Prolactinoma — Diagnosis and Treatment
Table of Contents
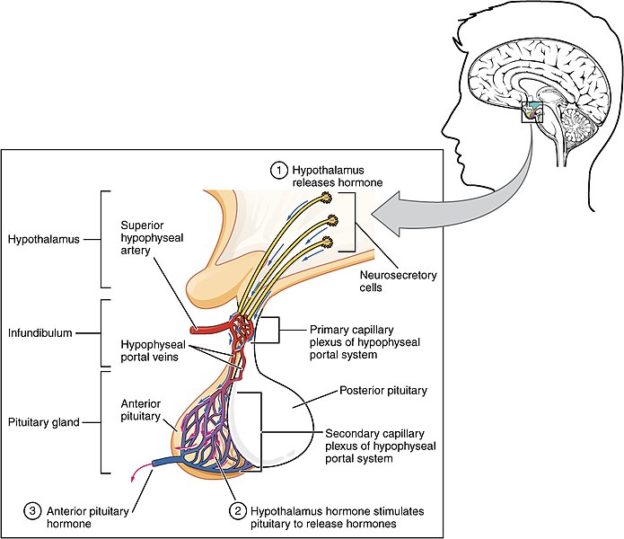
Image: “The Anterior Pituitary Complex” by OpenStax College. License: CC BY-SA 3.0
Definition of Prolactinoma
Prolactinoma are the most common hormone secreting pituitary tumours occurs due to neoplastic transformation of the anterior pituitary lactotrophs. They are benign non-cancerous tumours, and rarely become malignant.
Depending on the size, they are classified as:
- Microprolactinomas: < 10mm, these are common in premenopausal women.
- Macroprolactinomas: > 10 mm, these are common in men and post-menopausal women.
Epidemiology of Prolactinoma
Prolactinoma account for 25—40 % of all pituitary adenomas in USA. They occur in child-bearing years (second and third decade of life)*. Microprolactinoma is common than macroprolactinoma. They can cause significant morbidity (due to local mass effect of a macroprolactinoma), though mortality is unlikely.
Sex distribution
Both men and women are equally affected. About 90 % of females present with microprolactinoma, whereas 60 % of males present with macroprolactinoma. This is because symptoms occur earlier in women, menstrual irregularities are the common symptom for which a woman consults a physician and this leads to earlier diagnosis of the prolactinoma. On the other hand, males tend to present late as the symptoms of hypogonadism are nonspecific initially.
Males also consult physicians when they have had space occupying lesion effects. By then, the tumour has enlarged to form a macroprolactinoma. Children are rarely affected by prolactinioma.
Etiology of Prolactinoma
Etiology of prolactinoma is obscure. Most of the prolactinomas occur sporadically, but there can be a genetic predisposition to develop them as well. Prolactinoma can occur as part of MEN Type 1 (multiple endocrine neoplasia) along with pancreatic islet cell tumours and parathyroid tumours. This is an autosomal-dominant genetic disorder. Familial isolated pituitary adenoma (FIPA) has an autosomal-dominant inheritance and accounts for 2-3% of pituitary tumours.
A mutation in the aryl hydrocarbon interaction protein gene has been identified in 25% of FIPA family members, and these adenomas are predominantly prolactinomas and somatotropinomas.
Pathophysiology of Prolactinoma
Prolactin, a polypeptide hormone is secreted by the lactotrophs of the anterior pituitarygland. Prolactinoma are anterior pituitary lactotrophtumour which results in excess synthesis and secretion of tumours. This tumor is a true neoplasm that has monoclonal cell origin.
Prolactin acts on the mammary glands and facilitates mammogenesis (growth and development of the mammary gland), lactogenesis (secretion of milk) and galactopoiesis (maintenance of milk secretion). It has a role in the synthesis of progesterone and luteal cell hypertrophy during pregnancy and influences reproductive behaviour. Prolactin plays an important role in homeostasis by regulating the immune system, maintaining osmotic balance and facilitating angiogenesis .
