Pediatric Trauma: Primary and Secondary Survey — Checklist
Table of Contents
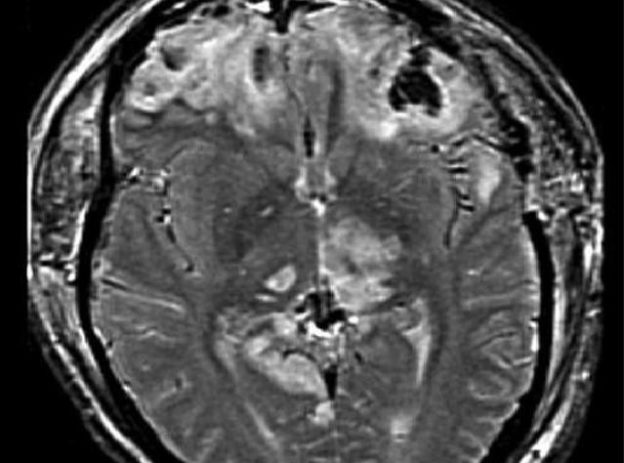
Image: “MRI of patient with brain trauma and resultant brain herniation.” By Rehman T, Ali R, Tawil I, Yonas H (2008). “Rapid progression of traumatic bifrontal contusions to transtentorial herniation: A case report”. License: CC BY 2.0
Overview
The most common cause of trauma differs per the child’s age. The most common cause of injury in infants is non-accidental. Falls are common in toddlers and account for the majority of traumatic injuries in this age group. Older children are more likely to be involved in motor vehicle accidents or sports injuries.
Most of the deaths related to trauma happen at the scene and can be attributed to severe head injuries and major hemorrhage. The next few hours are also very critical as 30% of the trauma-related deaths happen within the first few hours.
Head injury, ongoing hemorrhage and airway obstruction are the leading causes of death within the first few hours after presentation to the emergency department. The remainder of trauma-related deaths happen in the following days after admission to the hospital and can be attributed to sepsis and improper resuscitation.
Because half of the deaths that occur after trauma are caused by ongoing hemorrhage, failure to secure the airway and inadequate resuscitation, pediatricians had to define a systematic approach to the trauma patient. This systematic approach mainly consists of a primary surveyand a secondary survey. Going back to the primary survey can happen at any time during the management of the traumatic child.
The Initial Management of Pediatric Trauma
When a child presents to the emergency department due to sustaining a significant blunt or penetrating trauma, a systematic approach should be followed in order for us to not miss any life-threatening injuries.
The first step is to perform a primary survey to assess the airway patency, breathing, circulation, disability level, and any emergency investigations. Once the airway is secured, the hemodynamic stability of the child should be assessed and proper initial resuscitation should be attempted.
After the child is considered as hemodynamically stable, a more complete secondary surveyshould be carried out to detect any less significant injuries.
After finishing the secondary survey, emergency treatment should be started. For instance, in the case of head trauma, the child might need urgent intubation. Once the child is stable, definitive care should be provided. In case of head trauma, the definitive treatment can be surgical intervention to relieve an epidural hematoma for instance.
Primary Survey in Pediatric Trauma
The goal of the primary survey in pediatric trauma is to detect any life-threatening injuries and correct them as soon as possible.
Airway management in the traumatic child
The first step in the primary survey is to check and secure the patency of the airway. Because of the normal anatomical features of the head in the pediatric population, i.e. larger heads with smaller mid-face, the risk of airway obstruction is significantly higher in children compared to adults.
Image: “Jaw thrust maneuver.” by Randhillon – Own work. License: CC BY-SA 4.0
When a child sustains a blunt trauma without major involvement of the head, it might be justifiable to perform a simple jaw thrust maneuver to secure the airway if needed because the risk of cervical trauma is low.
Children with a traumatic brain injury very likely have a concomitant cervical injury and securing the airway in this group of children is challenging. Because of the increased risk of basal skull fractures in children with significant head trauma, orotracheal intubation is the preferred method of intubation when indicated.
Children with a significant head trauma who are not confirmed to have a cervical spine injury and who need urgent intubation should undergo manual in-line immobilization of the neck, rapid sequence induction, and orotracheal intubation.
Rapid sequence induction is indicated in the management of the airway in the primary survey of children with significant head trauma because it has been found to improve the outcome of head injury patients and to lower the intracranial pressure.
Thiopental, etomidate, or ketamine plus fentanyl can be used as an induction agent in children. Succinylcholine can also be used to facilitate intubation in children with significant head injuries as long as they do not show any signs of a significant crush injury.
