Introdução à Neonatologia ;) Neonatology (Newborn Medicine): Introduction
In Lecturio :) - This article introduces the reader to the topic of neonatology. In the first moments of life, individuals are particularly fragile and it is imperative that medical students have a comfortable grasp on how to assess whether an infant is healthy and what exactly to do if the infant is not healthy. This knowledge will be built around principles you learned in USMLE Step 1, and the basic sciences govern much of what we practice in Neonatology today. In this article, we introduce the epidemiology of births in the United States, remind the user of fetal physiology and prepare you for learning resuscitation techniques etc later on in this neonatology course.
Table of Contents
Image: “A 30 minutes old infant in Iran. The nurse is doing some care after birth.” by Alborzagros Alborzagros . License: CC BY-SA 3.0
Definition
Neonatology is defined as a subspecialty of pediatrics that comprises care of the newborn infant child especially the ill and premature.
Epidemiology
Epidemiology of Newborn Infants in the United States
There are around 4 million births each year in the United States. Of these, around 10 % (or 40,000) require some kind of intervention at birth. Of this 10 %, 10 % (or 1 % of the total population) require resuscitation at birth. As such, it is imperative for medical students to be comfortable with all manner of newborn interventions, not limited to resuscitation.
Risk Factors for Needing Resuscitation at Birth
There are a number of risk factors you should be aware of, that increased the probability of an individual needed resuscitation at birth. These are split below into pregnancy and labor risk factors. Women with a high-risk pregnancy will be flagged prior to labor (often), but women whose pregnancy is complicated in labor need a watchful eye to identify the birth as high risk for the child needing resuscitation.
Pregnancy risk factors:
- Multiple gestations (twins, triplets, etc.)
- Maternal infection (blood should be collected from the mother and white cell counts etc. should have an eye kept on them)
- Magnesium for preterm labor (these children are likely to come out “floppy” and many need resuscitation)
- Maternal substance abuse (this should be flagged in pre-labor questioning) or use of depressive anesthetics and analgesics such as opioids.
Labor associated risk factors:
- Breech presentation: This is generally described as a child that is born with its bottom first, before the head. The standard and most common birthing position is described as cephalic and occurs when the child is born head first. A breech presentation has an increased risk of complications (hypoxia to the infant etc.) and, as such, is a risk factor for infant resuscitation.
- Failure to progress: This is generally described as labor that has continued for more than 20 hours with little dilation (or dilation between 1 and 2 cm an hour). Many women will never reach full dilation and an emergency C-section will be planned. However, if a vaginal delivery is achieved, the newborn is at significantly increased chance of being in distress and requiring resuscitation.
- Nuchal cord: This describes a process by which the umbilical cord becomes wrapped around the neonate’s neck. They are reasonably common and most will spontaneously resolve before the delivery. However, this can have significant mortality and morbidity and is a significant risk factor for infant resuscitation on birth.
- Image: “Meconium close-up”. By Jeremy Kemp. License: Copyrighted free useMeconium stained liquor: meconium is the infant’s first stool. It is often described as “green and tenacious”. Staining of liquor with meconium indicates that an infant has passed meconium in the womb and is typically in distress and, as such, the probability they will require resuscitation on birth is significantly increased. Meconium is usually picked up during vaginal examination every 4 hours. In a healthy neonate, it is passed after labor.
- Chorioamnionitis: This is an inflammation of the fetal membranes (the amnion and the chorion) which can be due to an infection. This infection is usually bacterial in nature. In women with a prolonged labor, the risk increases significantly and is one reason long labors are not advised.
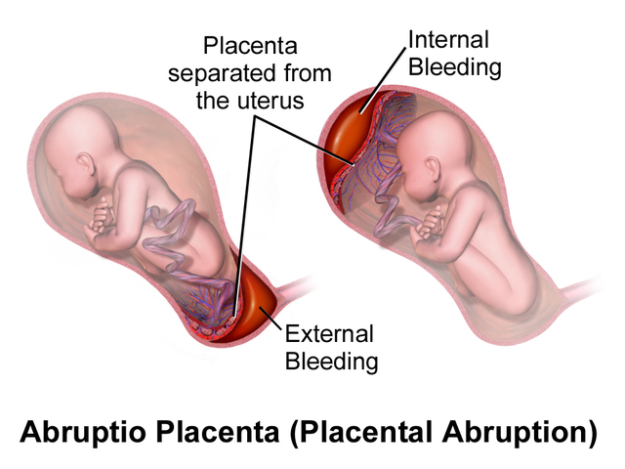
- Placental abruption/previa: placenta previa is abnormal position of the implantation site of the placenta which typically represents a placenta inserted lower down in the uterus, and possibly partially or fully covering the cervix. In some placenta previa, a vaginal delivery is, in fact, possible but the risk of newborn resuscitation is increased. In many, an emergency C-section may have to be performed. Rupture of the placenta denies the infant the only source of nourishment and thus the newborn is likely to be in distress hence necessitating resuscitation.