Prolactin releasing factors (PRFs) and prolactin inhibitory factors (PIFs) are the hypothalamic factors that regulate prolactin secretion. Dopamine is the most important PIF that causes tonic inhibition of prolactin secretion. This is in contrast to other anterior pituitary hormones which are controlled by the hypothalamic releasing factors. TRH (thyrotropin releasing hormone) and VIP (vasoactive intestinal peptide) stimulate prolactin secretion.
It is hypothesised that dopamine may have a role in the pathogenesis of prolactinomas. Certain antipsychotic drugs deplete the dopamine stores in the brain or interfere with the effects of dopamine at the pituitary gland result in secretion of prolactin.
Hyperprolactinaemia is a state where there is an increase in prolactin level. In addition to prolactinoma, hyperprolactinaemia can be caused by a pathologic problem of the hypothalamic-pituitary-dopaminergic pathway or certain drugs. Idiopathic hyperprolactinemia is a possibility and is a diagnosis of exclusion. Many drugs such as trifluoperazine, haloperidol, risperidone, molindone, metoclopramide, verapamil can cause hyperprolactinemia.
Symptoms of Prolactinoma
Prolactinoma can cause symptoms either due to the effects of increased prolactin levels or due to space-occupying lesion effects. The symptoms depend on the duration, size of prolactinoma as well as age and sex of the patient.
Hormonal Symptoms
Women:
Reproductive age females: They commonly present with menstrual disturbances such as oligomenorrhea, amenorrhoea or irregular menstrual cycles. Women may present with infertility These symptoms are due to suppression of GnRH (gonadotrophin releasing hormone) by the elevated prolactin.
Galactorrhoea: This is seen in 30—80 % of women. It can be spontaneous or expressive (seen only when nipples are squeezed). This is due to direct physiologic effect of prolactin on the breast epithelial cells.
Other symptoms are:
- Due to low oestrogen levels, women may complain of vaginal dryness and/or
- In young girls, there can be delayed menarche.
- Prolactin tumors may become large in size and compress the nearby hormone secreting cell of pituitary such as TSH, GH, etc. to induce other hormonal diseases.
Men:
- Men usually present with decreased libido, erectile dysfunction or infertility.
- Rarely, they may present with galactorrhoea or gynaecomastia.
- Patients may also uncommonly present with loss of musculature and body hair.
- In pre-pubertal boys, prolactinoma may result in small testicles and female body habitus.
- Eye problems and headache due to delay in appearance of symptoms.
Sexual dysfunction could be either due to hyperprolactinaemia or a combination of hyperprolactinaemia and low testosterone levels (secondary hypogonadism). Elevated prolactin suppresses the GnRH, leading to decrease FSH and LH secretion, thereby leading to decreased testosterone levels. Sexual dysfunction is seen both in males and females.
Elevated prolactin levels lead low bone mineral density causing osteopenia or osteoporosis. Elevated prolactin has a direct effect on bone leading to increased bone turnover in both sexes.
Space-occupying lesion symptoms:
These are mainly seen with macroprolactinoma. The space-occupying lesion effects of prolactinoma are similar to other brain tumours. Patients commonly present with headache and visual field defects. When the prolactinoma compresses the optic chiasma, it results in bitemporal hemianopia. This is the common visual disturbance of prolactinoma.
Macroprolactinoma can also compress the surrounding normal functioning pituitary tissue, resulting in deficiency of TSH, GH and ACTH.
Diagnosis of Prolactinomas
Blood tests
- Prolactin: Its secretion depends on the size of the tumour, the greater the size of the adenoma the higher the prolactin levels. If levels are only modestly increased, the test needs to be repeated again. Usually a fasting sample is needed. Commonly prolactin levels are greater than 250 ng/ml, and levels greater than 500 ng/ml are diagnostic of macroprolactinomas.
