Narrow- and Broad Spectrum-Antibiotics
Table of Contents
Aminoglycosides
Aminoglycosides have played a major role in antimicrobial therapy since their discovery in the 1940s. The first aminoglycoside, the antibiotic streptomycin, was isolated from streptomyces griseus. Today, streptomycin is widely used for the treatment of tuberculosis.
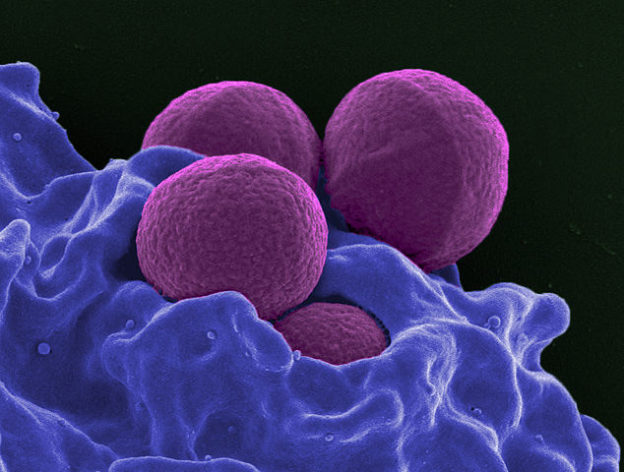
Image: “Gentamicin A”. License: Public Domain
The aminoglycoside gentamicin binds via an ionic binding to the bacterial cell surface. Gentamicin uptake into the bacterial cell depends on an electrochemical gradient across the bacterial cytoplasmic membrane. This electrochemical gradient cannot be maintained in anaerobic conditions and at a low pH, which is why the efficacy of aminoglycosides against anaerobes in a low-oxygen environment is markedly curtailed.
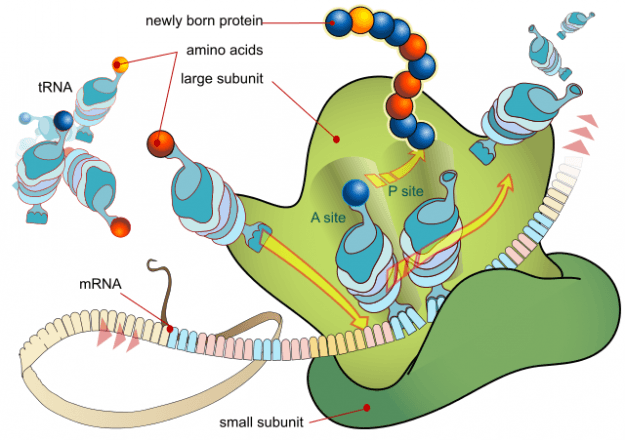
The effect of these antibiotics is based on an irreversible binding to the 30S subunit of the ribosome complex and, thus on the inhibition of protein biosynthesis. Aminoglycosides attack rapidly multiplying organisms, but also kill dormant bacteria.
Image: “Ribsosome mRNA”. License: Public Domain
Absorption of oral aminoglycosides is not good. Effective, clinically relevant concentrations are not achieved in respiratory secretions or cerebrospinal fluid. Aminoglycosides are eliminated via the kidney. Adjustment of aminoglycoside dosage is needed in patients with renal failure.
Aminoglycosides are contraindicated in pregnancy or deafness, as aminoglycosides accumulate in the endo- and perilymph of the inner ear. Aminoglycosides also exhibit a significant post-antibiotic effect (PAE), which means they persistently suppress bacterial growth even after only a brief exposure to the antibiotic.
Aminoglycosides are effective against enterobacteriaceae and pseudomonas. Many other bacteria such as enterococci, streptococci and legionella are resistant to aminoglycosides.
Recommended antimicrobial treatment of infections such as endocarditis, osteomyelitis burnsis a combination of aminoglycosides with other antibiotics such as β-lactams or fluoroquinolones. Tobramycin is the drug of choice for the treatment of pseudomonas aeruginosa infections. Amikacin, however, is a reserve aminoglycoside used in the treatment of immunosuppressed patients suffering from severe infections.
Tobramycin inhalation solution is currently the only aerosol antibiotic approved for the long-term treatment of chronic infections caused by pseudomonas aeruginosa in patients with cystic fibrosis (CF) and chronic obstructive pulmonary disease (COPD).
