications of infective endocarditis.
Image: “Xanthelasma palpebrarum” by Klaus D. Peter, Gummersbach, Germany. License: CC BY 3.0 DE
Upper and lower extremities
- Clubbing of the fingers or toes. The distal part of the digit flattens and widens. This is a sign of lung disease and a chronic hypoxemia.
- Cyanosis, blue discoloration of the digits implies poor perfusion. Cyanosis can be detected in the extremities or the lips.
- Image: “Splinter hemorrhages” by Splarka. License: Public DomainInfective endocarditis lesions on the hands and feet. Osler’s nodes are raised, painful, red lesions on the hands and feet. They are caused by immune complex deposition. Janeway lesions are small, red and painless. They are caused by microemboli. Splinter hemorrhages form vertically underneath the nails. They are also caused by small blood clots floating through the blood stream.
Image: “Example of clubbing, secondary to pulmonary hypertension, in a patient with Eisenmenger’s syndrome” by Ann McGrath. License: Public Domain
Jugular venous distention
The observation part of the cardiovascular exam includes observing the right internal jugular vein (IJV). This test is very useful to evaluate right heart function and central venous pressure.
Procedure
- Elevate the patients head between 15° and 30°.
- Identify the right internal jugular vein. This may take some practice. It crosses the deep to the sternocleidomastoid muscle and anterior to the right ear. Ask the patient to turn their head to the left or perform a valsalva maneuver. Additionally, use Hepato-Jugular Reflux to find the internal jugular vein. Apply firm pressure to the liver (right upper quadrant of the liver) for a few seconds and the IJV will fill with blood. Finally, a penlight can be very useful while trying to find the IJV.
- The IJV pulses, but so does the carotid artery. If the pulse rate matches the rate of the radial pulse, it is the carotid artery.
- Measure the top of the IJV fluid level in cm above the Angle of Luis (sternal angle). A normal measurement is a height of 3 cm above the sternal angle.
Image: “This photo represents obvious external jugular venous distention in a patient with severe tricuspid regurgitation. Note the ropy vein that courses almost vertical in this patient who is sitting almost upright.” by Ferencga. License: CC BY-SA 3.0
Palpation
The palpation portion of the cardiovascular exam includes evaluating the extremities and the carotid pulses as well as determining the point of maximum impulse (PMI) and evaluating it. A relatively strong vibration is created when the ventricles contract. This vibration is transmitted down the apex of the heart and into the chest wall. In a healthy individual the PMI is located at the 5th intercostal space along the left midclavicular line (just medial to and below the left nipple).
Evaluation of the extremities
Temperature
Evaluate the extremities for temperature. Gently touch the hands and feet to determine their temperature. A well perfused extremity will be slightly warm or at body temperature. A cold extremity indicates poor perfusion or blood may be shunted away from the skin. A warm extremity indicates a reduction of vascular resistance and may be a sign of septic shock.
Peripheral pulses
There are a variety of pulse points you should be familiar with. Some are regularly used (radial pulse, carotid pulse) and some are infrequently used (femoral pulse). A thorough cardiac exam requires an evaluation of all peripheral pulses. Always compare the paired pulses (is one stronger than the other, etc.) results.
- Carotid Artery
- Radial Artery
- Femoral Artery
- Popliteal Artery
- Posterior Tibial Artery
- Dorsalis Pedis Artery
Peripheral edema
Palpating the extremities is the preferred method to quantify peripheral edema. There are two types of edema: pitting and non-pitting.
Pitting edema will form indentations when palpated; you are effectively pushing fluid out of the tissue. Pitting edema is a sign of poor liver function or heart failure based on an abnormality of Starling’s forces. An injured, malfunctioning liver produces less albumin; this lowers the oncotic pressure of blood inside the capillaries, allowing fluid to pass into the tissue. An injured, malfunctioning heart produces less hydrostatic pressure on the blood in the capillaries with the same result. Extreme fluid overload is another cause of pitting edema.
Non-pitting edema is a completely different process involving metabolic factorresultin subcutaneous tissue swelling.
