Anatomy and Most Common Diseases of the Rectum and Anal Canal
Table of Contents
Macroscopic Anatomy of Rectum and Anal Canal
Location of Rectum and Anal Canal
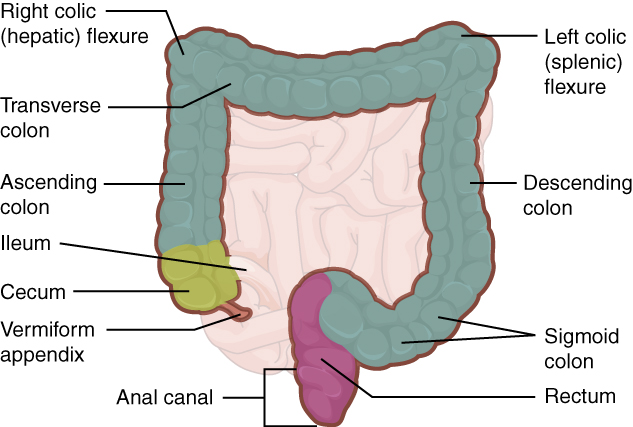
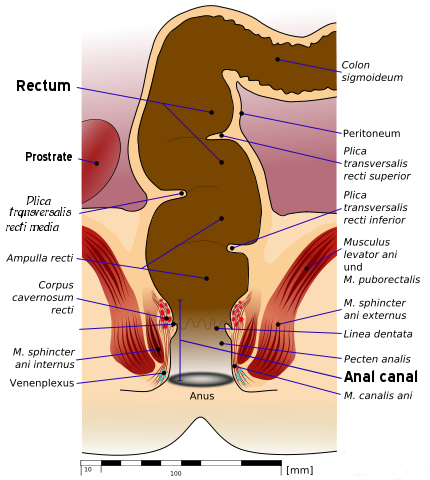
After the sigmoid colon, the large intestine passes on the level of the sacral vertebrae II/III into the 15-centimeter long rectum that lies directly anterior to the sacral bone (Os sacrum). In continuation with the rectum, the 3 – 4cm long anal canal (Canalis analis) follows. Both organs are located in the true pelvis and form the end of the intestinal tube.
Superficies of Rectum and Anal Canal
Despite its name (“straight intestine”), the rectum has several folds. In the sagittal plane these are:
Sacral fold (Flexura sacralis): Due to the close location to the sacrum the concave fold to ventral occurs.
Perineal fold (Flexura perinealis): Superior to the taint (Perineum) the convex fold to ventral occurs due to the caudodorsal fold of the rectum in continuation with the anal canal.
In the coronal plane three characteristic folds (Flexurae laterales) can be found, which correspond to a superior, middle and inferior transverse rectal fold of the mucosa on the inner side: Superior transverse rectal fold (from the left side), middle transverse rectal fold (from the right side) and inferior transverse rectal fold (from the left side).
The middle transverse fold is also known as Kohlrausch’s fold and is the most distinct. It is located circa 6cm superior to the anal aperture and is therefore still palpable. Rendering rectal carcinomas, which lie inferior to Kohlrausch’s fold, detectable during digital rectal examinations. Inferior to it the ampulla (Ampulla recti) begins.
