Testicle Pain in Young Boys — Symptoms and Treatment
Table of Contents
- Anatomy and Development of the Testicles
- Epidemiology of Testicle Pain in Young Boys
- Etiology and Pathophysiology of Testicle Pain in Young Boys
- Diagnosis of Testicle Pain in Young Boys
- Clinical Features of Testicle Pain in Young Boys
- Laboratory Investigations of Testicle Pain in Young Boys
- Imaging of Testicle Pain in Young Boys
- Differential Diagnoses of Testicle Pain in Young Boys
- Treatment of Testicle Pain in Young Boys
- Progression and Prognosis Testicle Pain in Young Boys
- Review Questions
- References
Image: “Sad Child Boy Kid Crying Tears Sadness Mood” by PublicDomainPictures. License: Public Domain
Anatomy and Development of the Testicles
An understanding of the basic anatomy and the development of the testicles is necessary in this discussion:
Before birth, the male testicles are intra-abdominal organs that migrate to the post-embryonic position via migrating down through the abdomen into the scrotum. The connection between the testes and the abdomen is maintained by the spermatic cord, which includes vital blood vessels, nerves, lymphatic vessels as well as the deferens. This connection creates a weakness for the development of various anomalies.
On the upper, outer, back position of the testicle lies a connected but separate structure called the epididymis, which serves to store and transport sperm.
Epidemiology of Testicle Pain in Young Boys
Testicular torsion is a common surgical emergency in the pediatric population, annually affecting almost 4 per 100,000 males younger than 18 years. It accounts for 10–15% of acute scrotal diseases in children. Its peak incidence is during puberty; however, it can occur at any age. Approximately, 42% of boys with testicular torsion have to undergo orchiectomy.
The hydatid torsion, also known as a torsed appendix testis is painful but is benign. Hydatid torsion or a torsed appendix testis tends to happen around 10 years of age and testicular torsion is usually seen in adolescent males.
Epididymitis is rare before puberty; after puberty, the incidence increases, and it becomes important in the differential diagnosis of an acute painful scrotum in young sexually active men.
Varicocele is found in 5–15% of adolescent boys. It is extremely rare in boys younger than 10 years of age. They may be unilateral or bilateral, but in most cases, they are unilateral and found on the left side. Approximately, one-fifth of adolescents with a varicocele will experience fertility problems.
Etiology and Pathophysiology of Testicle Pain in Young Boys
In neonates, when the testis has not yet become attached to tunica vaginalis, mobility of the testis can cause a predisposition to ‘extravaginal’ testicular torsion.
In approximately 12% of males, the attachment of the testis to the tunica vaginalis is inappropriately high – known as ‘bell clapper’ deformity. Such deformity makes the spermatic cord more susceptible to torsion, i.e. twisting. When the testis rotates more than 90°, blood flow to the testis can be compromised leading to swelling and ischemia of the testis. This is called ‘intravaginal’ testicular torsion.
Escherichia coli is the most common organism causing acute epididymo-orchitis in children. In sexually active men, chlamydia trachomatis is the most common cause followed by other organisms such as neisseria gonorrhoeae, treponema pallidum, trichomonas, gardenerella vaginalis, etc., but the organism is often undetermined. Mumps, coxsackie virus A, echoviruses, varicella, adenovirus, enterovirus, etc cause viral epididymitis. Tuberculous epididymis occurs in endemic areas.
Varicocele involves an abnormal dilation of the pampiniform plexus, which is a venous plexus, in the scrotum. This is described as a ‘bag of worms’. The pampiniform plexus dilation occurs because of valvular incompetence of the internal spermatic vein. The exact etiology of a varicocele remains unclear, however. Theories include the congenital absence of valves, increased pressure or increased length of the left testicular vein, and an abnormal, asymmetrical pattern in the venous drainage of the testes.
It is more common on the left side because of the angle made at the junction of the left testicular vein and the left renal vein, the absence of valve at the junction, and the compression of the renal vein between the superior mesenteric artery and the aorta (nutcracker effect) leading to increased venous pressure in the left testicular vein.
Diagnosis of Testicle Pain in Young Boys
When a young patient presents with an acute pain in the scrotum, along with scrotal swelling, the primary diagnoses to be considered include torsion (of the testes or testicular appendage), epididymitis, and incarcerated inguinal hernia. After they are ruled out, other diagnoses such as varicocele must be considered (see section Differential Diagnoses).
It is crucial to promptly identify and treat testicular torsion, because, in 4–8 hours, a serious ischemic damage can occur, which can affect sperm production and cause testicular loss. Incarcerated inguinal hernia is also a surgical emergency.
Clinical Features of Testicle Pain in Young Boys
The diagnosis can be gleaned from the patient’s history and physical examinations. Patients with torsion of the testis or testicular appendage usually present within 12 hours of the onset of pain, while those with epididymitis usually present after 12 hours. Patients with all three conditions can present with a history of similar episodes (of pain). Other general symptoms include nausea and vomiting (more common with torsion) and dysuria and fever (more associated with epididymitis).
