Hemolytic Disease of the Newborn (HDN) — Causes and Symptoms
Table of Contents
- Definition
- Epidemiology and Etiology of Hemolytic Disease of the Newborn
- Pathophysiology
- Clinical Presentation of Hemolytic Disease of the Newborn
- Diagnosis of Hemolytic Disease of the Newborn
- Treatment of Hemolytic Disease of the Newborn
- Prognosis and Prevention of Hemolytic Disease of the Newborn
- References
Image : “Newborn infant undergoing phototherapy to treat neonatal jaundice”by Martin Pot. License: CC BY-SA 3.0
Definition
It is a hematologic disorder of the fetus/ neonate that arises from alloimmunization/isoimmunization of the mother following blood group incompatibility with the fetus.
Epidemiology and Etiology of Hemolytic Disease of the Newborn
Fetal hemolytic disease (FHD) is more common among Caucasians than African-American babies due to the higher incidence rates of Rhesus negative mothers.
In mothers who do not receive prophylaxis, the overall risk of isoimmunization for Rh+ve ABO compatible infant with a Rh-ve mother is 16%. With :
- 1.5%-2% occurring in the antepartum period.
- 7% occurring within 6 months of delivery.
- 7% manifesting early in the consequent pregnancy.
Pathophysiology
Fetal blood is derived from the mother and the father thus, the fetus may have a different blood group from the mother. Incompatibility between maternal and fetal blood is the main cause of FHD. This incompatibility can be either AB0 blood group incompatibility or Rh factor incompatibility. Of these, Rh factor incompatibility is more common and more severe.
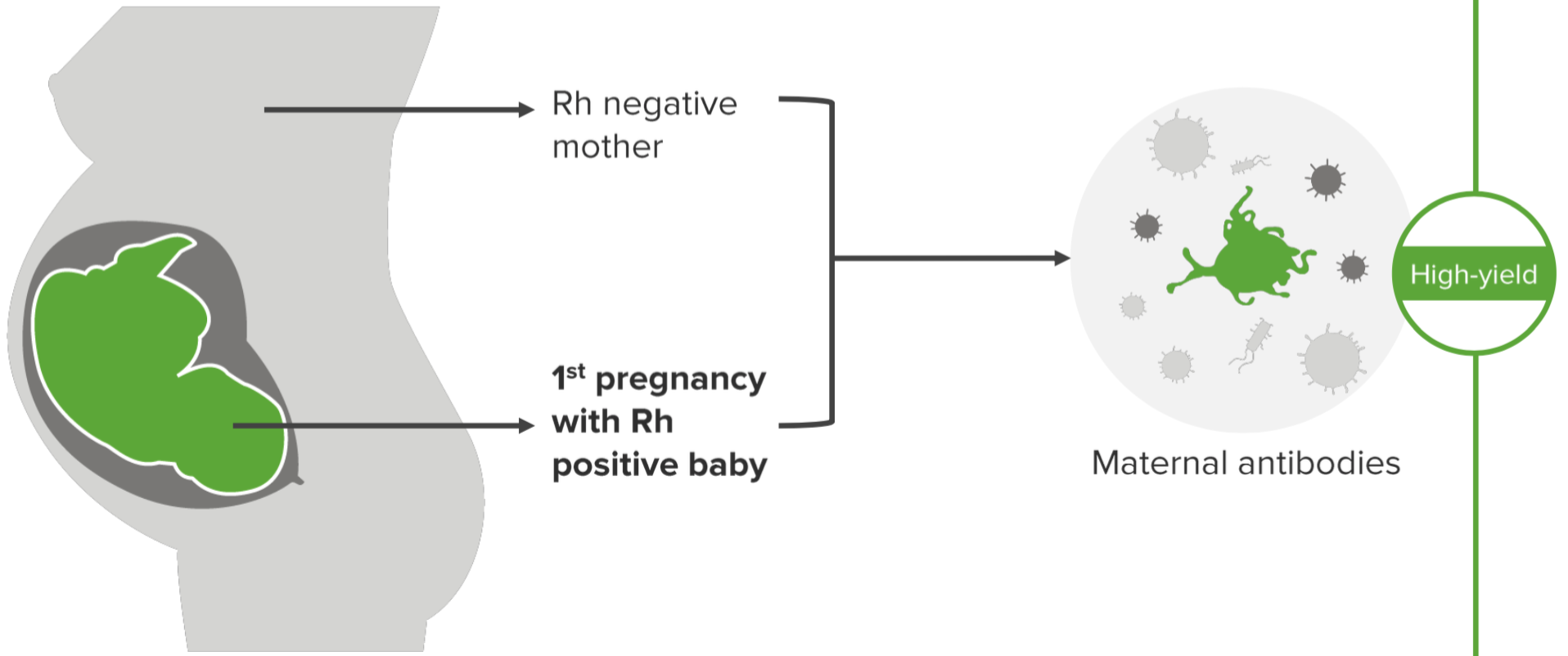
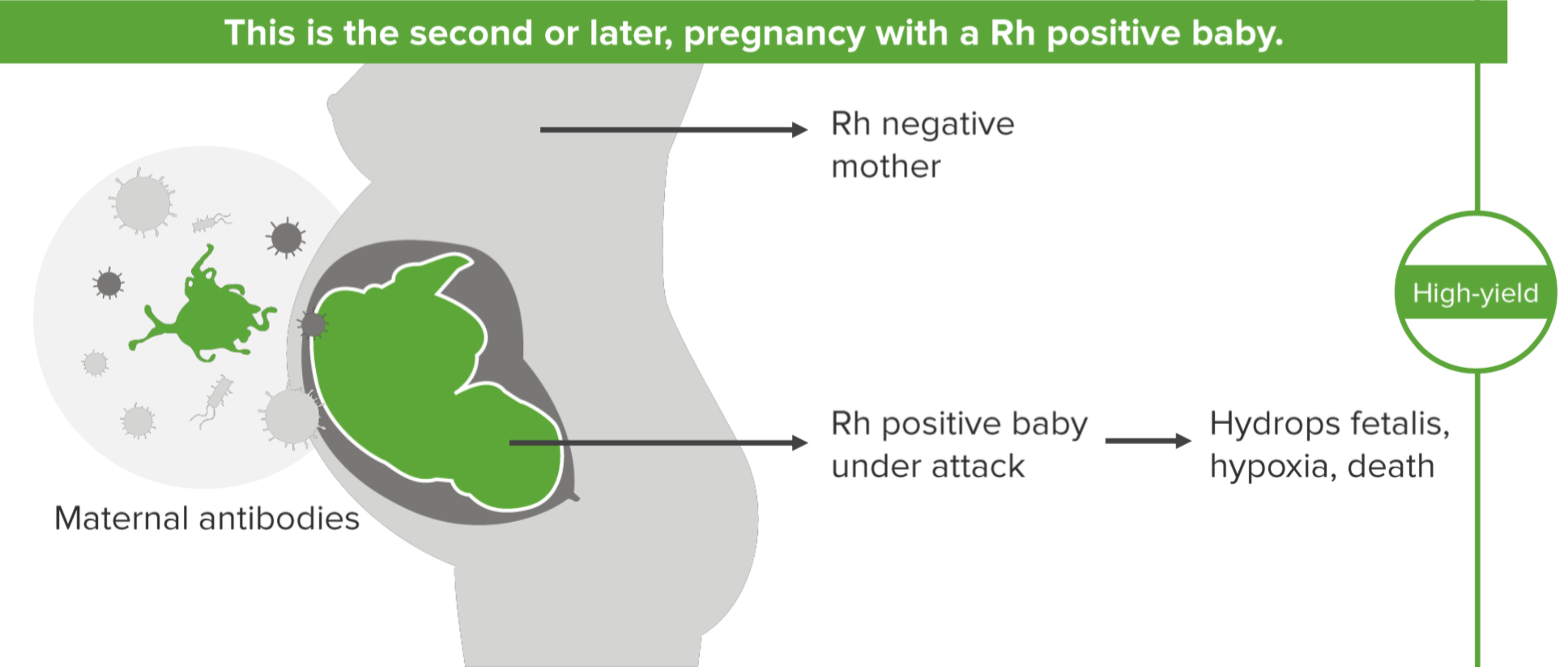
