Intestinal Malrotation — Symptoms and Surgery
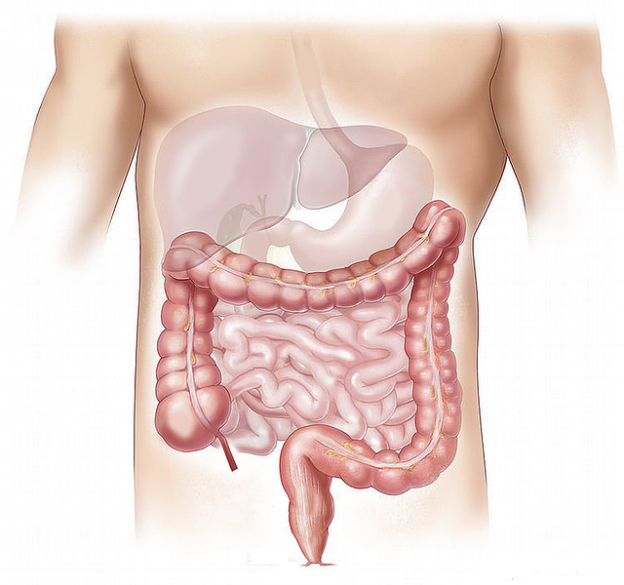
Image: “Innereien Kennzeichnung Medizinische Darm Leber” by Elionas2. License: Public Domain
Overview
Intestinal malrotation is a congenital anomaly that is characterized by an abnormal position of the bowel within the peritoneal cavity. This congenital anomaly might involve the small bowel, large bowel or both. The mesenteric bands which fixate the bowel can be absent in some cases.
Even if present, the mesenteric bands tend to be abnormal in position. Intestinal malrotation usually presents early in life. Mild intestinal malrotation might present after infancy; however, this is rarely seen. The most common manifestation of intestinal malrotation is bilious vomiting.
Epidemiology of Intestinal Malrotation
Intestinal malrotation is a common problem in the pediatric population, with an estimated incidence of 1 in 500 live births. Up to 75% of intestinal malrotation cases are diagnosed during the neonatal period. By the age of 1 year, 90% of the cases of malrotation have been diagnosed.
Intestinal malrotation is rarely an isolated finding. It has been associated with:
- Apple-peel intestinal atresia
- Cornelia de Lange syndrome
- Cantrell syndrome
- Cat-eye syndrome
- Chromosomal trisomies (13, 18 and 21)
- Marfan syndrome
- Meckel syndrome
- Prune-belly syndrome
The presence of intestinal malrotation is also associated with other anomalies including:
- Absence of kidney and ureter
- Congenital diaphragmatic hernia
- Meckel diverticulum
- Omphalocele
- Pyloric stenosis
- Imperforate anus
- Hirschsprung disease
Jejunal and duodenal atresia are also commonly found in patients with intestinal malrotation.
Mortality has dropped from 30% in the 1950s to 3% in the current era. This drop is attributed to better imaging techniques and the availability of better treatment options for infants with intestinal malrotation.
Pathogenesis of Intestinal Malrotation
The main pathologies in intestinal malrotation are:
- Impaired development of the intestine
- Incomplete intestinal rotation
- Abnormal fixation of the intestine to the abdominal wall
During normal embryogenic development, the developing gut rotates three times with the last rotation involving the traversing of the duodenum to the left side of the abdomen, the formation of the ligaments of Treitz, and the migration of the ileocaecal junction to the lower right abdominal quadrant.
In some cases, embryonic fibrous adhesions, known as Ladd’s bands, form before the fulfillment of the third embryonic rotation. The presence of these abnormal bands is believed to play a role in the pathogenesis of intestinal malrotation. The malrotated gut is more likely to undergo volvulus and torsion.
Torsion of an intestinal portion is associated with arterial blood supply compromise and eventually ischemia of that part of the intestine. Volvulus and torsion of a malrotated intestine is a common cause of severe sepsis and illness in infants and should always be considered as part of the differential diagnoses of the ill toxic infant.
