Acute Blood Loss — Causes, Symptoms and Treatments
Table of Contents
Etiology of Acute Blood Loss
Causes of Acute Blood Loss
Blood is constantly circulating through our bodies supplying vital organs with oxygen and nutrients. Damage to such blood providing vessels disrupts the integrity of the vessel walls. Usually, the body’s clotting mechanism aids in repairing and counteracting the damaged walls, however, when the amount damaged exceeds the clotting time, severe bleeding results.
Acute blood loss can be broken down into internal vs external bleeding. Internal bleeding occurs due to damage within tissues, organs or cavities. It is not easily identifiable and can go undiagnosed or unseen. In its worse form, increased amounts of bleeding may escape the compact heme system and collect in cavities or the body forming hematomas.
Most common reasons for internal bleeding arises from upper GI bleeds; these include bleeding ulcers, varices and diverticuli, bone damage, ruptured spleen subarachnoid hemorrhage, ruptured pregnancy, and malignancy. Other causes of internal bleeding includes physical damage which not always results in external damage or lacerations. These are harder to identify and bleeding may occur internally without any visual defects.
External bleeding, a bit more identifiable is the second major cause of acute blood loss. External bleeding results from any damage or trauma to the body resulting in identifiable blood loss from an open wound. These include lacerations, accidents, severed tissue and organs, lower GI bleeds, hematochezia, and hemorrhoids.
Pathogenesis of Acute Blood Loss
Anemia Evoked by Acute Blood Loss
Acute blood loss creates anemia due to two reasons. Primarily, the loss of red blood cells and secondly, a depletion of iron. The type of anemia from sudden blood loss is sometimes referred to as posthemorrhagic anemia. Hypovolemia is the largest threat, particularly to organs with large vascular supply. However, at this stage, hemoglobin isn’t affected so labs will not show anemia.
The body’s baroreceptors will initiate the release of vasopressin, shifting extravascular fluid to intravascular compartments. This results in hemodilution, changing hypovolemia to anemia. Plasma that was lost will be replaced by retaining volume in the kidneys. The anemia may be revealed by diluting the RBCs. Bone marrow response usually takes 5—7 days to respond with reticulocytosis.
In the worst case, the loss of > 20 % of blood leads to a hypovolemic shock. The cardiac output is soon decreased as a matter of too less blood volume being circulated. In response catecholamines, ADH and angiotensin II are released and lead to an increased peripheral vascular resistance. For that, the blood supply to the brain and heart stays stable, first the perfusion of the extremities (later on even inner organs) is reduced and results in impaired oxygenation.
The affected extremities and organs use the anaerobic metabolism and produce lactate. Precapillary dilatation and postcapillary constriction make the blood go into the capillary bed. This contributes to an even greater hypovolaemia.
Symptoms of Acute Blood Loss
Signs of Acute Blood Loss
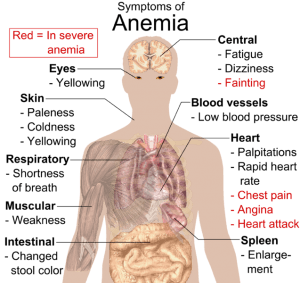
Image: “Main symptoms that may appear in anemia.” by Mikael Häggström. License: Public Domain
Acute blood loss signs and symptoms include a myriad of qualities. Initially, anemia isn’t present as blood plasma is lost with RBCs. However, as plasma and blood volume falls, anemia results. Primary symptoms of anemia with acute blood loss include dyspnea at rest or exertion, fatigue, bounding pulses, palpitations, lethargy, and confusion. Volume depletion due to bleeding can result in cramping, vertigo, syncope, and hypotension. The most feared complication of acute blood loss is volume depletion due to bleeding and can result in cramping, vertigo, syncope, and hypotension. The most feared complication of acute blood loss is a hypovolemic shock. The inability for adequate blood and volume load results in unperfused organs and decreased cardiac output, resulting in hypotension and end-organ failure. Angina and even cardiac arrest may occur.
Diagnosis of Acute Blood Loss
Labwork and diagnosis suggest a hemoglobin level < 7 g/dl as symptomatic and suggestive of acute anemia. MCV usually is normocytic ranging 80—100 in acute blood loss. Ultrasound and MRI/CT imaging can be performed to rule out bleeding locations if not visibly identifiable or hidden damage. Tagged RBC studies may also be performed to identify sources of GI bleeding.
Treatment and Management of Acute Blood Loss
Identifying the source of bleed and eliminating the hemorrhaging is the first priority. Stabilization is achieved by providing oxygen and cauterizing any bleeds. Once diagnosed with anemia due to acute blood loss, blood may need to be replaced. The body isn’t adaptable to the anemia as those with chronic anemia. Therefore, the body isn’t adaptable to the anemia as those with chronic anemia. Therefore, blood transfusion takes precedence. Hematocrit levels below 20 require blood transfusions. RBC transfusion is the most efficient way to regulate heme concentration; however, increases in mortality have been reported with those receiving transfusions.
Those with a hemoglobin level < 6.8 g/dl are usually the threshold for transfusions. Packed red blood cells (PRBC) may also be used to raise hematocrit levels.
Those with a hemoglobin level < 6.8 g/dl is usually the threshold for transfusions. Packed red blood cells (PRBC) may also be used to raise hematocrit levels.
Patients with acute blood loss should be monitored until stable; this includes monitoring O2 saturation levels, placing them on telemonitors and IV lines. Vasopressors are not given and are contraindicated. Pregnant patients with any acute blood loss must be given RhoGAM in cases of RH negative mothers due to the risk of the fetus’s interaction with the mother’s blood.
Review Questions
The answers are below the references.
1. A 43-year-old male was playing soccer when he suddenly fractured his knee. He received knee arthroplasty. Lab values before and after surgery are as follows, hemoglobin 17.2 before, 14.0 after, Hematocrit 90 before, hematocrit 75. Which of the following states his condition?
- Acute blood loss anemia according to the above-mentioned H/H levels
- No acute blood loss anemia according to H/H values
- Chronic anemia with concurrent acute blood loss anemia
- Iron deficiency anemia
2. A 24-year-old 28-week pregnant female was presented to the ER due to a slip and fall. She has a history of chronic anemia and vitamin K deficiency. The patient was complaining of tender flank pain and bruising in the lower abdomen and pelvic area. Which is the best immediate next step?
- Blood transfusion
- Treatment of RhoGAM
- Open laparotomy
- Physical examination and ultrasound
3. An 18-year-old male is brought to the ER after a motor vehicle accident. He is unable to ambulate and found to have a pelvic fracture on CT. While ortho is operating, the patient’s blood pressure drops significantly, has a normal central venous pressure and non-palpable veins. The patient is most likely suffering from?
- Hypovolemic shock
- Cardiogenic shock
- Transfusion reaction
- Septic shock

Comentários
Enviar um comentário