Organization of Rectum and Anal Canal
The inferior part of the rectum is called anorectum and consists of the dilatable rectal ampulla and the following anal canal. A corrugated line palpable on the inner side, the anorectal junction, separates both segments. The mucosal surface has several features:
- Anal columns: Lengthways oriented mucosal folds; eight to ten pieces
- Anal valves: Small transverse folds at the inferior end of the anal columns; connect these and form the dentate line like this
- Anal sinuses: Recesses behind the valves with the ports of the proctodeal glands (Glandulae anales); also known as Morgagni’s columns
- Hemorrhoidal plexus: submucosal; arterial provided cavernous body located in the wall in the area of the anal columns
- Anal pecten: follows the anal columns; occurs whitely; is one centimeter wide and sensitive to touch and pain, small tears in this area (anal fissures) are very painful; border to the outer skin is the anocutaneous line
Blood Supply and Innervation of Rectum and Anal Canal
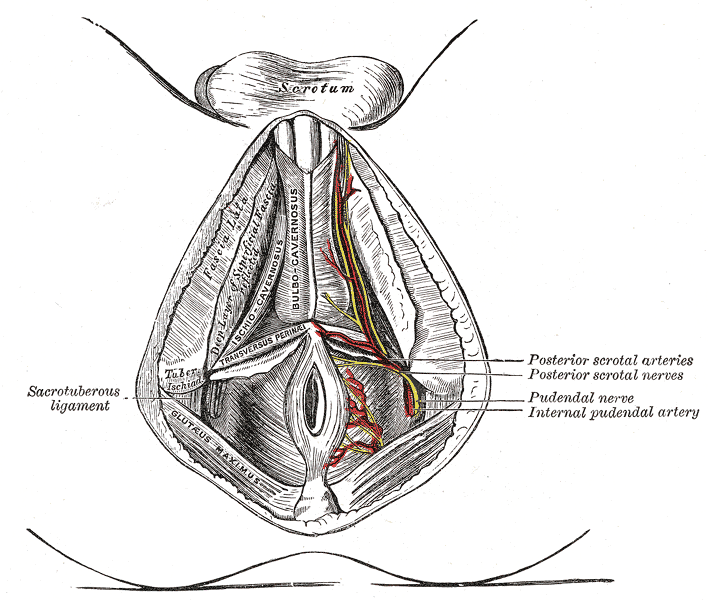
The arterial blood supply of the rectum and anal canal is ensured by five arteries in total with different origins. The biggest part of the rectum and the cavernous body are supplied by the unpaired superior rectal artery. It descends from the inferior mesenteric artery, reaches the rectum dorsally and divides into two smaller branches that arbors several times again in their course.
Out of the two internal iliac arteries, the left and right middle rectal artery reaches the rectum superior to the levator ani and particularly supply the inferior part of the ampulla.
The inferior rectal artery that descends from the pudendal artery, is also paired. Left and right inferior rectal artery reach the anal canal inferior to the levator ani and supply it as well as the sphincter muscles. The arteries form anastomoses with each other to compensate for the deficiency of one vessel with the other one.
The veins correspond with the arteries in their name and course. It is important to know that the superior rectal vein drains into the drainage of the portal vein via the inferior mesenteric vein, while the middle and inferior rectal veins drain into the vena cava via the iliac veins.
That is why rectal applied medications in form of suppositories must not be inserted too deep because they are resorbed by the superior rectal vein. This way they would be led to the liver first instead of directly to the systemic circulation, which would lead to an adverse first pass effect and to a diminution or even elimination of the pharmaceutical as a consequence.
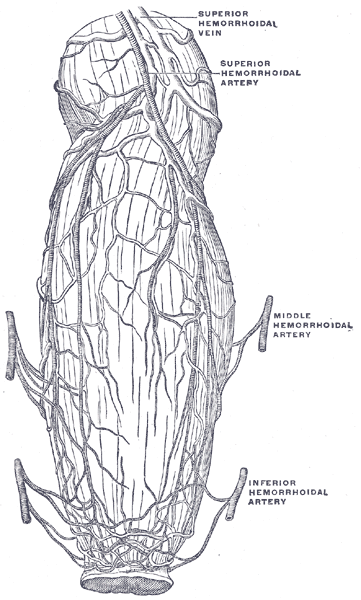
The blood vessels of the rectum and anus, which show the distribution and anastomosis of the intestine near end.
Furthermore, rectal carcinomas out of the superior rectum metastasize into the liver, while the ones out of the inferior rectum lead to metastasizes in the lungs. The two different drainages are connected by the rectal venous plexus. Portocaval anastomoses can be formed due to portal vein hypertension.
Tip: The venous drainage of the different parts of the rectum is a popular exam topic!
The sympathetic innervation is transmitted via the inferior mesenteric nerve plexus for the superior part of the rectum and via the inferior hypogastric plexus for the inferior part. Parasympathetically the rectum and anal canal are innervated by the pelvic splanchnic nerves out of the S2-S4 segments.
The somatic innervation for motor and sensory function is carried by the pudendal nerve.
