Hemangiomas in Children — Treatment and Removal
Table of Contents
Hemangioma
Overview
Hemangiomas are considered as the most common tumors in infants and young children. Hemangiomas arise from the vascular tissues and are characterized by early proliferationfollowed by spontaneous involution. Hemangiomas in children can occur in the head and neck, the trunk, the upper or lower extremities or in internal organs.
Most hemangiomas are medically insignificant, being benign vascular tumors but they may occasionally impinge or certain organs such as the respiratory tract. They may also ulcerate and bleed to cause cardiovascular compromise or they may heal with cosmetic blemishes.
Epidemiology of Hemangiomas in Children
While hemangiomas can be diagnosed at birth, they usually become more evident after the first month of life. Thirty percent of hemangiomas are diagnosed at birth and 70% are later diagnosed within the first month of life.
The incidence of infantile hemangiomas in Caucasians is estimated to be around 10%. The incidence of infantile hemangiomas in preterm infants with a low birth weight can be as high as 30%.
The most commonly recognized risk factors for hemangiomas include the female gender of the child, an older maternal age, maternal placenta previa or preeclampsia, and infants who are the product of multiple gestations.
Hemangiomas are approximately 10 times more common in white infants compared to African American or Asian infants. Approximately, one-third of infantile hemangiomas are recognized at birth, while the remainder two-thirds appear within the first weeks of life.
The hemangiomas themselves are considered as benign vascular tumors and are known to spontaneously regress. Despite this, hemangiomas can cause obstructive and pressure symptoms when they appear in vital organs and places such as the upper respiratory tract. Additionally, very large hemangiomas can cause high-output cardiac failure due to the increased vascular flow within the tumor.
Patients with PHACE syndrome are at an increased risk of a higher mortality and morbidity. PHACE syndrome is characterized by posterior fossa malformations within the cerebellum, hemangiomas of the face and head, cerebral and carotid arterial lesions, cardiac malformations and eye abnormalities.
Pathophysiology of Hemangiomas
Infantile hemangiomas are benign vascular tumors that are composed of highly proliferating endothelial cells. During the early stages of the tumor formation, the endothelial cells are not lined correctly but, with time, they start forming blood vessels and the tumor becomes highly vascular. The tumor usually has a lobular structure.
It is hypothesized that during fetal development a significant number of immature endothelial and pericytes can be retained within different tissues. These immature cells can proliferate and differentiate postnatally and give rise to the tumors known as hemangiomas.
During the early proliferative phase of infantile hemangiomas, several proliferative inducing signals are produced and include a beta-fibroblast growth factor, vascular endothelial growth factor and proliferating cell nuclear antigen. Once a significant number of endothelial cells become abundant within the involved tissue, other cells, such as mast cells and myeloid cells, are attracted to the tumor.
The mast cells and myeloid cells produce tissue inhibitors of metalloproteinases, interferon and transforming growth factor which work collectively to terminate the endothelial cell proliferation phase and can induce involution of the tumor.
Clinical Presentation of Hemangiomas in Children
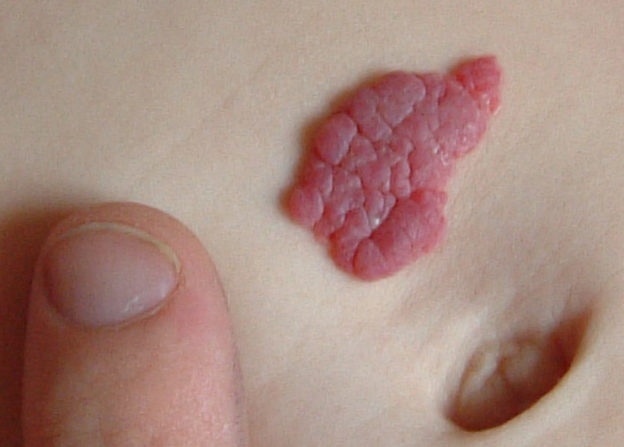
The first sign of a cutaneous hemangioma is skin blanching. Telangiectasias followed by red or crimson macules usually appear on the involved skin region. Ulceration of the involved skin might precede the appearance of the hemangioma.
- Small hemangioma on the scalp of a two year old female.
- Hemangioma on forehead of a six year old boy.
- Hemangioma
Hemangiomas usually grow at a much-exaggerated rate compared to the infant’s growth rate. They usually appear as skin lumps that are red or bluish in color. Cutaneous hemangiomas are most commonly found on the head and neck, followed by the trunk and least likely on the upper and lower extremities. Hemangiomas can also involve the liver, lungs or other deep organs. Hemangiomas within the liver can become large and can cause symptoms and signs suggestive of congestive heart failure due to increased cardiac output.