Procedure
- Starting with the hands, press firmly into the flesh of the palm. Continue up the forearm and arm until indentations no longer form. Pitting is measured by the following table:
- Report edema in numerical form at the highest point of detection (i.e., 2+ pitting edema at the height of the mid forearm.)
- Repeat for the lower extremity. Pitting edema usually occurs in the legs and feet well before the condition is sufficiently severe to result in edema of the hands and arms.
Point of maximal impulse (PMI)
Procedure
- Place the center of your palm at the PMI. The heel of your palm should rest at the sternal border. Your fingers should wrap around the patient laterally.
- Apply some pressure to the chest wall until you feel the heart beat in your palm.
- Identify the point of maximum impulse on the chest wall. It will be a small area, about 1 cm wide, with the strongest vibration.
Obesity will make this part of the exam difficult. Again, the PMI of a healthy person with a normal and healthy heart will be located near the 5th intercostal space, along the midclavicular line. The PMI of a dilated ventricle will be displaced laterally.
Thrill
A thrill may be detected if there is valvular disease present. This is a vibration associated with turbulent blood flow through a damaged or malformed valve. Thrills are located near the valve listening points as discussed below.
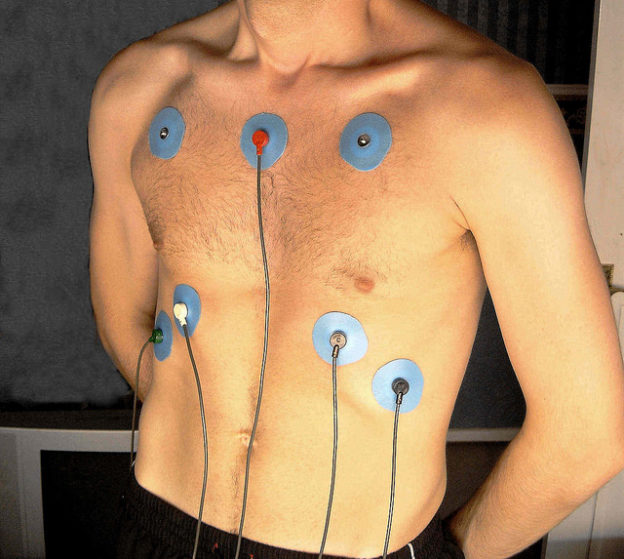
Auscultation
This part of the exam requires the use of your stethoscope. There are usually two sides to any stethoscope: the diaphragm and the bell. The bell is best used when auscultating low pitched sounds such as bruits (nonlaminar flow associated with stenosis) and some heart murmurs. The diaphragm is used to listen to most other sounds including high pitched sounds, breathing sounds, bowel sounds and normal heart sounds.
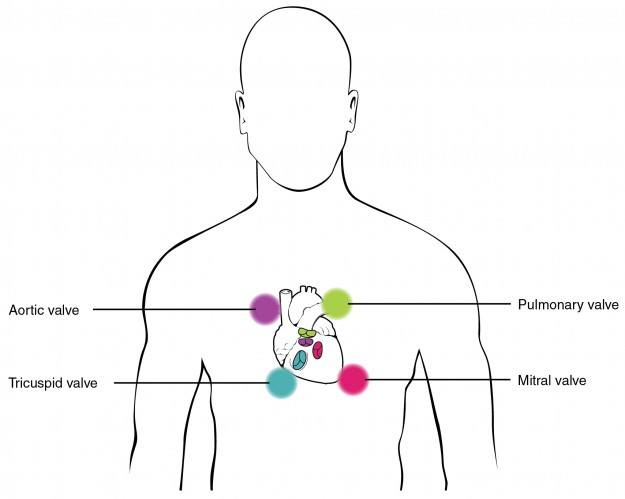
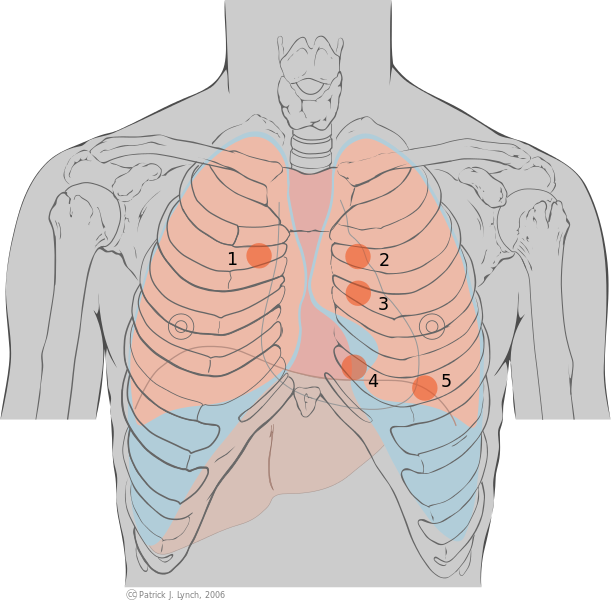
Familiarize yourself with the five listening points of the anterior chest wall. Each listening point corresponds to a specific heart valve sound. The listening points do not correspond to the physical location of each valve but to where the sound is conducted. Use the mnemonic of APT M:
Moving from the right 2nd intercostal space (A for aortic valve), to the left 2nd intercostal space (P for pulmonic valve) to the left 4th intercostal space (T for tricuspid valve) to the lateral aspect of the fifth intercostal space (M for mitral valve).
With the diaphragm, listen at each point for several seconds. Additionally, listen at the 3rdintercostal space near the left sternal boarder (Erb’s Point) where aortic and pulmonic sounds can be appreciated at the same time. Erb’s point is not used frequently.
