Maternal Physiological Changes During Pregnancy and Birth and Fetal Circulation
Table of Contents
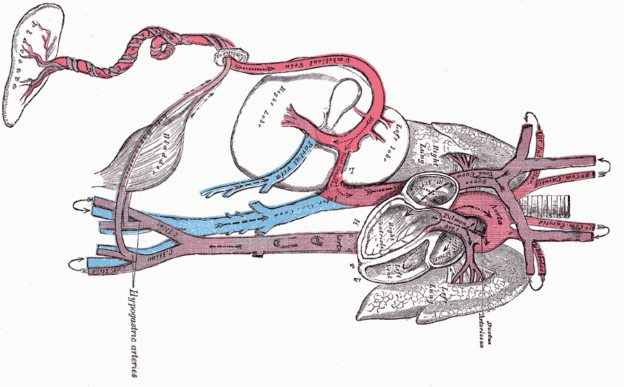
Image: “Circulation of a fetus.” by Henry Vandyke Carter, Henry Gray (1918) Anatomy of the Human Body. Bartleby.com: Gray’s Anatomy, Plate 502. License: Public Domain
Response of Mother’s Body to Pregnancy
Once a woman conceives and becomes pregnant, several physiological changes begin to occur in her body. This is not only to provide nourishment to the developing embryo, but is also an advance preparation of the parturition. The following are the major physiological maternal changes that occur during pregnancy:
The uterine size increases from 50g of non-pregnant female to about 1 kg. The vagina enlarges and the introitus opens more widely.
The breasts also become almost double in size with a 2 pounds increase in weight.
The average weight gain in pregnancy is 24 pounds; of which 7 pounds is of the fetus, 4 pounds of extra-embryonic structures, 2 pounds each of the uterus and the breasts, 6 pounds of the accumulated fluid and the remaining 3 pounds is the fat deposition in various parts of the body.
As the developing fetus removes substrates from the maternal blood, the desire for food is greatly increased. The basal metabolic rate (BMR) also increases by 15% during the later half of pregnancy. Hormones such as thyroxin, adrenocortical and sex hormones also contribute to increase in BMR.
Maternal body stores nutrients that are required by the fetus in the last trimester. The weight gain of the fetus almost doubles in the last trimester and so it requires an excessive amount of nutrients. A pregnant woman, in addition to having other nutrients, must take sufficient iron, calcium and vitamin D. In the later stage of pregnancy, she may also require vitamin K to prevent the newborn from hemorrhage during child birth.
Cardiac changes in pregnancy include
The cardiac output of the mother increases to 40% as the heart must supply additional blood to the placenta. Cardiac output, however, falls to a little above the normal value during the last 8 weeks of pregnancy with the maximum effect felt at 20-28 weeks of pregnancy. Vasodilatation also necessitates the increase cardiac output.
There is an increase in stroke volume by about 90% that leads to increase in left ventricular muscle mass and end diastolic volume but not end diastolic pressure.
There is a 10-20 increase in maternal heartbeat.
Blood pressure decreases in the first and second trimester and returns to normal levels in the third trimester.
Hematological changes in pregnancy
The maternal blood volume increases to 30% above normal during pregnancy. This is associated with a constant level of red blood cells hence a fall in the level of hemoglobin and hematocrit and red blood cell count. However, there is a normal level of mean corpuscular volume and mean corpuscular hemoglobin concentration. There is an associated fall in the level of thrombocytes and as such maternal pathological thrombocytopenia is below 100,000. The viscosity of blood also decreases.
Due to the above changes, pregnancy is associated with two-three-fold increase in iron requirement for hemoglobin synthesis and fetal development. Similarly, there is a need for increased folate up to 10-20 times and two-fold increased need for vitamin B12.
Pregnancy is referred to as a hypercoagulable or pro-thrombotic state. This is thought to prevent blood loss during parturitionand it begins in the first trimester all the way to 12 weeks post-partum.
The prothrombin time (PT) and activated partial thromboplastin time (APTT) decrease. There is an increase in procoagulant factors such as VIII, IX and X. Fibrinogen levels rise by up to 50% and fibrinolytic activity is decreased.
Venous stasis in the lower limbs is associated with vasodilation and decreased flow which is more marked on the left due to compression of the left iliac vein by the left iliac artery and the ovarian artery.
Respiratory changes in pregnancy
There is a 20% increase in oxygen demand during pregnancy that occurs due to 15% increase in BMR. Due to increased BMR during pregnancy, the minute ventilation also increases. Some of it is attributed to an increased level of progesterone, which is a direct respiratory stimulant. The PCO2 level in the blood decreases. As the growing uterus presses upon the abdominal structures, the change in shape of the diaphragm is limited. So, to maintain adequate ventilation, the respiratory rate increases.