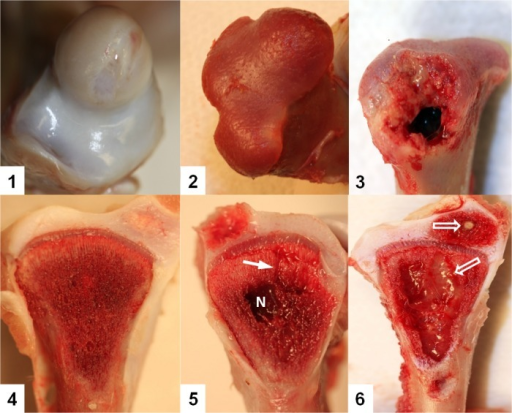
Topically applied aminoglycosides, for example neomycin and kanamycin, are used for treating skin and mucous membrane infections caused by staphylococci and enterobacteriaceae. Gentamicin is also successfully used against bone and soft tissue infections in prosthetic surgery. It is locally applied in the form of gentamicin-loaded PMMA beads or gentamicin bone cement.
Macrolides
Macrolide antibiotics all contain a lactone ring. They have poor chemical stability in aqueous solution (acid-labile) and also have a very unpleasant, bitter taste, which is why they are usually present in esterified or galenical form. Macrolides are administered as enteric-coated tablets, as the intravenous administration is poorly tolerated.
Macrolides target bacterial protein synthesis by inhibiting ribosomal translocation. Macrolides are bacteriostatic antibiotics and effective against many strains of gram-positive bacteria such as streptococci and clostridia.
Because macrolides are able to penetrate host cells, they can also target intracellularpathogens, for example chlamydia, bordetella pertussis and legionella. Only in the cerebrospinal fluid, insufficient concentrations of macrolides are reached. Macrolide antibiotics and their active metabolites are excreted mainly in the bile.
Macrolide antibiotics may cause gastrointestinal side effects and intrahepatic cholestasis, which is why they are contraindicated in liver disease.
Erythromycin and roxithromycin
Image: “Legionellen”. License: Public Domain
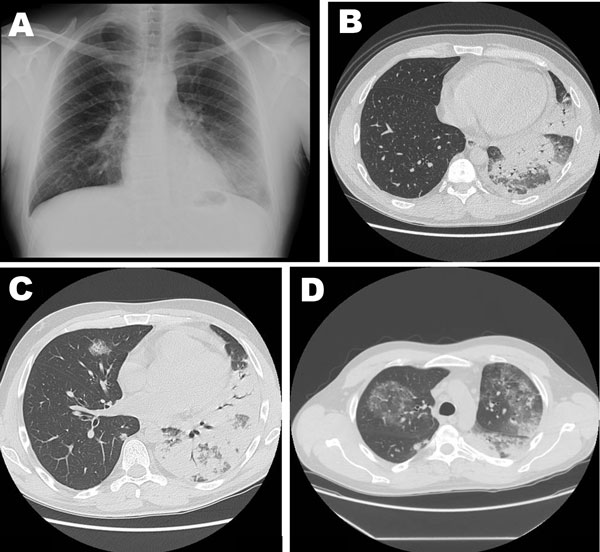
Erythromycin, a macrolide antibiotic, is the drug of choice for the treatment of legionnaires’ pneumoniaand pertussis (catarrhal phase). Erythromycin is effective in the treatment of acute infections of the respiratory tract, for example acute pneumonia caused by pneumococci and other infections caused by mycoplasma pneumoniae.
Moreover, erythromycin is most effective in the treatment of campylobacteriosis.
Image: “Severe Pneumonia Caused by Legionella pneumophila Serogroup”. License: Public Domain
Roxithromycin is an antibiotic used in the treatment of respiratory tract infections including pneumonia, as well as skin and soft tissue infections. Its pharmacokinetic properties are better than those of erythromycin.
Clarithromycin and Azithromycin
Azithromycin and clarithromycin are semisynthetic analogues of erythromycin and have better oral absorption and a lower side effect profile. Clarithromycin is used mainly in combination with other antibiotics for the treatment of helicobacter pylori infections and for the prophylaxis of bordetella pertussis infections.
Telithromycin
Telithromycin is also a semisynthetic erythromycin derivative. It belongs to a new chemical class of antibiotics called ketolides. It targets enterococci and macrolide-resistant pneumococci, which is why telithromycin is used in the treatment of respiratory infections caused by macrolide-resistant strains of bacteria. This drug has many side effects such as QT prolongation, CNS disorders and liver failure.
Tetracyclines
Doxycycline is the most frequently prescribed tetracycline. It is bacteriostatic and inhibits protein synthesis. It prevents the attachment of the tRNA to the 30S subunit of the ribosome. Doxycycline is most efficient against obligate intercellular parasites such as chlamydia and rickettsia.