Peritoneal Relations and Neighboring Organs of Rectum and Anal Canal
Ventral to the rectum lies the vagina and uterus in females or prostate, seminal glands and urinary bladder in males. While the superior part of the rectum is located retroperitoneally and sometimes a small part even intraperitoneally, the bigger inferior part with the rectal ampulla and the anal canal lies extraperitoneally.
This results, because a turnover of the peritoneum from rectum to the uterus (in females) or to the urinary bladder (in males) occurs at the perineal flexure. There a peritoneal recess is formed at the lowest point of the peritoneal cavity, the rectouterine pouch (of Douglas) in females and the rectovesical pouch in males. In females, the vesicouterine pouch is formed additionally due to the turnover of the peritoneum from the urinary bladder to the uterus.
According to the different peritoneal location of the rectum, you differentiate clinically a mobile rectum (retro- or intraperitoneal) and a fixed rectum (extraperitoneal). The rectum is surrounded by relocatable connective tissue, the paraproctium.
Microscopic Anatomy of Rectum and Anal Canal
The structure of the rectal wall principally corresponds to the rest of the digestive tract with mucosa, muscularis, and adventitia. But what the colon taenia lack, the rectum has a continuous longitudinal layer instead. Furthermore, there are no haustra and epiploic appendices. The transverse rectal folds correspond to the semilunar folds.
In the rectum, the whole colon has simple columnar epithelium with crypts and goblet cells, this area is called colorectal zone. At the supratransitional line, the rectal epithelium changes into the mucosal epithelium of the anal canal. This can be divided into three zones:
Transitional zone: On the level of the anal columns, between the supratransitional line and the dentate line; change from columnar to stratified non-keratinized squamous epithelium
Squamous zone (white zone): Between the dentate line and the anodermal line with stratified keratinized squamous epithelium; firmly grown together with the internal anal sphincter
Cutaneous zone (perianal skin): Inferior to the anodermal line with stratified keratinized squamous epithelium; strong pigmentation of the skin, sweat and sebaceous glands, hair follicles
Function of Rectum and Anal Canal
Continence
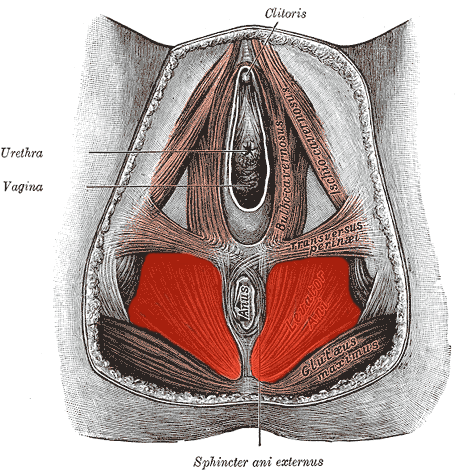
The closure of the anus is provided by different structures, which are called the continence organ in their entirety. This seals the straight intestine to not let solid, liquid and gassy intestinal contents outside. Following structures aid the continence organ:
Rectum and Anal Canal
Due to the S-shaped course of the rectum, the column of feces weighs on the pelvic diaphragm instead of on the anal canal. Furthermore, mechanoreceptors that register an incoming column of feces, are particularly located in the rectal ampulla. The skin of the anal canal is also dilatable.
Sphincter System
Three muscles participate in the closure of the rectum and anal canal, which belong to smooth and striated muscles:
Internal anal sphincter muscle: Smooth muscles (involuntary); continuation of the circular layer, sympathetically innervated; is permanently contracted due to missing parasympathetic ganglion cells
External anal sphincter muscle: Striated muscles (voluntary); subdivided into a deep, superficial and subcutaneous part; innervation by the pudendal nerve; surrounds the anal canal like a clamp and consequently leaves open only a longitudinal gap
Puborectalis muscle: Striated muscles; part of the levator ani; origin at the pubis, moves around the rectum from there on level of the anorectal junction and forms a muscle sling that strengthens the perineal flexure and constricts the rectum to a transversal gap; together with the longitudinal gap of the external anal sphincter the anal canal is closed crosswise
Cavernous body
The hemorrhoidal plexus, an arterially fed cavernous body, is located on the level of the anal columns in the submucosa. It is supplied by the superior rectal artery. The drainage occurs by arteriovenous anastomoses via veins that partly run through the sphincter muscles. During contraction of these muscles, the drainage of the cavernous body, therefore, is obstructed, it swells and the anal columns are put together. This particularly provides the gas-proof closure and therefore the finer continence.