At each listening point, you should be able to hear the two main heart sounds S1 and S2. Also, listen for the splitting of S1 and S2, the two gallop sounds S3 and S4 and any heart murmurs. S3 and S4 are very soft and may be appreciated better with the bell.
S1 is made of the tricuspid valve (T1) and mitral valve (M1) sounds and marks the beginning of systole. S1 does not normally split in a healthy heart. Myxoma, right bundle branch block and atrial septal defects can result in the splitting of S1.
S2 is made of aortic and pulmonic valve sounds and marks the end of systole and the beginning of diastole. S2 splits under normal physiological conditions and in several disease states. During inhalation, pulmonic valve closure is delayed. The aortic valve (A2) shuts first and then the pulmonic valve (P2) follows. The valves close in unison on expiration.
The third heart sound, S3, is “ventricular gallop” that immediately follows S2, in early diastole, during passive left ventricular filling. S3 is normal in patients under 40 years but is also associated with congestive heart failure. In both populations, the left ventricular wall may be compliant. This compliance allows for the S3 gallop. It is heard in ventricular septal defects, dilated cardiomyopathy and hypokinetic areas of the heart post-MI.
The forth heart sound, S4, is “atrial gallop” that follows S2 after a short pause, in late diastole, during active left ventricular filling. S4 is almost always abnormal. It is the result of a non-compliant left ventricle and is heard in hypertrophic ventricles, fibrosis and early phase of myocardial infarction.
Heart murmurs
Heart murmurs are sounds that are the result of turbulent flow across a heart valve due to a narrow path for the blood to flow (stenosis) or a damaged valve that allows blood to flow backwards (regurgitation).
An expert auscultator can discern a great deal about heart murmurs with a stethoscope. A medical student should be able to isolate the murmur to a specific valve, determine if it is a systolic or diastolic murmur and rate the sound on a scale from 1–6. A murmur with a rating of 1 is difficult to hear with a stethoscope. A murmur with a rating of 4 is easily discernable and is accompanied with a thrill. A murmur with a rating of 6 is audible without a stethoscope.
- Systolic murmurs occur during systole and include aortic stenosis, pulmonic stenosis, mitral regurgitation, tricuspid regurgitation and ventricular septal defect.
- Diastolic murmurs occur during diastole and include aortic regurgitation, pulmonic regurgitation, mitral stenosis and tricuspid stenosis.
Carotid auscultation
Ask the patient to hold their breath and listen over each carotid artery with the diaphragm. You are listening for carotid bruits, a high pitched rushing sound that indicates carotid artery stenosis. Never occlude both carotid arteries at the same time.





Comentários
Enviar um comentário