Scrotal Mass, Congenital- & Acquired Hydrocele and Spermatocele
Table of Contents
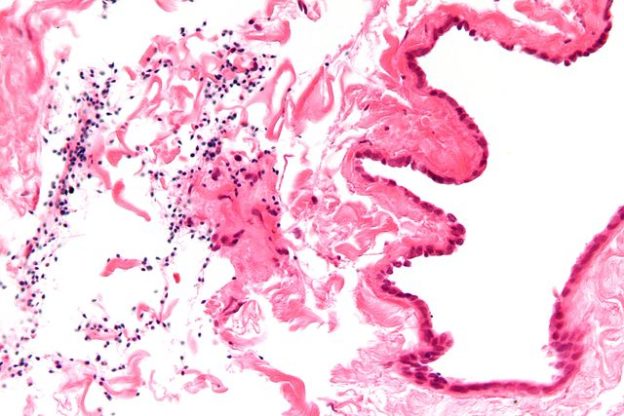
Image: “Micrograph of a spermatocele. The characteristic sperm are present (black dots – left of image). H&E stain.” by Unknown. License: CC BY-SA 3.0
Hydrocele
Definition
This is the pathological collection of fluid in the tunica vaginalis around the testes.
Pathogenesis
Various mechanical theories have been expatiated to explain the existence of hydrocele. The significant relevant ones are summarized below:
Classification
Hydrocele has been variously classified in literature. The simplest segregation is as follows:
- Primary hydrocele
- Secondary hydrocele
These chronic, longstanding relatively asymptomatic hydroceles are not secondary to any other defined primary pathology of the testes or the scrotum. They are usually painless and subsequently commonly subjected to ignorance and delay in seeking medical attention. However; long standing pressure atrophy of the testes has been documented and hence treatment is essential.
Primary Hydrocele
Other described hydrocele variants are as follows:
- Hydrocele of the hernia sac: Secondary to adhesions in the hernia sac; there is Loculated fluid collection present.
- Bilocular hydrocele: There is evidence of intercommunicating fluid collections on both sides of the neck of scrotum.
- Hydrocele of canal of Nuck: It is common in females around the round ligament and is always restricted to the inguinal canal.
Acquired Hydrocele
Also known as “secondary hydrocele”; it is often ancillary to an underlying primary pathology.
Various causes of acquired hydrocele can be tabulated as follows:
Secondary hydroceles usually subside upon treatment of the primary inciting pathology.
Symptoms
The most common presentation is that of a chronic scrotal mass that is progressively increasing in size and painless. The mass may be of differing size as in communicating hydrocephalus. They also presents with a fluid like collection in the scrotum that transilluminates. Other relatively rare symptoms are summarized as follows:
- Difficulty walking
- Traction like sensation; progressive heaviness and dull ache in the scrotum
- Infertility
- Difficulty in micturition
- Difficulty in intercourse.
Diagnosis
Hydrocele is a clinical diagnosis. Simple history and clinical examination often suffice to reach the diagnosis.
Classic clinical examination tests described for primary hydrocele can be summarized as follows:
Hydrocele fluid aspiration is usually not advocated due to obvious reaccumulation and recurrence. Once in a while in a morbid, elderly patient; aspiration of hydrocele fluid may be attempted. Ultrasonography guidance is preferred. Post-operative analysis of hydrocele fluid reveals the following characteristics:
- Straw color
- Albumin and fibrinogen rich
- Does not on clot
- Cholesterol abounds in long standing cases as mentioned in Filariasis.
- Tyrosine crystals may be present.
Ultrasonography is a useful adjunct in the diagnostic armamentarium of hydrocele. It often subserves as the confirmatory authority and also conclusively rules out common differentials of inguino-scrotal swellings.
Differential Diagnosis
Hydrocele is usually a simple straightforward clinical disease. Often however; closely related differentials can mar the diagnosis. These differentials are listed as follows:
- Spermatocele
- Testicular tumor
- Hernia
- Epididymal cyst
- Scrotal edema
Treatment
Hydrocele management is essentially surgical. It is relatively simple, definitive and curative. Various procedures have been described in the literature; all having withstood the test of time. They are as summarized below:
Sclerotherapy
Sclerotherapy ia an available alternative to surgical intervention; it has inferior results and higher morbidity. About 15-20 ml of 6% aqueous phenol is used in adjunct with lignocaine for additional analgesic effects. Use of tetracycline as sclerosing agent has fallen out of favor as the procedure incites considerable pain.
Complications
Hydrocele is a fairly benign disease with definitive treatment options. Rare but well described complications in literature can be summarized as follows:
- Pyocele
- Hematocele
- Infection
- Herniation of hydrocele sac
- Infertility
- Testicular atrophy
- Rupture
Spermatocele
Definition
Benign cystic accumulation of barley water like fluid containing spermatozoa and often is encountered at the superior aspect of the epididymis. This retention cyst is termed as “spermatocele”. They are usually unilocular in nature.
