Types of Seizures and Epilepsy during Pregnancy
In Lecturio ;) - Seizures are the result of abnormal electrical activity in the brain, which can be either stimulatory or inhibitory. The abnormal activity consists of repeated consistent discharges that can lead to motor, sensory, autonomic or behavioral dysfunction.
Table of Contents
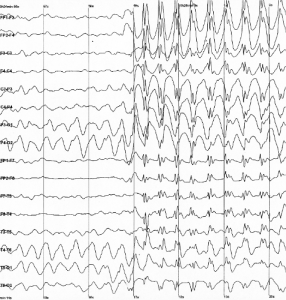
Image: “EEG registration.” by Baburov – Own work. License: CC BY-SA 4.0
Overview
A seizure is defined as uncontrolled high frequency bursts of action potential in the brain cortex. Thus, it has an initiation phase characterized by high frequency burst of action potential and a propagation phase characterized by hyper synchronization.
Classification:
Seizures can be classified according to the ILAE 2017 guidelines into:
- Focal seizures which can be simple or complex.
- Generalized seizures which can be convulsive or non-convulsive.
- Unclassified seizures.
Partial (focal) seizures occur as a result of abnormal electrical activity in one hemisphere of the brain, thus affecting one side of the body or even only an extremity. Partial seizures can be simple, not involving loss of consciousness, or complex, which affect the conscious level
Generalized seizures involve both brain hemispheres and can affect the whole body, associated with loss of consciousness. It is important to differentiate between seizures and epilepsy, which is recurrent seizures due to known or unknown factors. Two or more seizure episodes without return to baseline activity and mental status, or continuous five minutes of seizures, is known as status epilepticus.
The repetitive abnormal muscular contractions associated with seizure activity or status epilepticus are harmful to the physiological body environment in many ways. During muscular contraction, hyperthermia and hyperglycemia, followed by depletion of glucose stores, will develop.
Rhabdomyolysis and lactic acidosis with renal failure also are common complications of status epilepticus. Apnea with hypoxia can also be a complication, which will result in hypertension to maintain cerebral oxygenation. Multi-organ failure can be the end result due to hypercarpia and hypoxemia.
Etiology of Seizures
Thorough evaluation of seizure patients is mandatory to identify the etiologic factor. The incidence of the first seizure attack is common before 2 and after 65 years of age, with male predominance.
Types of Seizures
Partial/focal/local seizures
The electrical discharge involves a small focus or a single hemisphere of the brain, and the seizure involves one side of the body or a single extremity. Usually, there is an aura preceding partial seizures.
Partial seizures can be simple with no loss of mental status or complex with loss of consciousness. Simple partial seizures can be motor, sensory and autonomic. Patients may report automatisms, which are repetitive involuntary movements, e.g., lip smacking and chewing.
There two types of partial seizure :
- Simple partial seizure: the patient remains conscious during the seizure episode. The episodes are usually very brief, lasting for less than two minutes.
- Complex partial seizures: this type of seizure results to unconsciousness leading to uncontrolled motor symptoms that patient cannot recall such as chewing, moving legs, lip smacking as well as thrusting of the pelvis
Generalized seizures
The electrical activity involves the whole brain and affects both body sides or multiple extremities. Generalized seizures can be classified into:
Generalized tonic-clonic (or grand mal) seizures where patients lose consciousness, followed by generalized body stiffness called the tonic phase. After that, the patient experiences generalized convulsions or jerking, which is referred to as the clonic phase. Each of the phases lasts from 30 to 60 seconds, then the patient goes into deep sleep known as the postictal phase. The patients lose control over the bladder leading to incontinence. Various injuries are common during the grand mal seizures; therefore, it is important to secure the airway and prevent tongue biting during the attack.
Myoclonic seizures do not include loss of consciousness, but the patient experiences brief jerky movements of a group of muscles, described as shock-like jerks.
Clonic seizures are repetitive jerking movements that cannot be stopped by physical restraining. The contractions are rhythmic and involve both body sides.
In tonic seizures, the muscle tone suddenly increases, leading to stiffening of the body. It usually involves both sides without loss of consciousness.
Image: “An electroencephalogram of a person with childhood absence epilepsy showing a seizure,” by Der Lange. License: CC BY-SA 2.0
Atonic seizures involve loss of muscle tone, which leads to falls. These are also called drop attacks or akinetic seizures.
Absence seizures were formerly called petit mal seizures and consist of momentary loss of consciousness without motor jerking. They are most common in children and are known to affect school activities. The patients are not aware of the seizure disorder, but others report that they stare blankly several times a day.
Febrile seizures are most common during childhood between 6 months and 5 years of age. The seizures occur during febrile illness due to viral or bacterial infection or after vaccination-induced fever. Positive family history is common among affected children. These seizures can be simple with tonic-clonic convulsions or twitches that last for less than 15 minutes and no paralysis or paresis after the episode. They can also be complex, lasting for more than 15 minutes, with residual weakness of the affected extremities.
