Chronic Venous Insufficiency — Symptoms and Treatment
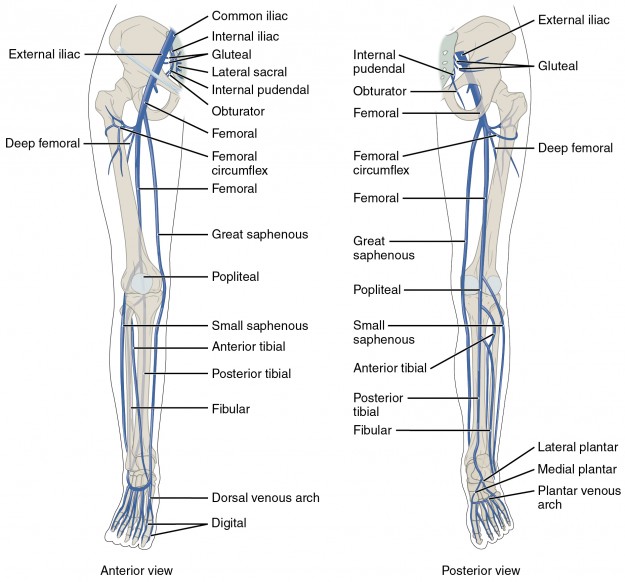
In a healthy individual blood passes through the deep and superficial veins of the legs into the thighs and then the iliac veins to the inferior vena cava. The blood is pushed by the heart and also by skeletal muscle pumps as the leg muscles contract and relax. Retrograde motion is prevented by organic valves in the veins. As the valves weaken blood begins to pool in the legs and feet resulting in discoloration, vein engorgement, varicose veins, and edema.
Table of Contents
- Definition of Chronic Venous Insufficiency
- Epidemiology of Chronic Venous Insufficiency
- Etiology of Chronic Venous Insufficiency
- Pathology and Pathophysiology of Chronic Venous Insufficiency
- Symptoms of Chronic Venous Insufficiency
- Diagnosis of Chronic Venous Insufficiency
- Differential Diagnoses of Chronic Venous Insufficiency
- Therapy of Chronic Venous Insufficiency
- Review Questions
- References
Are you more of a visual learner? Check out our online video lectures and start your vascular medicine course now for free!

Imageby TÜV SÜD. Licence: CC BY-ND 2.0
Definition of Chronic Venous Insufficiency
Venous insufficiency — blood flows backwards
Venous insufficiency is a condition in which blood flows backwards or retrograde through the veins due to failure to the venous valves. Gravity pulls the blood to the inferior extremities resulting in edema and vein engorgement.Both superficial and deep veins may be affected. This may be the result of thrombosis (clot formation, most commonly found in the veins of the leg and thigh), phlebitis (inflammation of a vein), congenital abnormality (lack of valve formation or valve deformity), or overuse (excess standing).