Often paratesticular in location, these fluctuant nodular cysts are formed by obstruction of rete testis or epididymal passages, resulting in diverticuli with sperm containing fluid. It is often the presence of debris within the cyst that distinguishes spermatocles from simple cyst of epididymis.
Pathogenesis
The exact etio-pathogenetic mechanism remains elusive. Potential hypotheses proposed are tabulated as follows:
- Idiopathic, arise from the efferent ductules of epididymis secondary to distal obstruction or primary distension of the epididymis
- Occlusion by agglutinated germ cells
- Gestational Diethylstilbestrol exposure
- Inflammation, trauma and subsequent epididymal scarring leading to adhesions and formation of loculated collections containing spermatozoa.
Classification
Spermatocele commonly arises from the head (caput) of the epididymis. Other potential locations for spermatocele help in topographical segregation as follows:
- Along the vas deferens
- Paratesticular in the scrotum.
Symptoms
Spermatocele usually presents as an innocuous unilateral scrotal swelling. It is typically asymptomatic. Often located postero-superiorly; it occasionally leads to aching discomfort and heaviness. It is not uncommon to find spermatocele as an incidental examination finding.
Diagnosis
Proper history taking and pertinent clinical examination usually suffice for small, classical, asymptomatic spermatocele situated on the postero-superior aspect. However, scrotal mass by itself many a times leads to psychological discomfort, anxiety and mild scrotal pain. These patients often demand confirmatory investigations.
Investigations often used as adjuncts to physical examination can be summarized as follows:
Differential Diagnosis
Differential diagnoses for spermatocele are listed as follows:
- Hydrocele
- Varicocele
- Epididymal cyst
- Inguinal hernia
Treatment
Various treatment strategies can be summarized as follows:
Hematocele
Intrascrotal collection of blood around the testes is termed as “Hematocele”. It often develops as an iatrogenic complication of surgical intervention on the scrotum. Occasional scrotal trauma can manifest as hematocele. Pain and history of precedent trauma to the scrotum help in diagnosis. Ultrasonography is the first and last investigation deemed necessary in diagnosis. Increased echogenicity with internal septae is characteristic.
Summary
Though potentially disturbing for males; benign scrotal masses often have definitive treatment available and good prognosis post-treatment. The most importunate fact is differentiation from malignant tumors. Majority of benign scrotal masses transilluminate. Ultrasonography often rules out testicular tumors.
Hydrocele is culmination of abnormal fluid accumulation in the tunica vaginalis surrounding the testes. It has a benign natural course. Surgical treatment is definitive, curative and relatively free of morbidity, complications and relapses.
Congenital hydrocele is secondary to persistent patent processus vaginalis with communication with the peritoneal cavity.
Acquired hydrocele is secondary to an underlying primary pathology. Timely treatment of the primary inciting factor often leads to regression of the secondary hydrocele.
Spermatocele is a benign retention cyst containing spermatozoa at the postero-superior aspect of the head of the epididymis.
While small asymptomatic spermatoceles can be expertly observed; spermatocelectomy in rest of the cases is definitive treatment option. Family completion is a pre-requisite for the same.
Hematocele is blood accumulation in the scrotum outside the testes. It is often secondary to trauma or iatrogenic insult to the scrotum and its contents.
Review Questions
The correct answers can be found below the references.
1. Which of the following procedure is best suited for small thin walled hydrocele?
- Jabouley’s procedure
- Observation
- Lord’s plication
- Sclerotherapy
2. Find the false statement:
- In funicular hydrocele, the hydrocele fluid communicates with the peritoneum at the internal inguinal ring but no communion persists with the tunica vaginalis.
- In infantile hydrocele, tunica vaginalis and PV are enlarged till the internal inguinal ring but there exists no communication between the PV and the peritoneal cavity.
- Hydrocele of the hernia sac is often secondary to adhesions in the hernial sac.
- Congenital hydrocele is due to congenital scrotal lymphatic blockage.
- Spermatocele contents resemble the following:
- Barley water
- Malt water
- It is straw colored fluid rich in cholesterol
- It is clear, serous fluid which is rich in iron and magnesium.
It was my last hope of having a child and Dr Obodo made my dreams come true. I asked for the spells, but didn’t tell my husband. We carried on trying to get pregnant as normal. I had a really good feeling about Obodo. I felt pregnant or like pregnancy was coming very about a week after the spells were cast. I began to vomit in the morning from morning sickness. I thought it was the toast. I’ve never felt like that before. And it was true! I went and grabbed the pee stick to show my husband. I went to my doctors at the earliest possible time to have a test and it came back positive. I immediately rang up my husband to let him know that the pee stick was not a false positive. He asked me how it was possible. He was certain that the pee stick was passed the expiry date. I told him all about Obodo, the fertility spells and he was amazed. We now have a very beautiful baby boy on the way and we are expecting to use Obodo in hope that I can have my baby girl. you can get in touch with doc via info ___ templeofanswer@hotmail . co . uk , call 234 8155 425481 for help
ResponderEliminarThank you,
The Messer Family