Tonic-clonic seizures, previously known as grand mal seizures, are the most dramatic type of epileptic seizure and can cause an abrupt loss of consciousness, body stiffening and shaking, and sometimes loss of bladder control or biting your tongue.
Evaluation of febrile seizures in children
Exclusion of other causes of childhood febrile seizures, including meningitis, is crucial for management. Febrile seizures are common in the first 24 hours of fever and usually affect children with frequent fever episodes or with positive family history of febrile seizures.
Management of febrile seizures
ABCs with securing the airway, breathing and circulation are the first step. The convulsing patient should be placed on the lateral decubitus with administration of intravenous diazepamfor rapid control of the seizures. Parents can use diazepam gel into the rectum before arriving to the emergency department in case of prolonged seizures.
Acetaminophen is used to treat fever episodes. Patients with febrile seizures can have recurrent attacks of febrile seizures which commonly disappear with advanced age. There is no residual brain impairment or epilepsy risk.
Evaluation of the First Seizure
After stabilization, the first step in evaluating a patient with a first seizure episode is to identify any reason that may hide behind the attack as well as the possibility of recurrence of the episode. Recurrent unprovoked seizures are considered epilepsy, while provoked seizures due to acute brain lesion or systemic metabolic abnormality are not considered epilepsy.
Brain-related causes of epilepsy in adults include brain trauma, brain tumor, stroke, infection or malformation. Brain anoxia due to drowning, cardiac arrest can also present with seizures.
Systemic causes include:
- Toxic and drug abuse, e.g., alcohol withdrawal is a common cause of seizures that occur in the first day after the last drink.
- Hyperthyroidism is a common cause of convulsions and can exacerbate an existing seizure disorder.
- Hyponatremia with brain edema may lead to tonic-clonic fits.
- Hyperglycemic seizures occur in diabetic patients and manifest as focal fits.
- Hypoglycemic seizures may occur due to insulin injection, insulinoma or hypoglycemicdrugs. The patient will present with diaphoresis, tachycardia and confusion due to autonomic stimulation.
- Hypocalcemia and hypomagnesemia may manifest as tetany and convulsions especially after parathyroid resection.
- Renal failure can lead to convulsions in uremic patients along with loss of consciousness and metabolic disorders, even with hemodialysis.
Thorough history is mandatory for identification of any etiologic factor, including family history, past medical history, medication history and social history. Positive family history of epilepsy is a risk factor for the condition. Past medical history of febrile seizures, metastatic malignancy, systemic lupus erythematosus, sickle cell disease, CNS infection or previous surgery should be evaluated.
Social and sexual history should be discussed to look for drug abuse and neurosyphilis or HIV. Full neurological examination should be condicted to search for any lateralizing signs, focal signs or signs of meningitis.
Causes of non-febrile seizures in children can be genetic, CNS infections, brain structural abnormality and metabolic disorders.
Laboratory workup
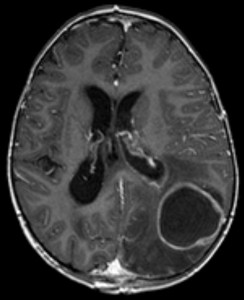
Image: “Hirnabszess in der MRT / MRT scan of brain with abscess,” by Hellerhoff. License: CC BY-SA 3.0
- Basal metabolic profile, including sodium, potassium, calcium, magnesium, blood urea nitrogen and creatinine and glucose
- Thyroid hormone levels
- Drug toxicology screen
- CBC
- Renal function tests
- Liver function tests
Imaging studies
- EEG (electroenchephalography) can be used for screening, but it is not specific in excluding seizure disorder. It can detect specific types of seizures and predict recurrence.
- CT & MRI can detect brain tumors, infarctions, abscess and vascular malformations.
- ECG can evaluate arrhythmia as an etiology for brain anoxia or syncopal episodes.
- Lumbar puncture and CSF analysis are used to evaluate for brain infections, CNS lymphoma and subarachnoid hemorrhage.
Management of the first seizure episode
Prolonged attack of more than 2 minutes requires immediate abortion with antiepileptic medications to avoid serious consequences. Intravenous administration of benzodiazepines is effective in aborting the attack. Prophylaxis with antiepileptic drugs may be needed with recurrent episodes while correction of the underlying pathology is ongoing.
Epilepsy and Pregnancy
Epilepsy during pregnancy can cause various critical conditions that may compromise both the mother and the fetus, including miscarriage, fetal malformations, preterm labor, stillbirth and promotion of seizure threshold.
The risk of developing congenital malformation in the fetus is double that of the population but remains as low as 6%. The risk increases with administration of more than one medications and at high doses. Congenital malformations include cleft lip and palate, neural tube defects, lower IQ, cardiac and genital defects.