Rh factor incompatibility is reported commonly when the mother is Rh negative while the fetus is Rh positive. This incompatibility is due to several antigens, the D antigen being the chief culprit while other antigens like c, C, E and e may also be responsible. The maternal immune system responds to these antigens by forming IgM antibodies during the first encounter and these IgM antibodies do not cross the placenta. However, a subsequent exposure to the antigen triggers a release of IgG antibodies by the maternal immune system and these antibodies travel across the placenta to the fetal circulation, target the fetal RBCs causing lysisand FHD.
Maternal sensitization can occur :
- During delivery of aRh-negative fetus.
- During a prenatal bleed or miscarriage.
- After receiving a blood transfusion.
- During chorionic villus sampling or a procedure to terminate the pregnancy.
- When a small amount of fetal blood entering the maternal blood, stream is sufficient to cause maternal sensitization.
FHD secondary to AB0 incompatibility is less severe as compared to Rh incompatibility, as fetal RBCs have fewer AB0 blood group antigens than adults. Also, unlike Rh antigens, various fetal tissues express AB0 blood group antigens and so there is a lesser possibility for anti-A and anti-B to bind to the fetal red blood cell antigens.
Minor blood group incompatibility is a very rare cause of FHD and occurs due to E, c, Kell, Kidd or Duff antigens. The signs and symptoms of FHD secondary to minor group incompatibility are similar to those in Rh incompatibility, although hemolysis in anti-Kell disease can be more severe due to suppression of RBCs or excessive RBC hemolysis.
Clinical Presentation of Hemolytic Disease of the Newborn
Clinical presentation of FHD depends on the rate of hemolysis. The presentation can be grouped into:
- Fetal effects
- Neonatal effects.
The presentation can also be classified as mild, moderate, or severe FHD.