- Image: “A liver hemangioma.” by James Heilman, MD. License: CC BY-SA 3.0
- Image: “Hemangioma of the liver as seen on ultrasound.” by James Heilman, MD. License: CC BY-SA 3.0
If left untreated, 50% of infantile hemangiomas undergo complete involution by the age of 5 years, 70% by the age of 7 years and 90% undergo complete involution by the age of 9 years.
Hemangiomas can also involve the central nervous system. Children with central nervous system hemangiomas can present with seizures or focal neurological signs that are progressive and correlate with the tumor’s proliferative phase. The tumor’s proliferative phase usually lasts between one month after birth up to 12 months after birth.
Pressure and obstructive symptoms of hemangiomas include stridor or difficulty breathing. Blurred vision can occur with retinal hemangiomas.
Diagnostic Workup for Hemangiomas in Children
The same factors that regulate the tumor’s proliferation and differentiation can also be used to assess the tumor’s degree of proliferation and to determine the current phase of the tumor “early proliferative phase versus the involution phase”. The measurement of serum vascular endothelial growth factor and urinary beta fibroblast growth factor levels might correlate with the proliferation of the tumor. Matrix metalloproteinases which are secreted by the recruited myeloid cells are usually increased once the tumor becomes well differentiated and when the involution phase starts.
When cutaneous tumors are surgically removed, it is beneficial to differentiate between hemangiomas and other vascular tumors. Glucose transporter 1 (GLUT-1) stain is positive in proliferating and involuting hemangiomas, but negative in other vascular tumors.
Before surgical planning for the removal of the cutaneous or internal hemangioma, adequate imaging of the tumor is indicated for proper delineation of the tumor’s margins and extent. Magnetic resonance imaging (MRI) is the preferred imaging modality for the evaluation of infantile hemangiomas. MRI with intravenous gadolinium can help in the differentiation between proliferating and involuting hemangiomas. Proliferative hemangiomas might resemble high-flow vascular lesions, such as arteriovenous malformations, while involuting hemangiomas can resemble low-flow vascular lesions such as venous malformations.
Ultrasonography can also differentiate between hemangiomas and other liver tumors, such as liver cysts, but is not helpful in the delineation of the tumor’s extent. Arterial Doppler can be used to visualize the increased blood flow to the tumor.
Children presenting with breathing difficulties or stridor should undergo chest and neck x-ray imaging. This technique is fast and reliable in excluding upper airway obstruction.
Treatment of Hemangiomas in Children
Hemangiomas that are small and do not cause any other symptoms to the child should be left untreated because of the very high probability of spontaneous involution. When hemangiomas become symptomatic or problematic to the child or her or his caregivers, medical therapy might be warranted.
The first-line medical therapy for hemangiomas in children is the beta-blocker propranolol. Propranolol has been found to induce involution of infantile hemangiomas. Trial of corticosteroid therapy is considered in patients whom beta-blockers are contraindicated. Other agents with antiangiogenic properties include vincristine and interferon.
When medical treatment for symptomatic hemangiomas is initiated, close monitoring of the child is indicated. Infants should be evaluated for possible cardiovascular abnormalities, the frequency of dosing should be adjusted on an individual basis, and care must be taken to prevent hypoglycemia. The deleterious effects of hypoglycemia on the developing brain outweigh the benefits of treating the hemangioma in some children especially those with small and mildly problematic hemangiomas.
Laser surgery can be used to treat proliferating or involuting hemangiomas in children with excellent results. Pulsed-dye laser surgery is effective in children with ulcerating hemangiomas. Laser surgery should be repeated every two to four weeks until complete healing of the hemangioma happens.
Children with confirmed involuting hemangiomas might benefit from non-ablative fractional photothermolysis therapy. This technique helps with the common skin residue that can be seen after spontaneous involution of the tumors.
Surgical excision of hemangiomas should be limited to large, slowly involuting tumors. Early proliferative tumors carry a significant risk of hemorrhage if they are surgically excised. The main benefit of surgical excision of the tumors, as opposed to laser or medical therapy, is the availability of an excisional biopsy tissue with surgical approaches for the confirmation of the diagnosis.
Complications
Hemangiomas may ulcerate and bleed either superficially or deep within the structures. Massive bleeding may lead to high output failure while ulceration may expose wounds sites that become infected.
Enlargement of hemangiomas may cause obstruction such as in the respiratory tract which causes difficulty in breathing. Obstruction of the visual pathway may lead to development of amblyopia.
Hemangiomas are also associated with post-operative cosmetic blemishes especially for facial lesions involving the lips and nose.





Thank you for sending this info. I learned alot from it. I am grateful for the amount of time and effort you put into this helping us.
ResponderEliminarHow to Cure Different Types of Hemangiomas