Image: “Mild chronic venous insufficiency” by James Heilman, MD. License: CC BY-SA 4.0
Epidemiology of Chronic Venous Insufficiency
Spread of venous insufficiency
Venous insufficiency is relatively common and is more common in the developed world. Approximately 40 % of the adult population suffers from some venous insufficiency and about 5 % of the population suffers from chronic venous insufficiency is found in about 2–5 % of the population. The condition is more common in women. Peak incidence in women is between 40–49 years and in men around 70–79 years.The elderly are at a greater risk of developing venous insufficiency. There is also increased risk with a history of deep vein thrombosis, sedentary lifestyle, smoking, obesity, or occupations involving prolonged standing with minimal ambulation.
Etiology of Chronic Venous Insufficiency
Venous insufficiency may result from a variety of conditions including congenitally, via wear and tear, or by the formation of thrombi. Most superficial venous insufficiency is the result of a valvular condition of the great saphenous vein which passes through the medial thigh and leg. The valves near the saphenofemoral junction are especially susceptible to reflux. Weak valves can fail spontaneously while normal valves weaken with excess standing, thrombosis, or trauma. Deep vein insufficiency is the result of deep vein thrombosis.Pathology and Pathophysiology of Chronic Venous Insufficiency
There are three sets of veins in the legs:- The superficial veins (great saphenous veins [media], small saphenous veins [lateral], etc.)
- The deep veins (from inferior to superior: anterior and posterior tibial veins, peroneal vein, poplitel vein, deep and superficial femoral veins, and finally the iliac vein the feeds into the inferior veina cava
- Communicating veins that connect the deep and superficial systems
Primary valve failure, where the valve is directly damaged, results from injury or thrombus formation. Secondary valve failure is the result of dilation of the vein walls. This prevents the valves from operating properly. Additionally, valves and vein walls are susceptible to damage during changes in hormone as seen in pregnancy.
Symptoms of venous insufficiency are the result of venous hypertension and the accumulation of metabolic byproducts such as carbon dioxide and lactate.
CEAP classification for venous disease
| Clinical Class | Characteristics |
| 0 | No clinical findings or symptoms |
| 1 | Teleangiectasia or reticular veins |
| 2 | Varicose Veins |
| 3 | Edema, only due to venous etiology |
| 4 | a) Pigmentation and/or eczema b) Lipodermatosclerosis |
| 5 | Prior ucleration, now healed |
| 6 | Active ucleration |
Symptoms of Chronic Venous Insufficiency
Signs of venous insufficiency
Common symptoms are focused in the legs and thighs and include:- Fatigue
- Burning
- Cramping
- Heaviness
- Formation of telangiectasia and varicose veins

Image: “Venous ulcer before surgery” by Nini00. License: CC BY-SA 3.0
- Edema
- Ulceration
- Dermatitis
- Cellulitis
Diagnosis of Chronic Venous Insufficiency
Ultrasound of the veins of the lower extremity is the preferred method to diagnose venous insufficiency. In these studies the physician is evaluating the vessels for reflux. If deep vein thrombosis is a concern then a D-dimer blood test may be useful in addition to ultrasound.Besides ultrasound, there are other methods to visualize the deep and superficial veins of the leg and thigh involves magnetic resonance venography.
Additionally, it is possible to measure the venous refill time. In patient with normal, healthy veins it takes about two minutes to refill the leg after blood is pumped out via the skeletal muscle pumps. In patients with valve patency it will take a shorter period of time due to venous reflux.
Differential Diagnoses of Chronic Venous Insufficiency
Clinical pictures similar to venous insufficiency
- Cellulitis
- Squamous Cell Carcinoma
- Stasis Dermatitis
- Traumatic Ulcers
Therapy of Chronic Venous Insufficiency
Treatment of venous insufficiency
Artificial compression is the treatment of choice for venous insufficiency or chronic venous insufficiency. Graduated compression stockings with a rating of 30–40 mm Hg are sufficient. Superficial varicose veins can be ameliorated surgically. Deeper veins can be bypassed to remove the points of excess reflux, but there are many complications associated with this type of surgery. There is no effective treatment involving medication. Deep vein insufficiency is difficult to treat.Additionally, in the presence of sever venous insufficiency or venous stasis ulcers an Unna boot may be applied to the legs. This is a special gauze that is impregnated with medication including zinc oxide and calamine that should help promote healing and reduce some symptoms.
Review Questions
The solutions are located below the references.1. Venous ulcers may be found on which part of the leg?
- Medial malleolus
- Lateral malleolus
- Peripheral leg
- Popliteal fossa
- Dorsal foot
- …is improved with activity.
- …is improved by elevating the legs.
- …results in pain with activity.
- …results in pain when elevating the legs.
- Both C and D.
- …surgical ablation.
- …exercise.
- …Aspirin.
- …compression stockings.
- …venous bypass.
Comentários
Enviar um comentário