Renal changes in pregnancy include
The 40% fall in systemic vascular resistance also affects the kidneys leading to increased renal blood flow and thus glomerular filtration rate(GFR) increases by 50% to excrete out excessive water and salts retained in the body due to hormonal changes occurring in pregnancy. This increase in blood flow causes and increase of kidney size by 1-1.5 cm. this may be accompanied by dilatation of the pelvicalyceal system.
Relaxin secreted from the corpus luteum and the placenta peaks in the first trimester to stimulate the formation of endothelin and vasodilatation of renal arteries.
Changes in the alimentary canal
Pregnancy is associated with increase in nausea and vomiting that is thought to be because of imbalance of hormones. It is also thought to be a protective mechanism against consuming any teratogenic substances. This phenomenon resolves by the 20th week of gestation in most people.
Endocrine changes
There is an increased level of all thyroid hormones thus pregnancy is considered a hyperthyroid state.
Reduction in vascular resistance activates the RAAS system causing a three-fold increase in aldosterone in the first trimester and a 10-fold rise in the third trimester.
The pituitary gland enlarges in pregnancy due to proliferation of prolactin producing cells in the anterior lobe.
Pregnancy is a diabetogenic state associated with increase in maternal glucose to supply the fetus and accompanying insulin resistance.
Skeletal and bone changes
Pregnancy is associated with reversible bone loss. There is increased bone turnover to supply the fetus with calcium.
Summary of maternal changes
Heart rate and stroke volume increase to maintain cardiac output and arterial pressure when systemic vascular resistance falls.
The inability of red blood cell production to keep pace with increasing plasma volume causes hematocrit to fall during pregnancy and leads to a physiological anemia.
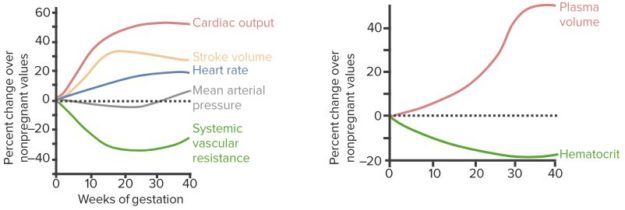
“Maternal Changes” Image created by Lecturio
Maternal Changes During Parturition
Parturition refers to the birth of the baby as a result of forceful uterine contractions. Two main effects which lead to the production of such contractions are hormonal changes and mechanical factors.
Hormonal factors
During pregnancy, the placenta produces estrogen and progesterone in excessive amounts. Estrogen promotes uterine contractility, while progesterone inhibits it. It has been hypothesized that, at the time of delivery, the ratio of estrogen to progesterone increases significantly which leads to initiation of uterine contractions.
The pituitary gland of the fetus produces oxytocin, while the adrenal glands produce cortisol. Both of them are the uterine stimulants and initiate uterine contractions.
At the time of labor, the fetal membranes secrete prostaglandins, which too will stimulate the cervix and the uterus.
Mechanical factors
When the smooth muscles of the uterus are stretched, their contractile power increases. The movements of the fetus cause intermittent stretch of the uterine wall. In a twin pregnancy, the average time of delivery is 19 days earlier than in single pregnancy. This emphasizes the importance of mechanical forces produced by the fetus.
When the fetal membranes are ruptured, the head of the baby is further pushed downwards causing stretching and irritation of the cervix. This results in the transmission of signals from the cervix to the uterus, either by the nerve reflexes or through direct myogenic transmission of signals.
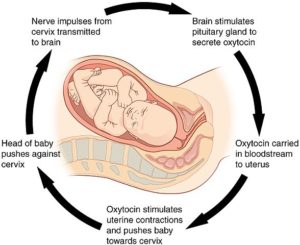
Initiation of Labor
The weak and rhythmical contractions of the uterus that occur throughout the pregnancy are called Braxton-Hicks contractions. However, at the end of pregnancy, these uterine contractions become stronger in amplitude and frequency and result in the dilatation of the cervix, which forces the baby out of the birth canal.
This process is known as labor. The normal duration of labor in a primary gravida is up to 24 hours and, when exceeded, the woman is said to be in an obstructed labor which requires urgent intervention. With multiple pregnancies, the duration of labor significantly reduces.
The process of labor has been explained on the basis of positive feedback mechanism.
As the fetal head descends down into the pelvis, it stretches the cervix. This stretch response causes uterine contractions. These uterine contractions begin from the fundus of the uterusabove and then propagate downwards, causing a further stretch of the cervical wall. This re-sends the signals to the uterus to produce another forceful contraction, stronger than the previous one. The cervix is stretched and dilated because of this vicious circle and finally, the baby comes out of the birth canal.
Another important event occurring during this process of cervical stretching is the signal transmission from the cervix to the hypothalamus, which results in the production of oxytocin hormone. This oxytocin hormone causes a stronger uterine contraction than the previous one, so every succeeding uterine contraction is stronger than the preceding one.
The pain signals from the uterus and the birth canal travel through the spinal cord to give signals to the abdominal muscles. These muscles contract forcefully, further aiding the passage of the fetus through the birth canal. The combined force of the contraction of the abdominal muscles and the uterus pushing the baby through the birth canal is around 25 pounds.