Doxycycline can be administered orally or parenterally. However, many foods such as milk and iron products interfere with doxycycline, making it less effective by reducing its absorption rate dramatically. Tetracyclines can cross the blood-brain barrier to some extent.
Tetracyclines are predominantly metabolised in the kidneys. In patients with renal impairment this may lead to excessive accumulation of the antibiotic and can potentially cause hepatic damage. Common side effects include gastrointestinal disturbances and photosensitivity.
Contraindicated in pregnant women and children because tetracyclines have chelating effects on calcium, which may cause discoloration of teeth and an increased susceptibility to caries and delayed bone growth.
Many bacteria such as streptococcus, clostridium, enterobacteriaceae and gonococcus are resistant to doxycycline. They have developed bacterial efflux pumps that remove the antibiotic from the bacterial cell. Since tetracyclines are no longer used in the production of meat, a decline in tetracycline resistance has been observed.
Doxycycline is the drug of choice for the treatment of chlamydial infections. It is also useful in the treatment of human brucellosis, leptospirosis, lyme disease (not neuroborreliosis) and mycoplasma pneumoniae. Furthermore, it is one of only a few selected drugs that has been used for the treatment of malaria tropica caused by chloroquine-resistant plasmodium.
Nitroimidazoles
Metronidazole and other nitroimidazoles are prodrugs, activated within the microbial cell by oxidoreductases under anaerobic conditions. It is a bactericidal antibiotic active against anaerobic bacteria and selected parasites. Its mode of operation is not fully understood. It is believed that nitroimidazoles produce short-lived free radicals, which are cytotoxic and can interact and harm bacterial DNA.
Metronidazole is well absorbed and distributed after oral administration, reaching high and effective tissue concentrations in the brain, uterus, liver and abscess cavities. Metronidazole is indicated for the treatment of infections caused by protozoa and obligate anaerobes, such as bacterial vaginosis and clostridium difficile-associated diarrhea.
Metronidazole is used for perioperative antibiotic prophylaxis. It is oxidised and conjugated in the liver and partially excreted in the urine. It is contraindicated during pregnancy and in patients with severe hepatic disease.
Anaerobes have evolved different mechanisms of resistance. Specific resistance genes (nim) confer resistance to metronidazole by encoding an alternative reductase that can convert nitroimidazole to a nontoxic derivative.
Fosfomycin
Fosfomycin is a phosphonic acid derivative that irreversibly inhibits murein precursor synthesis. Due to its good soft tissue penetration and the broad spectrum of activity, it is used as a reserve antibiotic in the treatment of osteomyelitis and soft tissue infections. Renal excretion occurs via glomerular filtration. No tubular secretion occurs.
Fosfomycin should be used in combination with other bactericidal antibiotics to prevent development of resistance. Common side effects of fosfomycin include nausea or vomiting. The infusion solution contains high concentrations of sodium and recrystallised succinic acid, which must be considered in the treatment of patients with hypernatremia and allergies.
Trimethoprim-Sulfonamide-Combinations
Image: “Pneumocystis jeroveci Pneumonie” by Yale Rosen. License: CC BY-SA 2.0
Cotrimoxazole is the combination of trimethoprim and a sulfonamide. It is used for prophylaxis of AIDS-related infections like pneumocystis jirovecii infections and in cancer patients.
Cotrimoxazole inhibits tetrahydrofolic acid production, which is needed for the synthesis of nucleic acids and amino acids. As trimethoprim and sulfonamides act synergistically, cotrimoxazole is bactericidal. Cotrimoxazole achieves adequate concentrations in the cerebrospinal fluid, bronchial secretions and sputum.
Cotrimoxazole is eliminated by the kidneys. Cotrimoxazole is contraindicated in patients with renal impairment, in glucose-6-phosphate dehydrogenase deficient patients and during pregnancy.
Chloramphenicol
Chloramphenicol is a phenylalanine derivative which blocks bacterial protein biosynthesis. This bacteriostatic antibiotic inhibits the attachment of the tRNA to the ribosome and has a broad spectrum of activity. It targets a wide variety of both gram-positive and gram-negative bacteria (except pseudomonas aeruginosa).
Chloramphenicol is characterized by good tissue penetration. It reaches high, effective concentrations in the cerebrospinal fluid and aqueous humor. However, chloramphenicol also has undesirable, life-threatening adverse effects. The incidence of irreversible aplastic anemiaand more commonly reversible bone marrow suppression are estimated to be 1: 10,000.