Risk of epilepsy increases during pregnancy in women with previous history of eclampsia, stress, lack of sleep, inadequate medication levels, hormonal changes and salt and water retention.
Management of epilepsy in pregnant women
- Genetic counseling as early as possible.
- Check the level of antiepileptic drugs monthly; attempt to lower the dose or withdraw the medication if necessary after 2 years of seizure free period.
- Folic acid supplementation is mandatory to prevent neural tube defects and congenital anomalies.
- Vitamin K should be given to pregnant women and newborn babies to prevent bleeding from antiepileptic drugs.
- During pregnancy, maternal and amniotic fluid alpha fetoprotein level can be used to assess fetal anomalies.
- At the time of labor, consider prophylaxis with intravenous diazepam or phenytoin. If there are signs of fetal distress, immediate delivery is indicated.
- Antiepileptic drugs are not a contraindication to normal vaginal delivery or breastfeeding.
- No switch or discontinuation of the antiepileptic medication during pregnancy is indicated as long as optimum symptoms’ control is achieved.
Antiepileptic Medications
Image: “Valproic acid structure,” by Giorgiogp2 – Own work. License: CC BY-SA 3.0
Their goal is to achieve long term seizure free survival with least complications.
Absence seizures are best treated by ethosuximide. Valproic acid has similar efficacy but more side effects. Valproic acid and lamotrigine are indicated if absence seizures are associated with tonic-clonic or myoclonic seizures. Ethosuximide is a t-type calcium channel blocker with a long half-life of about 40 hours. Common side effect is GI disturbance.
Generalized tonic-clonic, tonic and myoclonic seizures are best treated with valproic acid, lamotrigine and levetiracetam. Valproic acid acts by blocking sodium and calcium channels. It is considered a broad spectrum antiepileptic medication, which can be used for all kinds of seizure disorders. Side effects include pancreatitis, weight gain, fetal defects, hair loss, GI upset, osteoporosis and abnormal blood count.
Lamotrigine is a similar broad spectrum anticonvulsant that acts by inhibiting glutamate release in the brain. Side effects include rash, fatigue and cognitive impairment. Levetiracetam is also a broad spectrum drug with better side effect profile. It has no cognitive impairment effects but can induce fatigue, mood changes and insomnia.
Other antiepileptic medications
- Phenobarbital is a barbiturate type drug that works via increasing GAPA inhibition. Side effects include addiction, memory impairment, congenital anomalies and mood changes.
- Phenytoin is the most widely used medication. It acts by inhibiting sodium channels. Side effects include Stevens-Johnson syndrome, hair growth, rash, cognitive impairment and osteoporosis.
- Carbamazepine acts via sodium channels against partial seizures. Side effects include agranulocytosis, Stevens-Johnson syndrome, weight gain and blurring of vision.
- Gabapentin works through GAPA transport in the brain. Side effects include fatigue and weight gain.
World Health Organization:
https://www.who.int/mental_health/neurology/epilepsy/international_day/en/
Global campaign against Epilepsy with the WHO:
https://www.who.int/mental_health/neurology/epilepsy/euro_report.pdf?ua=1
International Epilepsy Organizations by Country:
https://www.epilepsy.org.uk/about/international-epilepsy-organisations
International League Against Epilepsy:
https://www.ilae.org/
International Epilepsy Organizations by Country:
https://www.epilepsy.org.uk/about/international-epilepsy-organisations
International League Against Epilepsy:
https://www.ilae.org/
Associação Portuguesa de Familiares, Amigos e Pessoas com Epilepsia:
http://www.epilepsia.pt/
Liga Portuguesa contra a Epilepsia:
http://www.epilepsia.pt/lpce
Sociedade Portuguesa de Neuropediatria:
https://neuropediatria.pt/index.php/pt/para-os-pais/o-que-e-a-epilepsia
American Epilepsy Society:
https://www.aesnet.org/for_patients/about_epilepsy
Epilepsy Foundation in Chicago:
https://epilepsychicago.org/
Epilepsy Society, guidelines in the web site:https://www.epilepsysociety.org.uk/what-epilepsy?gclid=Cj0KCQjwj9LkBRDnARIsAGQ-hUcOQh1prQ3Yut-rUuf5TcAa9-Iy3XXKthuuuJpY-EiPG9HAHkE3q3IaAvIFEALw_wcB#.XJSoXyL7Tcs
NHS in the Uk point of view and guidelines:https://www.nhs.uk/conditions/epilepsy/
https://www.who.int/mental_health/neurology/epilepsy/international_day/en/
NHS in the Uk point of view and guidelines:https://www.nhs.uk/conditions/epilepsy/
https://www.who.int/mental_health/neurology/epilepsy/international_day/en/

Comentários
Enviar um comentário