Nervous control
The visceral in the somatic nervous system participates incontinence (s.a.).
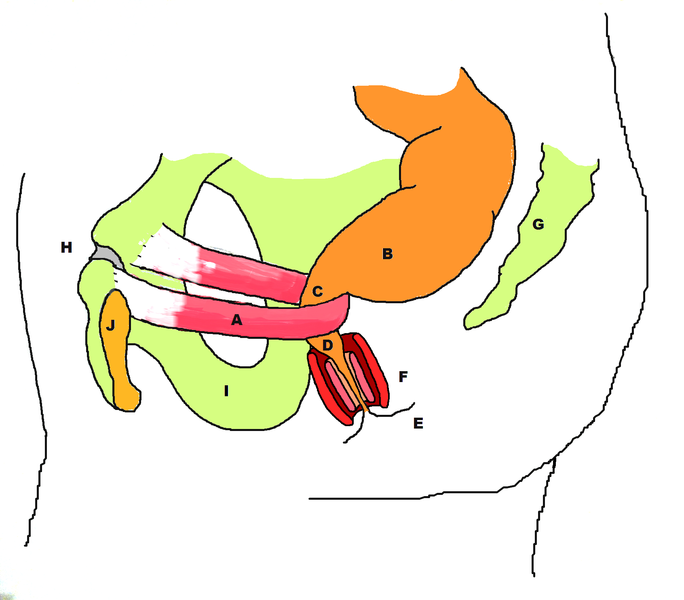
Picture: “Stylized depiction of puborectalis sling and its role in formation of the anorectal angle. Legend: A: puborectalis B: rectum C: level of anorectal ring and anorectal angle D: anal canal E: anal verge F: representation of internal and external anal sphincters G: coccyx & sacrum H: pubic symphysis I: Ischium J: pubic bone” by Tepi. License: CC BY-SA 3.0
When a bolus of feces arrives in the ampulla, the state of filling is registered by mechanoreceptors and is transmitted to the sensory cortex via the sacral cord, which signalizes the urge to defecate to the body. Due to the increasing pressure in the ampulla, the internal anal sphincter releases. The voluntarily innervated external anal sphincter and puborectalis muscles relax.
Due to the slackening of the sphincter muscles, the cavernous body is emptied. For expulsion of the column of feces, the parasympathetic peristaltic movements of the colon are assisted by the abdominal press, elevation of the pelvic diaphragm and contraction of the diaphragm. The feces is sensed according to consistency and volume in the white zone.
Diseases of Rectum and Anal Canal
Anal Abscess and Anal Fistula
Both clinical pictures occur due to an inflammation of the proctodeal glands which arises from the clogging of the anal glands drainage system by fecal matter. Anal abscesses can be classified as perianal, ischioanal, intersphincteric and supralevator types.
While the anal abscess is the acute form, the anal fistula is the chronic form that occurs in up to 50 % of the patients with anal abscesses. Anal fistulas can spread along the excretory ducts and have a connection to the outer skin and anal canal, unlike abscesses. Anal fistulas can be classified based on their relationship with various components of the anal sphincter as superficial, intersphincteric, transphincteric, suprashincteric and extrasphicteric. The symptoms of anal fistulas manifest in pruritus, weeping, and discharge of pus, mild to violent pain with fever and leukocytosis similar to anal abscesses.
The therapy happens surgically in both cases.