- Growth hormone can be evaluated as some prolactinomas can secrete growth hormone.
- Urine or serum pregnancy test is performed to identify if patient is pregnant.
- Serum TSH may be increased. Prolactin may be elevated secondary to increased TRH. Free T4 levels are measured too.
- FSH and LH may be decreased.
- Testosterone levels may be decreased.
- If adrenal insufficiency is suspected, basal and cosyntropin stimulated cortisol levels are measured.
- If patient has symptoms of acromegaly, insulin like growth factor-1 is measured.
- Liver function tests, serum urea and creatinine are measured to assess for liver or kidney failure.
Imaging studies
- MRI with gadolinium enhancement can identify small lesions (as small as 3—5 mm) and is better for soft tissue delineation.
- CT with contrast can identify bone destruction better than MRI.
- Rarely, biopsy of the lesion is indicated when there is diagnostic uncertainty.
Differential Diagnosis
The following are the differentials for hyperprolactinaemia:
- Pregnancy and puerperium
- Primary hypothyroidism
- Drugs: Phenothiazines, haloperidol, metoclopramide, tricyclic antidepressants, cocaine, opiate abuse, methyldopa, reserpine, verapamil, etc.
- Adrenal insufficiency
- Chronic renal failure
- Liver cirrhosis
- Breast stimulation
- Chest wall lesions, trauma or surgery
- Spinal cord lesions
- Hypothalamic or pituitary causes: Growth hormone secreting adenoma, non-functioning adenoma, pituitary stalk compression, meningioma, craniopharyngioma, dysgerminoma, etc.
- Previous radiation to hypothalamic or pituitary region
- Idiopathic causes.
Treatment of Prolactinoma
Most microprolactinoma (up to 95 %) do not progress to macroprolactinoma. Hence patient with a microprolactinoma having minimal symptoms can be closely followed with serial prolactin levels and CT/MRI scans yearly. On the other hand, if a patient with microprolactinoma is symptomatic, then it needs to be treated. Patients with macroprolactinoma need treatment as it may grow compressing the surrounding structures.
Medical management
Bromocriptine is a dopamine agonist and decreases the synthesis and secretion or prolactin. It reduces the rate of tumour cell division and also decreases the growth of the individual cells. It is usually given orally, twice a day, starting at a dose of 1.25 mg, and gradually increased, normally doses greater than 7.5 mg are not needed except in macroadenomas. Side effects include nausea, nasal stuffiness, depression, psychosis and orthostatic hypotension
Female patients intolerant to even small doses of oral bromocriptine can be prescribed intravaginal bromocriptine, it provides same efficacy as the oral route.
After initiating treatment, prolactin levels return to normal levels within a few days—weeks in microprolactinoma in 80—90 % of patients.
In microprolactinoma, bromocriptine treatment results in shrinkage of tumour size in about 80—85 % of patients.It result in return of normal functioning of gonads. But in contrast to macroprolactinoma, the prolactin levels do not reduce to normal levels. Further, the shrinkage in tumour size does not correlate well with prolactin levels. As the tumour shrinks, pituitary function improves as evident by increased serum testosterone levels and increased sperm count in males. Patient should be monitored regularly by clinical symptoms and signs, prolactin levels and radiological changes.
The adverse drug reactions of bromocriptine are dizziness, nausea and nasal stiffness and orthostatic hypotension.
Patients who do not respond, or are intolerant to bromocriptine can be given cabergoline. It can be given twice a week due to its long half-life. It has a superior efficacy than bromocriptine in reducing prolactin levels and tumour shrinkage. Side effects are less than bromocriptine which include nausea, headache, fatigue and dizziness.
In women presenting with infertility secondary to prolactinoma, as prolactin levels normalize, the gonadal function also recovers and menstruation returns within a few months. Sometimes, the woman may become pregnant even before the appearance of menstrual cycle, hence patients are advised to use barrier methods of contraception until normal menstrual cycles resume. This helps to correctly assess the timing of conception, and also helps the physician to withhold the medical management upon conception.