Clinical Presentation of Intestinal Malrotation
The most common clinical presentation of malrotation in neonates is bilious vomiting. Abdominal distention is also a common finding. Volvulus due to malrotation is a life-threatening complication and can be the presenting feature of the congenital anomaly.
Failure to recognize midgut volvulus might result in delayed treatment which can be associated with small-bowel necrosis and short-gut syndrome. Newborns who develop short-gut syndrome are dependent on total parenteral nutrition.
Volvulus is caused because of the short mesenteric attachment of the midgut. The midgut is prone to twist counterclockwise which can obstruct the superior mesenteric artery and vein. If volvulus does not cause significant blood supply compromise to the gut, the presentation might be intermittent abdominal distention and pain. Children with volvulus and torsion of the blood vessels typically present with sepsis and are very ill due to acute bowel necrosis.
Malrotation of the intestines is a spectrum of anomalies which can be subtle or substantial. Unfortunately, it is still impossible to predict who is going to develop volvulus and who is unlikely to develop that complication; therefore, whenever you recognize an intestinal anomaly on abdominal imaging, you should document that anomaly and discuss it with the patient, even if it is not the reason that brought him or her to you.
Documenting the presence of even subtle intestinal abnormalities make it easier for you to think of midgut volvulus if the patient present to you in the future with non-specific symptoms, abdominal distension and pain.
Older children might present with intermittent abdominal pain that has been going on for years. Vomiting in older children with intestinal malrotation might be non-bilious which makes the diagnosis more challenging. Infants and children with intestinal malrotation might present with:
- Malnutrition
- Failure to thrive
- Diarrhea
Finally, a minority of the patients are diagnosed incidentally during adulthood.
Diagnostic Workup for Intestinal Malrotation
When the patient presents with symptoms and signs suggestive of bowel obstruction, a plain radiography is indicated. If volvulus is absent, the findings on plain radiography are usually non-specific and they might include right sided jejunal markings and absence of stool in the right colon.
Ultrasonography is useful in the evaluation of an infant or a child suspected to have malrotation. The relationship between the superior mesenteric artery and vein is inversed in patients with intestinal malrotation; therefore, ultrasonography typically shows the superior mesenteric artery on the right and the vein on the left.
Multidetector computed tomography scans of the abdomen are superior to the previous twoimaging modalities in the depiction of small and large bowel anatomy. On computed tomography, you should again look for an inverse in the relationship between the superior mesenteric artery and vein. The large bowel is typically found on the left side of the abdomen, whereas the small bowel is on the right.
Fluoroscopy with pediatric upper gastrointestinal contrast study is the imaging modality of choice for the examination of a child suspected to have intestinal malrotation.
The pediatrician or radiologist should focus on the duodenojejunal junction (DJ) location, which is abnormal in patients with intestinal malrotation. On the frontal view, the DJ junction fails to cross the midline and is not on the left of the left-sided vertebral body pedicle. The DJ junction is found to be inferior to the duodenal bulb.
Finally, the second and third parts of the duodenum are not found in the normal posterior retroperitoneal position. These three cardinal features on fluoroscopy are used to confirm the diagnosis of intestinal malrotation.
Management of Intestinal Malrotation
The management of intestinal malrotation is surgical. The main goal of surgical intervention in a child or an infant with intestinal malrotation is to prevent the life-threatening complication, midgut volvulus.
If a surgical intervention is carried out, the following principles should be followed. If volvulus is present, the intestine should be examined for viability. The first step is to untwist the volvulus and to mobilize the intestine.
As we have explained, patients with intestinal malrotation usually have abnormal peritoneal adhesions known as Ladd bands. These bands should be divided as they might increase the risk of intestinal obstruction in the future. The mesenteric base is then widened. To prevent future volvulus, the duodenum and caecum are fixated to the retroperitoneum.
Because of the abnormal anatomy of the intestine, it is recommended to remove the appendix at this stage. If the appendix is left in place, you should remember that the cecum and appendix will remain on the left side after the surgical intervention; therefore, an acute appendicitis will present with left-sided abdominal pain.
Even after optimal surgical intervention, the risk of post-operative adhesions, redo-surgery, and hernia remains high.
Comentários
Enviar um comentário