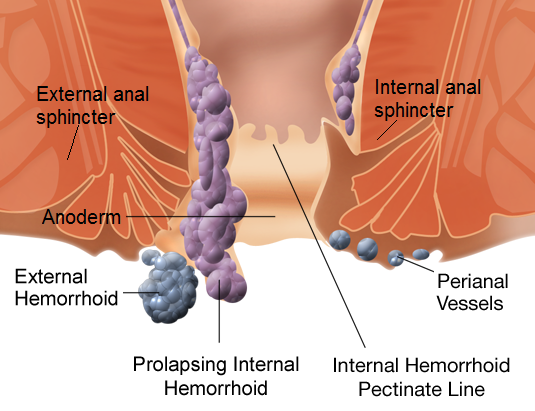
Hemorrhoids
Picture: “Types of hemorrhoids” by WikipedianProlific and Mikael Häggström. License: CC BY-SA 3.0
Hemorrhoids occur due to asymptomatic hyperplasia of the hemorrhoidal plexus. Symptoms include pruritus, stinging, pain or hemorrhages. Promoting factors for this are continuous pushing due to obstipation, pregnancy, alcohol and long periods of seated activity. The knotty transformations of the hemorrhoidal plexus are most often found at three, seven and eleven o’clock in the lithotomy position. The hemorrhoidal disease can be classified into four grades:
- Grade I: non-painful submucous cushions lying superior to the dentate line; only visible by proctoscope; conspicuously due to bright red blood in the feces
- Grade II: While pushing, the hyperplastic vascular cushions prolapse into the anal canal or outwards, which is connected with pain; spontaneous retraction
- Grade III: Prolapsed knots, which have to be restored manually
- Grade IV: Permanent prolapse (irreducible)
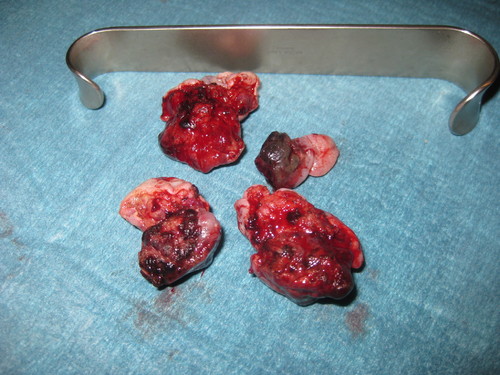
Picture: “Piles of 3rd degree.” by Dr. K.-H. Günther, Klinikum Main Spessart, Lohr am Main. License: CC BY-SA 3.0
With all four grades, there is a danger of complications in the form of massive hemorrhages. Furthermore, there can be an obstruction of draining vessels (hemorrhoidal vein thrombosis), inflammations, rectum prolapse and fecal incontinence due to sphincter muscle weakness. To ease the symptoms a treatment with ointments and suppositories is a possibility. Furthermore a dietary change in high fiber, low fat should follow.
Picture: “Resected hemorrhoid cushion after a hemorrhoid surgery by Milligan Morgan” by Dr. K.-H. Günther, Klinikum Main Spessart, Lohr am Main. License: CC BY-SA 3.0
For grade I and II of the disease sclerotization or rubber band ligation as semi-operative methods are used, while grade III and IV have to be treated surgically (hemorrhoidal ectomy).
Rectum Prolapse
It is a condition in which the rectum loses its attachment and protrudes out of the anal aperture with all its wall layers spontaneously or after defecation, it is called prolapse. Reason for this is an insufficiency of the pelvic diaphragm in most cases, which particularly occurs at older ages. The condition is more common among women aged 60 years and over. Other promoting factors are obstipation and an elongated colon.
The rectum prolapse is barely related to pain, but closely with fecal incontinence. The therapy is determined by the dimension of the prolapse and reaches from rubber band ligations to operative fixation of the rectum with the sacrum (rectopexy).
Picture: “Prolapse of rectum.” by Dr. K.-H. Günther, Klinikum Main Spessart, Lohr am Main. License: CC BY-SA 3.0
Rectum Carcinoma
Colorectal carcinomas are the second most common cause of cancer mortality in men and women. In contrast to colon carcinomas, rectal carcinoma is digitally palpable in many cases and therefore can be detected by a simple preventive check-up. Such a carcinoma often develops from adenomas (polyps), which describe benign pre-stages. Risk factors for the disease include advanced age, smoking, family history of the disease and inflammatory bowel disease.
The symptoms (loss of efficiency, loss of weight, fever) are very unspecific, which makes the diagnosis difficult. Most often the patients consult the doctor due to blood on the toilet paper, toilet or in the feces. A digital rectal examination should be realized immediately followed by a coloscopy.
Memorize: Blood in the feces can arise from hemorrhoidal disease, but can also be a hint for rectum carcinomas!