The main indications of intubation in children are respiratory inadequacy, a Glasgow coma scale below 8, suspected increased intracranial pressure, need for ventilation or need for transport to a tertiary center.
Breathing in the traumatic child
The traumatic child can develop hypoxia and airway collapse very easily; therefore, adequate ventilation should be secured in any child with a significant trauma. The main emergencies to be excluded in the primary survey of the adequacy of breathing are tension pneumothorax, open pneumothorax, hemothorax and a flail chest.
Chest trauma can cause significant pain which can further complicate breathing for the child. Children with multiple rib fractures or a flail chest should receive good and strong analgesia to allow for full expansion of the chest and decrease the risk of airway collapse.
Circulation assessment and management in the traumatic child
Children with traumatic injuries can have hypovolemia due to hemorrhage. The heart rate and the capillary refill time are the first to become abnormal in a traumatic child. Children with significant hypovolemia might have tachycardia or a capillary refill time above 2 seconds.
Peripheral arterial pressure is usually maintained until the child becomes severely hypovolemic and loses 25 to 40% of blood volume; therefore, a traumatic child with hypotension is indicative of decompensated shock. Impaired mental state can be a sign of inadequate circulation rather than a direct brain injury.
Intravenous access should be secure as early as possible in any child with significant traumatic injuries. In young and small children, it is usually easier to secure an intravenous access in the hands or feet rather than the antecubital fossa. When intravenous access is not possible within 90 seconds, the child is deemed to have severe injuries, and is younger than 6 years, intraosseous access should be attempted.
Initial resuscitation in a traumatic child with hypovolemic hemorrhagic shock
When a child is diagnosed with hypovolemic hemorrhagic shock, 20 ml/kg of Ringer’s lactate or isotonic saline should be administered in a bolus dose over five minutes. Because of the hazardous consequences of hypothermia in children, warm isotonic crystalloid solution is preferred. If the child still shows signs of decompensated shock after the administration of two boluses, then blood boluses of 10 ml/kg should be started.
Children with ongoing hemorrhage should receive fresh frozen plasma and platelets during the primary survey until they are stable enough to undergo definitive treatment of the origin of the hemorrhage.
Disability assessment in the traumatic child
In the primary survey, we aim to assess the level of neurologic injury that might be life-threatening and not to assess the exact level of neurological deficits the child is expected to have after definitive treatment. The AVPU system is rapid and adequate in identifying significant neurological injury in the traumatic child.
The child should be evaluated and he or she might be A: Alert, V: Responsive to voice commands, P: Responsive to pain, or U: Unresponsive. After securing the airway, breathing and circulation, morphine can be used at this stage to provide adequate analgesia.
Investigations as part of the primary survey in the traumatic child
At this stage, a chest X-ray, a pelvic X-ray and a cervical spine X-ray might be indicated to exclude significant chest injuries, such as pneumothorax or hemothorax, pelvic fractures and severe cervical spine injuries.
Arterial blood gases, full blood count, cross and matching of blood and serum glucose levelsshould be determined in any child with hypovolemic shock. A urinary catheter might be required to evaluate urinary output.
Once the primary survey is finished and before starting the secondary survey of the child, it is usually recommended to take a step back now and re-assess the situation.
One should attempt to get a detailed medical history to look for any allergies, a history of recent medication use, past medical history, and the mechanism of injury. Whenever possible, try to determine when was the last oral intakebecause this information might be needed if surgical intervention is needed and general anesthesia is required.
Secondary Survey in Pediatric Trauma
The goal of the secondary survey in the pediatric traumatic patient is to perform a head to toe examination to detect any less obvious injuries. The cervical spine should be protected during this stage and hypothermia should be prevented.
Hypothermia can be prevented by using warming blankets and overhead radiant heaters. During the secondary survey, the airway, breathing and circulation from the primary survey should be re-assessed regularly.
Head and neck examination as part of the secondary survey
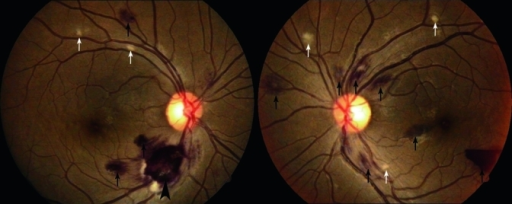
Look for facial or scalp bruising, lacerations, depressed skull fractures and otorrhea or rhinorrhea – two signs of basal skull fractures. The Glasgow coma scale should be determined during this examination and pupillary reflexes should be checked. An optic fundoscopic examination should be performed looking for retinal hemorrhages, a sign of non-accidental injury in infants.