Chloramphenicol cannot be glucuronidated by the immature neonatal liver. Thus, toxic levels accumulate. Chloramphenicol induces Gray baby syndrome, which is a state of cardiovascular collapse, involving hypothermia, respiratory failure and circulatory collapse, which often leads to death. Therefore, the use of chloramphenicol is only recommended for the treatment of life-threatening ocular infections, brain abscesses and severe salmonellosis.
Streptogramins
Streptogramin and pristinamycin belong to a relatively new class of substances, the streptogramins. Like macrolides and lincosamide, they inhibit the peptidyl transferase activityof the 50S ribosomal subunit (elongation inhibition). Streptogramin can also be bactericidal; a component of the antibiotic modifies the conformation of the ribosome, so that only the active component of the antibiotic can bind there.
Streptogramins are effective in the treatment of infections caused by gram-positive bacteria, including MRSA. Enterobacteriaceae are resistant to these antibiotics.
Oxazolidinones
Oxazolidinones are also a new class of synthetic antibiotics, and are not related to any other class of antibiotics. Hence, oxazolidiones do not exhibit cross-resistance or cross-allergies with other antimicrobial agents. Oxazolidiones inhibit protein biosynthesis, however, the exact mode of action is still unknown.
They act as bacteriostatic agents against gram-positive bacteria, including MRSA, VRE and penicillin-resistant pneumococci. But they do not target gram-negative pathogens. Oxazolidinones are formulated for both oral and parenteral administration, both of which produce few adverse effects. It should be noted, that oxazolidiones have a weak inhibitory effect on monoamine oxidase (MAO). Therefore, the use of oxazolidione antibiotics may cause adverse interactions in patients treated with antidepressants. Particularly, symptoms like low blood pressure, increase of temperature and confusion should be monitored.
Linezolid is used for the treatment of infections such as pneumonia or skin and soft tissue infections caused by resistant gram-positive bacteria.
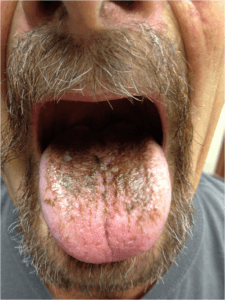
Linezolid is not approved for and should not be used in the treatment of children and is not recommended in patients with depression or malignant hypertension, as in pheochromocytoma or thyrotoxicosis. Possible side effects include vomiting, diarrhea, discoloration of the tongue and pancytopenia, which is why the blood count should be monitored once per week.
Lincosamides
Clindamycin is the best known lincosamide antibiotic and the only one in clinical use. By affecting the peptidyl transferase reaction, clindamycin inhibits bacterial protein synthesis and has a bacteriostatic effect. It is highly effective against several types of bacteria such as staphylococci, streptococci (also pneumococci) and anaerobic bacteria belonging to the genera Bacteroides, Actinomyces, and Propionibacterium and Clostridium perfringens. Other Clostridium spp. and all aerobic gram-negative rods are resistant to clindamycin.
Clindamycin is readily absorbed from the gastro-intestinal tract and reaches significant, clinically relevant concentrations in bone and other tissues. It undergoes metabolism in the liver, which is why clindamycin therapy has been linked to symptoms like jaundice and elevated hepatic enzyme levels. Clindamycin-based drugs contain high levels of benzyl alcohol so clindamycin should not be administered during pregnancy and the first months of life.
Clindamycin resistance is based on modifications of the ribosomal binding site and inactivating nucleotidyltransferases. In addition, the cell wall of gram-negative bacteria is impermeable to clindamycin.
Clindamycin is associated with a high risk of antibiotic-associated enterocolitis (C. diff colitis), so it is used exclusively in the treatment of serious anaerobic infection, such as abscesses, intra-abdominal infections, osteomyelitis, or dental and gynaecological infections.
Review Questions
The answers can be found below the references.
1. Which of these antibiotics is suitable for the treatment of soft tissue infections with MRSA?
- Gentamicin
- Benzylpenecillin
- Erythromycin
- Doxycycline
- Linezolid
2. A 33-year-old man presents while you are on duty in the emergency room. You diagnose sepsis and incipient multiple organ failure. The patient indicates to have been in Kenya and to have had no malaria prophylaxis in recent weeks. Since there is no chloroquine stocked in your hospital, you decide to combine quinine with which antibiotic for initial therapy?
- Doxycycline
- Erythromycin
- Rifampicin
- Azithromycin
- Metronidazole
3. Rapid intravenous administration of which antibiotic is associated with a risk of neuromuscular blockade or acute respiratory failure?
- Clindamycin
- Chloramphenicol
- Gentamicin
- Ceftriaxone
- Cotrimoxazole





Comentários
Enviar um comentário