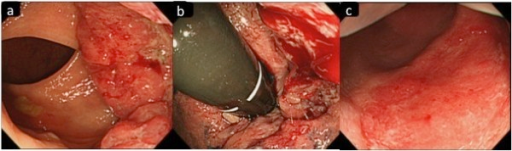
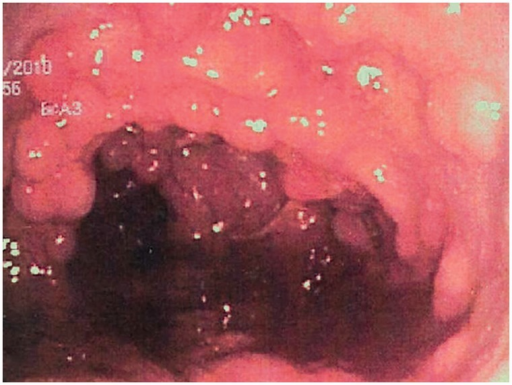
Picture: “Colonoscopy images. (a) Colonoscopy imaging shows a 3 cm in length, type 2 rectal cancer (b) that invades to the dentate line. (c) Repeated colonoscopy after chemotherapy shows an excellent response with only injected mucosal scar in the area of the previously identified rectal cancer.” by openi. License: CC BY 2.)
Exogenous risk factors include high intake of meat and fats, alcohol abuse, long-term smoking of cigarettes and being over 40 years. As endogenous risk factors are chronic inflammatory bowel diseases (Crohn’s disease, ulcerative colitis), colorectal carcinomas in the family history and adenomatous rectal polypes possible. The familial adenomatous polyposis (FAP) for example presents an obligatory precancerosis.
A cure can only be achieved by a surgical therapy. For infestation of the superior or middle rectal third, the rectum is only removed partly (rectum resection), while for infestation of the inferior third (tumor is less than six centimeters away from the anus) the whole rectum has to be removed (rectum extirpation) and an artificial anus to be created (anus praeter).

Picture: “Eight months after second surgery with transverse colostomy on the right side. The well-healed transverse scar on left side of abdomen may be seen.” by openi. License: (CC BY 2.5)
Examination of Rectum and Anal Canal
Digital Rectal Examination
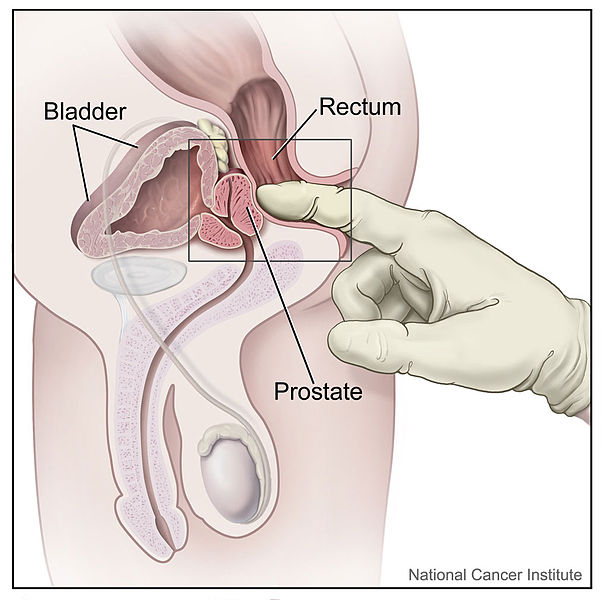
Picture: “Digital Rectal Exam (Male)” by Alan Hoofring.
The palpation of the rectum is an unpleasant examination for many patients, which is tainted with a lot of shame. Therefore educating the patient about the importance of the examination and the procedure should be mandatory. There are different possibilities for the patient’s position:
- Lateral Position: Maximal flection of the hip joints such as rectangular flection of the knee joints.
- Lithotomy Position: Tucked up and spread legs in supine position.
- Knee Elbow Position: Kneeling position, rest of hands and lower arms.
The examiner should wear gloves and use a lubricant. The finger is then gently inserted and led forward towards the abdominal wall. At the same time, there is to heed the tone of the sphincter muscles and the condition of the mucosa. In males, the prostate can be grouped and evaluated. After pulling the finger out, potential blood trails on this should be heeded. Furthermore, stool residues can be evaluated according to color and consistency.
