Urologic Cancer — Surgical Treatment
Table of Contents
- Background of Urologic Cancer
- Epidemiology of Bladder and Prostate Cancer
- Pathophysiology of Bladder and Prostate Cancer
- Grading and Staging of Bladder and Prostate Cancer
- Clinical Presentation of Bladder and Prostate Cancer
- Screening for Bladder and Prostate Cancer
- Diagnostic Workup for Bladder and Prostate Cancer
- Management of Bladder and Prostate Cancer
- References
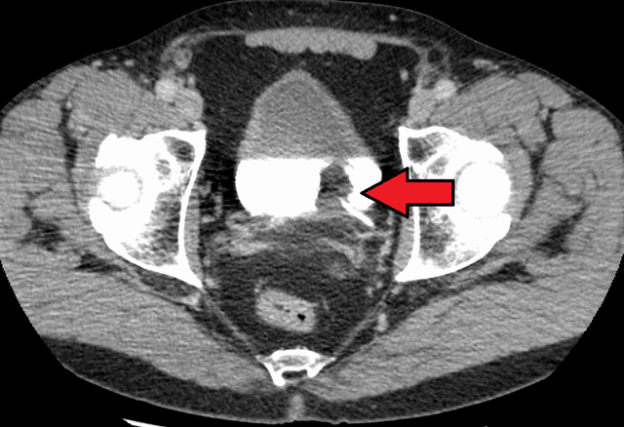
Image : “Transitional cell carcinoma of the bladder. The white in the bladder is contrast.” by James Heilman, MD. License: CC BY-SA 4.0
Background of Urologic Cancer
Bladder cancer
While the bladder is elastic and can expand considerably as it gets filled with urine, the third layer of smooth muscle makes the bladder capable of contraction when needed. Bladder cancer typically arises from the innermost layer of urothelial cells and can be classified into superficial or invasive carcinoma.
Superficial bladder cancer
Superficial bladder cancer is usually limited to the first two layers, whereas invasive bladder cancer extends into the third muscular layer. Obviously, the risk of metastasis is higher with invasive bladder cancer. Superficial bladder cancer might protrude towards the lumen. This type of cancer is known as papillary superficial bladder cancer. Flat superficial bladder cancer is a tumor that does not project into the lumen of the bladder. Flat carcinoma has a higher risk of invading the outer layers of the bladder and to metastasize.
Prostate cancer
The second urologic cancer we are concerned with in this article is prostate cancer. Prostate cancer has been rated as the most common non-cutaneous cancer in men. Prostate cancer, as the name implies, is a malignant neoplasm that arises from the prostate gland. Most cases of prostate cancer are identified via routine screening.
The prostate is found below the urinary bladder and it surrounds a part of the urethra known as the prostatic urethra. This explains why prostatic hypertrophy, or the presence of a prostatic mass, causes urinary symptoms such as urgency, frequency, post-dripping, or even urinary obstruction. The prostate is surrounded by a capsule and is near the rectum; hence, it can be palpated by digital rectal examination. Up to 95% of prostate cancers are adenocarcinoma. The rest are found to be of urothelial cell origin, i.e. transitional cell.
Epidemiology of Bladder and Prostate Cancer
Occurrence
The estimated incidence of bladder cancer in the United States is around 17.7 per 100,000 in whites and 9.2 per 100,000 in blacks. Ethnic differences in the incidence of bladder cancer have been long recognized by epidemiological scientists and they can be explained by several factors.
American Indians seem to have the lowest incidence of bladder cancer, i.e. 2.6 per 100,000. The risk of bladder cancer is considerably higher in men. The male to female ratio has been estimated to be around 3 to 1. Up to 3.4% of men are expected to develop bladder cancer in their lifetime.
This can be related to hormonal differences or occupational exposures. Bladder cancer is most commonly seen in patients older than 70 years of age; however, it might be diagnosed in patients aged between 55 and 69 years of age. People aged between 30 to 54 years are twenty times less likely to develop bladder cancer compared to those who are older than 70 years.
Risk factors
Mortality is quite high in people with bladder cancer, mainly due to delayed diagnosis. The estimated mortality rate in the United States is around 3.2 per 100,000. The most important risk factor for bladder cancer is cigarette smoking. Occupational exposure to benzene derivatives and arylamines also put the person at an increased risk of bladder cancer and has been reported as a possible risk factor in up to one-quarter of the cases of bladder cancer. Workers involved in dyes, rubbers, paints, leathers, and textiles industry have an increased risk of developing bladder cancer as well.
The use of hair dyes by women has been also associated with an increased risk of bladder cancer, especially in women who have been using them for longer than 15 years. Arsenic contaminated water in the developing world also increases the risk of bladder cancer. Men with certain polymorphisms in cytochrome p450 isoenzymes and glutathione transferase are at an increased risk of bladder cancer.
Prostate Cancer
The family history of bladder cancer can also put the person at an increased risk of bladder cancer. Prostate cancer is considered as the most common non-cutaneous cancer in the United States in men. The lifetime incidence of prostate cancer in white men is one in six, and, in black men, is one in five. Most cases of prostate cancer occur in men older than 50 years of age. The current estimated annual incidence of prostate cancer in the United States is 150 per 100,000. In the last decade, the incidence of low-risk prostate cancer has declined, whereas the risk of metastatic prostate cancer seems to have increased.