In the early part of labor, the frequency of uterine contractions is low, occurring after every 30 minutes, but, as the labor progresses, these contractions become stronger and may recur after every 5 minutes. These intermittent, rhythmic contractions of the uterus are of utmost importance as they prevent the blockage of blood flow to the fetus which may result in fetal death. Abusive use of oxytocin may cause uterine spasm resulting in fetal death.
The process of labor is divided into three stages:
- The first stage is the start of labor until full dilatation of the cervix (10cm), which is approximately equal to the size of the fetal head. This is the longest stage of labor prolonging up to 22-24 hours.
- The second stage is from the dilatation of the cervix until the expulsion of the fetus. This is the shortest phase of labor and is sometimes as short as one minute.
- The third stage is when the placenta is separated from the uterus and is expelled out. This may take up to 45 minutes. The positive feedback mechanism is illustrated in the diagram beside.
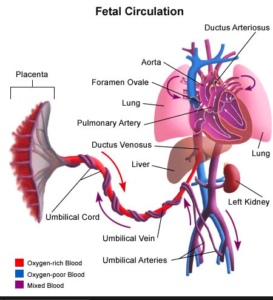
Fetal Circulation
During fetal life, the lungs are non-functional. Therefore, the fetus does not have the ability to oxygenate its blood. It gets the oxygen and other nutrients directly from the mother via placental circulation. The fetal circulatory system is therefore different from an adult circulatory system. There are several bypass mechanisms discussed below:
Image: “Fetal Circulation.” by KellyPhD – Own Work. License: CC BY-SA 3.0
Oxygenated blood, and other nutrients, travels through the placenta into the umbilical vein. The exchange of gasses occurs at this level.
Ductus venosus shunts the oxygenated blood away from the liver into the inferior vena cava.
The blood then enters the right atrium through the inferior vena cava.
Some of the blood goes directly to the left atrium via foramen ovale, which is a window-like opening between the two atria.
The remaining blood, which enters the pulmonary artery, re-enters the aorta through a connection between the two called ductus arteriosus. It shunts blood away from the lungs.
Mixed blood after supplying the head and the body travels back to the placenta via umbilical arteries. It then enters the maternal circulation.
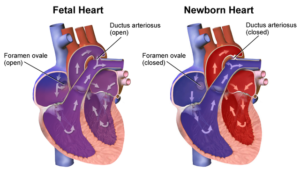
Changes at birth
The following structural changes occur at birth:
The first cry of the baby lets the air flow into the lungs. As a result, they expand and the blood starts flowing in the pulmonary arteries. The increase in pressure in the right side of the heart, and in the pulmonary artery, causes closure of foramen ovale and ductus arteriosus. Prostaglandins inhibition also plays an important role in their closure.
The functional closure of ductus venosus occurs at birth. However, its anatomical closure may take a week. The remnant of ductus venosus is called ligamentum venosum.
Image: “Changes occurring after the birth in a newborn heart.” by BruceBlaus – Own work. License: CC BY-SA 4.0
Adult circulation
In an adult, two circulatory systems flow simultaneously.
The deoxygenated blood, from different parts of the body, enters the right atrium via superior and inferior vena cava. From the right atrium, the blood flows into the right ventricle and is finally pumped into the pulmonary artery. The pulmonary artery takes the blood to the lungswhere it gets oxygenated. This is pulmonary circulation.
The oxygenated blood leaves the lungs and enters the left atrium via pulmonary veins. It then flows into the left ventricle and is then pumped into the aorta and to all parts of the body. This is called systemic circulation.
Comparison of fetal and adult circulation
In fetal circulation, the exchange of gasses occurs at placental level, while in an adult circulation, it occurs in the lungs.
In a fetal heart, there is higher pressure on the right side of the heart while, in adult circulation, the left side of the heart bears more pressure of the blood.
In fetal circulation, the lungs are bypassed by the foramen ovale and ductus arteriosus. In an adult, there are two circuits of blood.
In the fetus, the blood flowing is oxygenated, deoxygenated or mixed. Under normal physiological conditions, the adult blood is either oxygenated or deoxygenated.
Review Question
The correct answers can be found below the references.
1. A young pregnant lady, in the 3rd gestational month, came for a follow-up observation ultrasound to the gynecologist. She has HR 116/min, RR 28/min and a temperature of 99F. Which of the following would decrease during her pregnancy?
- BMR
- Hematocrit
- Blood pressure
- Cardiac output
2. A 9 month pregnant female came with a complaint of cramping pain in the abdomen since morning. The pain is now worse and bleeding has started. She has been examined by the duty doctor in the labor room and the head of the baby was seen on per vaginal examination. Which stage of labor is she in?
- Stage 1
- Stage 2
- Stage 3
- Stage 4
Comentários
Enviar um comentário