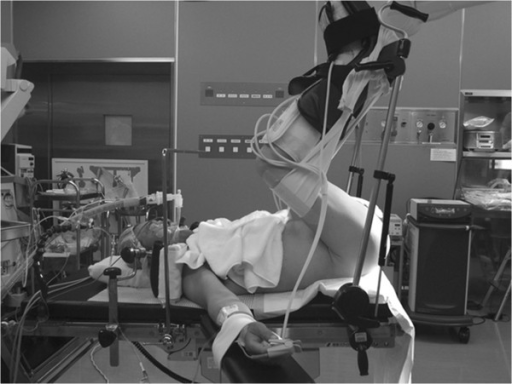
Picture: “The patient was placed in the exaggerated lithotomy position.” by openi. License: (CC BY 2.5)
Rectoscopy
For preparation, the intestine must be emptied by use of an enema or suppository that is preceded by a progressively light diet for three days. Prior to the procedure, consent is sought after explaining the procedure to the patients. During the examination, the patient should be in knee-elbow position or lateral position. The rectoscope is inserted under visual control and further advanced. To better evaluate the rectum and its mucosa, air is insufflated, and the intestine widened this way. Though the examination is unpleasant for the patient, it usually is barely painful.
Review Questions
The results can be found below the references.
1. Which statement about Kohlrausch’s fold is accurate?
- It is a mucosal fold of the sigmoid colon.
- It is also called superior transverse rectal fold.
- It protrudes into the rectal lumen from the left.
- Inferior to it, the anorectum begins.
- It is circa four centimeters superior to the anal aperture.
2. Which statement about the venous drainage of the rectum is not accurate?
- By the rectal venous plexus the drainages of the superior, middle and inferior rectal vein are connected with each other.
- While the superior rectal vein drains into the vena cava, the middle and inferior rectal veins drain into the portal vein.
- Due to portal vein hypertension, portocaval anastomoses in the area of the rectal venous plexus can be formed.
- The inferior rectal vein descends from the pudendal vein.
- The superior rectal vein is unpaired.
3. Hemorrhoids…
- …are adequate to a hyperplasia of the venous fed rectal cavernous body.
- …are extremely painful.
- …can lead to hemorrhoidal disease
- …are always treated with hemorrhoidal ectomy.
- …can be classified in five degrees of severity.



My name is Stephanie Brown I had Rectum effect and I was so worried am I going to die soon. I made my search on herbal remedy for rectum effect, then I found lots of testimonies on how Dr James Herbal Medicine cured diseases like Rectum effects, intestine damage, bowel obstruction, Ovarian disease, Cancer, hypothyroidism, Herpes, COPD, HIV, Arthritis, Lyme disease,Hpv, Infections,Liver Disease, Autoimmune Diseases, Parkinson's disease,Lupus,Nephrology and Hypertension, Neurology, Obstetrics, Gynecology, and Women's Health, Oncology, Pediatrics, Pulmonary, ACUTE MYELOFIBROSIS, ALZHEIMER's symptoms, BREAST CANCER, DIABETES, HAIR LOSS AND HAIR TREATMENT, KIDNEY DISEASES, LEUKEMIA, MYELOID LEUKEMIA, STEM CELL TREATMENT , On websites sharing their testimonies, which made much more sense to me. All the authors pronounce Dr James As a man with Good Heart, I picked interest in their testimonies and I contact him about my situation then he gave me procedure how it works, I proceed after one week he courier his Herbal Medicine to me and instructed me on how to drink it for two weeks to cure. I received His Herbal Medicine so I drank it for two weeks as I was told then after 2 weeks of drinking his medicine, I went for a test I found out I was cured from Rectum effect, I paid homage to his country to celebrate with him on his African festival which he told me it usually happens every year. I know there are lots of diseases denials of Herbal Remedy movement the same few doctors and they represent a very small fraction of the community. I could have died because I refused Natural Herbs Cures for so long, but luckily, by the grace of God I am alive to tell my story. Contact Info...Whatsapp Number...+2348152855846,Email...drjamesherbalmix@gmail.com
ResponderEliminar