Physiology/Pathophysiology
Development of the chambers of the heart during pregnancy
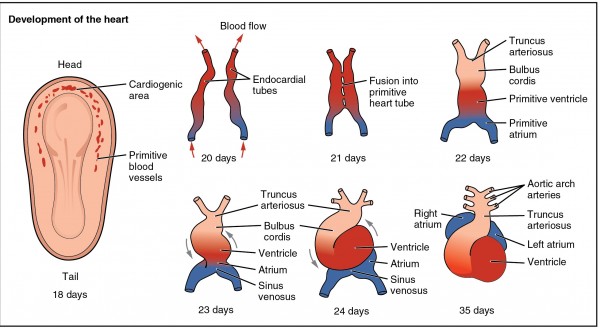
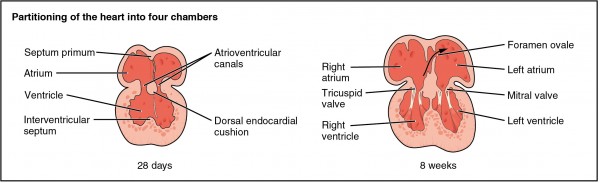
This acts as a reminder from embryology you are probably familiar with from USMLE step 1. However, it will form a crucial part of the clinical practice of neonatology and needs to be refreshed.
The septation of the chambers of the heart proceeds as follow. To begin with, the septum primum grows up towards the endocardial cushions which narrow the previously formed foramen primum, then the second foramen (foramen secundum) forms in the septum primum. The septum secundum develops. Whilst this occurs, there is a right to left shunt in the which is maintained by the foramen secundum. The septum secundum grows to cover most of the foramen secundum; the hole left behind is the foramen ovale. When an individual does not close the septum primum and septum secundum after birth, this is known as a patent foramen ovale.
It is also important to remember that the septum secundum and septum primum eventually fuse with each other making the atrial septum. As evidenced below, the foramen ovale will close after birth because of the pressure in the left atrium (which stops the right left shunting).
The ventricles form in a far simpler series of events. It can be broken down into 3 simple steps:
In the first step, the muscular ventricular septum forms. The opening of this is called the interventricular foramen. The aorticopulmonary septum then fuses (via rotation) with the ventricular septum; this closes the interventricular foramen. A ventricular septal defect can form. This usually arises from the membranous septum. Again, these defects are important to remember for the coming lectures and a solid understanding of the embryology will leave you in good stead to understand the congenital defects and their relevant symptomatology often seen in the neonate.
In the fetus, blood from the right ventricle mainly flows through the ductus arteriosus, bypassing the lungs. This is because the lungs are full of fluid and the fetus does not receive oxygenated blood via gas exchange. Blood in the inferior vena cava mainly passes through the foramen ovale. Blood from the superior vena cava mainly flows into the right ventricle.The deoxygenated blood is not disposed of in the lungs (which are as mentioned before full of fluid) but, in fact, crosses the placenta via the umbilical arteries.
Physiology of Birth
The first breath of the infant causes a rapid expansion of the lungs. This hugely decreases the resistance in the pulmonary vasculature. The molecular pumps (active transport) rapidly pull fluid out of the airspace through osmosis and into the interstitium. Oxygen causes a rapid dilatation of the pulmonary arteries which, in turn, decreases the pulmonary vascular resistance.
At this point, the sympathetic nervous system increases systemic vascular resistance. The differences in vascular resistance result in the transformation from fetal to adult circulation with the patent ductus arteriosus and patent foramen ovale closing over the first 1 – 2 days. After its close, the foramen ovale is referred to as the fossa ovalis. The ductus arteriosus will then close due to an increase in oxygen. There is also a decrease in the concentration of prostaglandins due to placental abruption. The prostaglandins PGE1 and PGE2 keep this ductus arteriosus open and their decreasing concentration results in the closure of this hole.
Physiology of Birth
Therapy/Management
Preparation for an infant resuscitation
Make sure you have obtained information about the prenatal history and delivery history. This includes a full history of the mother’s past medical history (previous cerebrovascular events for instance) and social history (e.g., are they an intravenous drug user – are they HIV positive?). The room should be set accordingly. There should be a warmer on standby, clean, dry cloth for drying, suction, airway equipment, etc. The physician should also know the gestational age and estimated weight in advance.




Comentários
Enviar um comentário