In testicular torsion, tenderness is usually diffuse in torsion with the cremasteric reflex typically being absent on the ipsilateral side. It will start off as red and then turn blue and, if left alone, will turn black which means it is now dead and necrosed. The patient’s testicle will have a high lie (High yield information for USMLE).
In epididymitis, the tenderness is localized, over epididymis, and the cremasteric reflex is usually present.
In some patients with torsion of a testicular appendage, a blue dot sign is seen. This is a common finding in appendix testis.
Laboratory Investigations of Testicle Pain in Young Boys
Although a thorough clinical history and examination can give good clues to the diagnosis, additional testing may still be necessary. A urinalysis and culture are frequently done: presence of pyuria and bacteria in the urine is more diagnostic of epididymitis. If the boy is postpubertal and sexually active, a urethral swab should be taken for culture.
Other laboratory investigations that should be done if epididymitis is suspected involve checking for leukocytosis, staining, and culture of urethral discharge if present, and other specific tests for detecting Neisseria gonorrhoeae and Chlamydia trachomatis.
Imaging of Testicle Pain in Young Boys
Color Doppler ultrasonography (preferably high-resolution) is often performed to help with the diagnostic process, as it evaluates the testicular blood flow, i.e. whether the flow is normal, increased, or decreased. Color Doppler ultrasonography is also helpful when there is a hydrocele or when an abnormality of the testis is found on palpation.
In the case of testicular torsion, color Doppler ultrasonography may show no blood flow within an enlarged, often heterogeneous testicle. In the case of torsion of a testicular appendage, the findings may be a discrete appendage or increased blood flow to the testis or epididymis and, in the case of epididymitis, increased blood flow to an enlarged epididymis is usually seen, with a thickened scrotal wall.
In the hands of experienced operators, this type of ultrasonography has great results, with an accuracy of >95% [sensitivity 89.9%, specificity 98.8%, and false-positive rate 1%]; however, it is not used for a definitive diagnosis but mainly to determine if a urologic consult is indicated.
Radionuclide imaging can also be used (which shows ‘hot spots’ in areas with increased blood flow and ‘cold spots’ in areas with decreased blood flow), but color Doppler ultrasonography is more easily available, faster, and does not involve exposure to radiation, so the latter is the modality of choice to aid in the diagnosis of acute scrotum.
In the case of varicocele, ultrasonography should be used for the assessment of testicular volume which helps determine if surgical intervention is necessary. Color Doppler ultrasonography should also be performed to rule out torsion and other similar conditions, as well as to check for the presence of a small contralateral varicocele. Semen analysis may be performed to check for sperm pathology, which again helps in determining the indication of surgical intervention.
Differential Diagnoses of Testicle Pain in Young Boys
Infection
- Cellulitis
- Epididymitis (viral or bacterial)
- Orchitis
Torsion
- Epididymis
- Spermatic cord (testicular torsion)
- Testicular appendage
Trauma
Trauma to the testes often produces extreme pain. A direct blow to the scrotum, while very painful, usually causes only temporary pain. Most cases of testicular injuries (85%) are caused by blunt trauma. The injury may result in a bruise or swelling of the scrotal area and testes. Occasionally, trauma to the testes may cause a more significant injury that may require emergency surgery.
- Blunt (e.g. sports injury)
- Sexual abuse
Other
- Abnormality in the vas deferens or ejaculatory duct
- Hemangioma
- Hernia (obstructed or incarcerated)
- Hydrocele
- Idiopathic scrotal edema
- Non-infectious/chemical epididymitis
- Pyocele
- Testicular tumor
- Vasculitis (e.g. Henoch–Schönlein purpura)
Treatment of Testicle Pain in Young Boys
Torsion
If physical assessment findings are strongly suggestive of testicular torsion, immediate
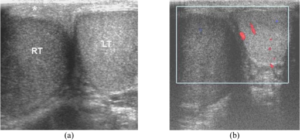
Image: “Acute testicular torsion in a 23-year-old man presented with sudden right scrotal pain for 1 hour. (a) Transverse US image shows enlarged, hypoechoic right testis (RT) with thickened scrotal skin. (b) CDUS shows no vascularity in the right testis.” by Thinyu S, Muttarak M. License: CC BY 2.5
surgery must be performed without waiting for imaging studies. Ideally, surgical repair of testicular torsion (surgical detorsion) must occur within 6 hours of the symptom onset, for delayed treatment can lead to a patient’s decreased fertility or even having to undergo an orchiectomy.
If the duration of the symptoms exceeds 10 hours, this guarantees the non-viability of the testis, and necessitates orchiectomy. Another indication of orchidectomy (i.e. testicular non-viability) includes a lack of bleeding from the testicle 10 minutes after the tunica vaginalis has been cut. In all cases, contralateral orchiopexy must be performed intra-operatively to avoid torsion of that testicle in the future. Hydatid torsion is treated with NSAIDs.