Mild FHD
When the rate of RBC hemolysis is well tolerated by the fetus, the symptoms and signs of FHD are mild. In the neonatal period, clinical features of mild anemia and hyperbilirubinemia can be noted and they usually resolve without intervention.
Moderate FHD
When the rate of RBC hemolysis is moderate during pregnancy, the fetal bilirubin levels are low as the placenta continues to filter the bilirubin from the fetal circulation. However, after birth, the immature neonatal liver cannot metabolize the excessive amount of bilirubin leading to hyperbilirubinemia and accumulation of bilirubin in the plasma and tissues.
Excessive bilirubin accumulation in the brain results in a condition called kernicterus, which can be potentially fatal or can lead to neurological deficits if the baby survives.
Severe FHD
When the rate of RBC hemolysis in utero is excessive, rapid, and prolonged, it leads to a constellation of problems that include:
Severe fetal anemia which stimulates fetal extramedullary hematopoiesis that produces high levels of nucleated red blood cell elements flowing into the fetal circulation.
The fetal liver and spleen overwork to compensate for the loss of the RBCs leading to hepatosplenomegaly, and later to hepatic dysfunction.
Sustained severe anemia eventually leads to high output failure with edema of fetal tissues (also called hydrops fetalis associated with low serum albumin levels), ascites and pleural effusion develops leading to respiratory failure followed by fetal demise.
Neonatal period
A baby born with FHD can present with
- Anemia due to destruction of RBCs.
- Hyperbilirubinemia (jaundice), coagulopathies, hypoglycemia (secondary to islet cell hyperplasia and hyperinsulinemia).
- Kernicterus.
Diagnosis of Hemolytic Disease of the Newborn
As several conditions can mimic the presentation of FHD, the diagnosis depends on detecting Rh or AB0 incompatibility thus blood grouping should be done.
During pregnancy, the diagnosis is based on:
- History of sensitization in the mother during previous pregnancy or current pregnancy
- Evaluation of maternal blood group and Rh factor
- Atypical antibodies test (AAT) results
- Direct Coombs test in a Rh negative mother. If anti-D is found, then Amniocentesis is performed to harvest fetal cells and detect the Rh status of the fetus.
- If the fetus is detected to be Rh positive, then it is monitored for the development of FHD by scheduling a fetal ultrasound at regular intervals and monitoring maternal anti-D levels. An increase in the titer of anti-D titer is an indication of active RBC hemolysis.
After delivery, the diagnosis and management is based on fetal testing:
- Complete blood count and reticulocyte count
- Serum bilirubin level
- Blood group and type
- Peripheral smear
- Coagulation profile
Laboratory findings in AB0 incompatibility which differ from Rh incompatibility:
- Peripheral smear shows microspherocytosis
- Direct Coombs test may be weakly positive
- Mean corpuscular volume
Differential diagnosis
- Alpha thalassemias
- RBC enzyme disorders like Glucose-6-phosphate or pyruvate kinase deficiency
- RBC membrane disorders like hereditary spherocytosis
- RBC hemolysis secondary to drugs, sepsis, TORCH infection, Parvovirus B19 infection
- Isoimmunization
Treatment of Hemolytic Disease of the Newborn
Intrauterine period
Fetal anemia is monitored in cases where FHD is detected. In-utero blood transfusion may be required repeatedly to treat the anemia. The transfusion is done using O-ve, washed, leukocyte depleted and irradiated blood via the umbilical vein.
Neonatal period
- Neonate may require frequent feeding as well as an intravenous fluid replacement.
- Exchange blood transfusion is indicated in severe hyperbilirubinemia to remove the excess bilirubin and antibodies.
- Phototherapy helps to metabolize the excess bilirubin in the tissues. Care of the neonatal eyes is vital to prevent retinal damage during phototherapy.
- Intravenous immunoglobulins are administered to prevent neonatal RBC destruction.
- Inotropic agents may be required, along with intravenous fluids to treat hypotension.
- Antibiotics if there is concomitant neonatal sepsis.
- Oxygen and surfactant with mechanical ventilation may be required in neonates with immature lungs.
Prognosis and Prevention of Hemolytic Disease of the Newborn
Prognosis of FHD is variable as some babies with mild disease are asymptomatic, while severe hemolysis with fetal hydrops can lead to intra-uterine or neonatal fetal death unless detected and treated early.
FHD is a preventable disease. Counseling Rh negative women, antenatal education and antenatal testing with indirect Coombs test plays an important role in its prevention. An Rh negative woman should be administered RhoGam around the 28th week of pregnancy, followed by a second dose within 72 hours of delivery if the baby is Rh positive. However, if the baby is Rh negative, then the second dose needs not be administered.
https://www.immunology.org/anti-d-1941-and-1968
https://www.stanfordchildrens.org/en/topic/default?id=rh-disease-90-P02498
https://www.nature.com/articles/pr2013208
https://extranet.who.int/rhl/topics/preconception-pregnancy-childbirth-and-postpartum-care/antenatal-care/who-recommendation-antenatal-anti-d-immunoglobulin-prophylaxis


Comentários
Enviar um comentário