Surgery
Trans-sphenoidal pituitary adenoidectomy is the surgical treatment of choice in patients with dopamine agonist treatment resistant microprolactinoma (despite being treated with maximum tolerated dose), patients with macroprolactinoma and patients with large cystic or haemorrhagictumours.Transcranial resection of pituitary tumor is favorable only in the patients that have large extrapitutary extension.
Radiation treatment
Radiation is rarely used as a primary treatment to manage prolactinoma, and is used only in patients where there is rapid tumour regrowth despite medical and surgical treatment or in case of malignant prolactinoma. Complications include hypopituitarism (12-80%), optic nerve damage and neurologic dysfunction.
Management of resistant prolactinoma
In patients having resistant prolactinoma and persistent hyperprolactinemia despite medical treatment, surgical debulking and with or without radiation therapy, temozolomide (for malignant prolactinoma) can be used. It is a chemotherapeutic alkylating agent and has been shown to reduce prolactin level and reduce tumour growth.
Even after regression of the tumor, periodic monitoring of the PRL levels is suggested to the patient to prevent re-growth of prolactin tumors.
Prolactinoma in Pregnancy
During pregnancy normal pituitary gland doubles in size and prolactin levels increase 10 fold; hence it is not advisable to check prolactin levels for management of prolactinoma.
Management of prolactinoma should begin prior to conception, and the woman and her partner should be appropriately counselled. The main risk to the woman is enlargement of prolactinoma and exposure of dopamine agonists to the foetus.
The risk of enlargement of microprolactinoma during pregnant is low. On the other hand macroprolactinoma can enlarge during pregnancy due to hormonal stimulation of lactotrophs. Hence the tumour needs to be shrunk either by dopamine agonist treatment or surgery before the woman becomes pregnant.
Bromocriptine can be used pre-conceptually due to its relative safety record. Once pregnancy is confirmed, dopamine agonist therapy should be stopped as they cross placenta and safety due to continued usage during pregnancy has not been studied.
During pregnancy, woman must be followed every 3 months and specifically asked about headache and visual symptoms. Visual field testing and MRI should be performed. If MRI reveals that prolactinoma enlargement (macroprolactinoma) is responsible for the visual field defect, the patient can be started on dopamine agonist therapy with bromocriptine for the rest of the pregnancy.
If the adenoma does not respond to bromocriptine, then cabergoline can be prescribed. Cabergoline is more efficacious and better tolerated than bromocriptine in treatment of prolactinomas in pregnancy. If cabergoline is also not successful and vision is severely compromised then transsphenoidal surgery can be performed in the second trimester. If woman is already in the third trimester, then surgery is deferred until the delivery.
Breast feeding can be advised as there is no evidence that breastfeeding stimulates growth of the tumour. In women who wish to breast feed, dopamine agonists must be withheld as they impair lactation.
Review Questions
The answers can be found below the references.
1. A 55-year-old man presents with headache, loss of libido and visual symptoms. A MRI scan revealed a 13 mm pituitary adenoma and prolactin levels were elevated. Which of the following visual field defect is most likely to experience by the patient?
- Tunnel vision
- Monocular visual loss
- Homonymous hemianopia
- Bitemporal hemianopia
2. A 35-year-old woman presents to the doctor with infertility. On investigations, she was found to have elevated prolactin levels and microprolactinoma. She was started on bromocriptine, but the woman experienced severe side effects. Which of the following is the next best treatment strategy?
- Transsphenoidal surgery
- Cabergoline
- Radiation treatment
- Temozolamide
3. A female with prolactinoma is least likely to exhibit which of the following symptoms?
- Loss of libido
- Menstrual irregularities
- Dysmenorrhoea
- Infertility
Comentários
Enviar um comentário