If immediate surgery is not possible, manual detorsion can be tried; however, this can be difficult and painful. If the manual detorsion is successful, a surgical fixation of the testes should be performed before the patient is discharged.
Epididymitis
The management of epididymitis involves bed rest and antibiotics against the implicated organism. Trimethoprim-sulfamethoxazole must be given to prepubertal boys for E. coli. In addition, supportive care is given, which includes analgesics (NSAIDs or narcotic analgesics), scrotal elevation and support, ice pack application, and, if indicated, spermatic cord block.
In children less than 10 years old, surgical exploration may sometimes be required as it may be difficult to differentiate it from testicular torsion. If a sexually transmitted disease is suspected as the etiology, it is essential to ensure that the sexual partner also gets tested.
Varicocele
Surgical repair of a varicocele (varicocelectomy) is performed in some adolescents with varicocele. The criteria for selecting patients for whom varicocelectomy may be indicated are as follows: an accompanying small testis, reduced fertility (poor sperm quality) or presence of an additional testicular condition that can affect fertility, bilateral varicocele, and symptomatic condition.
Varicocelectomy involves ligation or occlusion of the internal spermatic veins. Ligation is performed at different levels: inguinal, subinguinal, or suprainguinal, and can be performed using microsurgical approaches or using open or laparoscopic techniques.
Progression and Prognosis Testicle Pain in Young Boys
In testicular torsion, the main factor influencing the salvage rate of the testis is the duration from the symptom onset before a surgical procedure is performed. Within 6 hours, the salvage rates are as high as 90%; however, these rates drop dramatically to 50% at 12 hours and to almost 10% after 24 hours. Perinatal torsion has a very low salvage rate (<5%).
Even if testis loss has not occurred, a decrease in fertility is a common complication of testicular torsion. The reason for this is anti-sperm antibody production, which occurs due to the damaged blood–testis barrier initiated by ischemia–reperfusion injury.
Epididymitis or epididymo-orchitis, if untreated, can lead to complications such as testicular ischemia and infarction, testicular abscess and pyocele, and testicular atrophy.
Even after varicocele ligation, recurrence is possible, although the rate of recurrence varies with the surgical approach used. For instance, ligation performed using the open or laparoscopic approaches can have as much as 13–16 % recurrence rate, whereas the recurrence rate is only 5 % using microsurgical approaches. Embolization has a variable recurrence rate, ranging from 10 % to 25 %.
Prevention of testicular pain may be achieved by:
- Educating children about their genital anatomy and early recognition of pathologies.
- Practice of safe sex or abstinence to avoid contracting sexually-transmitted diseases and genital infections.
- Drinking sufficient amount of fluids throughout the day.
- Wearing a protective cup or athletic supporter while playing sports that can cause injuries.
- Undergo scheduled regular testicular self-exams so that it becomes easy to detect tumors or lumps at an early stage.
Review Questions
The correct answers can be found below the references.
1. Which of the following diagnostic methods are preferred to confirm the diagnosis of testicular torsion?
- Urinalysis
- Doppler ultrasonography
- Radionuclide imaging
- Surgical exploration of the scrotum
- Wait and watch
2. Which of the following are non-surgical indicators of testicular non-viability in a 10-year-old boy with testicular torsion?
- Duration of symptoms more than 10 hours
- No bleeding for 10 minutes after incision of tunica albuginea
- High degree of torsion
- Intact blood flow to the testicle on color Doppler ultrasonography
- Thickness of the spermatic cord
3. Which of the following is the most common organism causing acute epididymo-orchitis in a sexually active adolescent?
- Escherichia coli
- Ureaplasma urealyticum
- Neisseria gonorrhoeae
- Gardenerella vaginalis
- Chlamydia trachomatis

It was my last hope of having a child and Dr Obodo made my dreams come true. I asked for the spells, but didn’t tell my husband. We carried on trying to get pregnant as normal. I had a really good feeling about Obodo. I felt pregnant or like pregnancy was coming very about a week after the spells were cast. I began to vomit in the morning from morning sickness. I thought it was the toast. I’ve never felt like that before. And it was true! I went and grabbed the pee stick to show my husband. I went to my doctors at the earliest possible time to have a test and it came back positive. I immediately rang up my husband to let him know that the pee stick was not a false positive. He asked me how it was possible. He was certain that the pee stick was passed the expiry date. I told him all about Obodo, the fertility spells and he was amazed. We now have a very beautiful baby boy on the way and we are expecting to use Obodo in hope that I can have my baby girl. you can get in touch with doc via info ___ templeofanswer@hotmail . co . uk , call 234 8155 425481 for help
ResponderEliminarThank you,
The Messer Family