Based on the Glasgow coma scale (GCS), the severity of the traumatic brain injury (TBI) can be determined. Mild TBI has a GCS between 13 and 15, moderate TBI has a GCS between 9 and 12 and severe TBI has a GCS between 3 and 8. Any child with a GCS < 8 should be intubated.
Children with a GCS < 12, loss of consciousness at time of injury, obvious signs of skull fracture, or focal neurological signs or symptoms such as seizures, should undergo a brain computed tomography scan. Whenever a brain computed tomography scan is performed in a traumatic child, the C-spine should be included.
Computed tomography scans of the chest or abdomen should be performed only if indicated, i.e. lacerations and bruising of the chest in a motor vehicle accident victim. Children with focal neurological signs, an abnormal computed tomography scan, or penetrating or depressed skull fractures should be referred to a neurosurgical unit at this stage.
Children with severe vomiting, a deteriorating GCS, and non-reactive pupils might have impending cerebral herniation and should receive Mannitol or hypertonic saline until definitive neurosurgical intervention is performed.
Children with severe TBI should undergo intracranial pressure monitoring, and surgical or medical intervention should be started if the intracranial pressure goes above 20 mmHg. Cerebral perfusion pressure which is equal to arterial blood pressure minus intracranial pressure should be maintained between 40 and 60 mmHg. This can be achieved by preventing systemic hypotension and reducing the intracranial pressure.
Spinal injuries as part of the secondary survey
Children with significant traumatic brain injuries might have a cervical spinal injury. The most common site of cervical spinal injury in traumatic children is within the C1 to C3 spinal segments.
Cervical X-rays can be normal and a computed tomography scan should be performed in any child who sustains a significant trauma to the head or who has focal neurological deficits. If the child still has signs and symptoms of focal neurological deficits and the computed tomography scan is normal within the first 72 hours post-trauma, then a magnetic resonance imaging scanof the cervical spine is indicated.
Chest examination as part of the secondary survey
Up to 3% of children who sustain a significant traumatic injury have some sort of a significant chest injury as well. The most common types of chest injuries are pneumothorax, hemothoraxand lung contusions. Children with improper oxygenation of the blood despite adequate breathing, and circulation and a patent airway, might have a lung contusion. A chest computed tomography scan can reliably exclude lung contusions.
Abdominal examination as part of the secondary survey
Up to 10% of children who sustain a significant trauma also have a significant abdominal trauma that can be life-threatening. In fact, abdominal trauma is the second most common cause of death in the traumatic child after airway obstruction.
A complete physical examination of the abdomen in the secondary survey looking for bruising, abrasions, guarding, tenderness and abdominal distension is sufficient in identifying up to 97% of significant abdominal injuries in children.
Image: “Microscopic hematuria: Red blood cells in a urine sample seen under the microscope.” by Bobjgalindo. License: CC BY-SA 4.0
During the primary survey, we recommended the insertion of a urinary catheter. If the child has hematuria, the possibility of kidney or ureter injury is high. Children with significant abdominal injuries should undergo a FAST scan to exclude any intra-abdominal fluid accumulation, a sign suggestive of intra-abdominal bleeding.
Whenever in doubt, an abdominal computed tomography scan should be performed to exclude intra-abdominal organ injury. A double contrast-enhanced computed tomography scan is superior to non-contrast computed tomography in the detection of abdominal injuries.
Children who are hemodynamically unstable despite adequate resuscitation and who have a distended abdomen should undergo urgent laparotomy. Additionally, children with proven peritonitis which is most commonly due to a small bowel, large bowel, stomach or gallbladder injury, should undergo urgent laparotomy. Children with a suspected renal injury should also undergo urgent surgical intervention.
Upper and lower limbs examination as part of the secondary survey
Skeletal injuries are very common in pediatric trauma patients. Fortunately, skeletal injuries are easy to manage and are rarely fatal. Open fractures usually result in more blood loss in children compared to closed fractures. For example, an open fracture of the femoral shaft can result in the loss of as much as 40% of the blood volume, precipitating shock.
The Next Step
Once the primary and secondary surveys are finished, the child is considered as stable and the exact types of injuries are determined, definitive care should be provided. Definitive care is different based on the type of injury, the associated injuries, and the child’s age.
For instance, children with large epidural hematomas usually undergo epidural hematoma evacuation. On the other hand, children with skeletal injuries undergo adequate orthopedic management of their fractures which can be surgical or non-surgical.
Most of the deaths occur due to the failure to recognize an impending airway obstruction, inadequate breathing and a failing circulation. Failure to detect less obvious abdominal, skeletal, or spinal injuries accounts for the remainder of the deaths and can be prevented by a thorough and complete secondary survey.


Comentários
Enviar um comentário