Ethnic differences in prostate cancer incidence exist. African-Americans have a mortality rate that is twice what is found in whites. The prognosis of prostate cancer is dependent on the Gleason grade.
Genetic predisposition has been also suggested as an important risk factor for prostate cancer. Several genes on chromosomes 1, 17 and X-chromosome have been associated with prostate cancer. A family history of prostate cancer also puts the person at an increased risk. Increased fat intake and obesity are two modifiable risk factors associated with an increased risk of prostate cancer.
Pathophysiology of Bladder and Prostate Cancer
Bladder cancer arises from transitional cells which compose the urothelial innermost layer of the bladder; therefore, the most common type of bladder cancer is urothelial. Adenocarcinoma, squamous cell carcinoma, leiomyosarcoma, and rhabdomyosarcoma are rarely seen in the bladder. Genetic alterations in chromosome 9 and the cyclin cycle regulatory protein have been found in urothelial cancers of the bladder. Over-expression of vascular endothelial growth factor has been also reported.
The over-expression of this factor explains why such tumors are usually rich in blood vessels. Protein p53 is also over-expressed in bladder cancer.
Prostate cancer ensues when the rates of cell division and death are no longer equal. Protein p53 has been found to be over-expressed in prostate cancers. In contrast to bladder cancer, the most common type of prostate cancer is adenocarcinoma. Urothelial cancers are recognized in only 4% of the cases of prostate cancer.
70% of prostate cancers are found in the peripheral zone. The remainder is distributed equally between the central and the transitional zones. In practice, multifocality is a common finding with prostate cancer and the involvement of multiple zones is quite often. The extension of prostate cancer is dependent on the location of the tumor. Tumors from the peripheral zone tend to invade the ejaculatory ducts and seminal vesicles. Transitional zone tumors typically invade the bladder neck. For unknown reasons, prostate cancer is more likely to spread to the bones before any significant lymphadenopathy even develops.
Grading and Staging of Bladder and Prostate Cancer
The national cancer institute has published a staging system for superficial and invasive bladder cancer. The following table summarizes the staging of bladder cancer:
Superficial Bladder Cancer
Invasive Bladder Cancer
Risk stratification of superficial bladder cancer patients is very important as it has a huge impact on the management plan. The following table, which is adapted from Lee and Droller, Pow-Sung and Sigma, and Kurth et al works, summarizes the most recent risk stratification system for superficial bladder cancer:
The most important prognostic scoring system for prostate cancer is the Gleason grading system. The following table summarizes the Gleason score for prostate cancer:
Clinical Presentation of Bladder and Prostate Cancer
The most important clinical finding in a patient with a bladder cancer is hematuria. Suprapubic discomfort due to bladder irritation. Incomplete voiding feeling is commonly seen in patients with bladder tumors that invade the bladder neck.
The main clinical manifestations of prostate cancer are urinary retention, back pain, and hematuria. Urinary retention is usually progressive and the patient might complain of incomplete voiding feeling. A digital rectal exam is not accurate in the differentiation between benign prostate hypertrophy and prostate cancer. In fact, most patients with prostate cancer have a normal digital rectal exam.
Screening for Bladder and Prostate Cancer
The goal of screening in bladder and prostate cancer is to detect cancer at an early stage where surgical or radiological intervention might be curative. In the United States, screening of the general population for bladder cancer is not being performed. The main reason behind not recommending routine screening for bladder cancer is the fact that most patients can be adequately managed at the time of diagnosis. Additionally, screening of high-risk populations failed to show any added benefit, an increase in detection rate, or better outcomes.
On the other hand, screening for prostate cancer might have some added benefits. Regardless, the topic of screening in prostate cancer remains controversial. The current recommendations for screening for prostate cancer are to start screening in men older than 50 years of age and younger than 76 years of age. A digital rectal examination is recommended in this age group. Prostate-specific antigen levels above 3 mg/L are worrisome for the physician and they indicate further diagnostic workup to exclude prostate cancer in this age group.
Diagnostic Workup for Bladder and Prostate Cancer
Laboratory investigations are not very helpful in a patient suspected to have bladder cancer. Instead, one should opt for urine cytology looking for the presence of malignant or suspicious cells. The diagnosis of bladder cancer is usually confirmed by cystoscopy. Papillary tumors are generally resected via transurethral approach and later staged. In other kinds of tumors, the goal of cystoscopy is to simply obtain a biopsy for staging and histopathologic examination.
The usability of prostate-specific antigen in the confirmation of the diagnosis of prostate cancer is questionable; therefore, an elevated prostate specific antigen is indicative of further workup but is neither diagnostic nor correlated with the grade of prostate cancer. The best diagnostic modality of prostate cancer is a transrectal ultrasound-guided biopsy.
Because prostate cancer can be multifocal, multiple cores should be taken. A histopathologic examination is then performed to confirm the diagnosis and score the tumor based on the Gleason score. Bone scans and positron emission tomography are used to detect bone metastasis. Computed tomography scans of the pelvis and abdomen or magnetic resonance imaging studies are useful in detecting adjacent organ involvement.
Management of Bladder and Prostate Cancer
The mainstay treatment of bladder cancer is surgery, and surgery is usually the only curative treatment for early bladder cancer. The two most commonly performed surgeries are transurethral resection of bladder tumor (TURBT) and radical cystectomy with lymph node dissection. The decision to go to a minimally invasive approach such as TURBT is dependent on the absence of muscle layer invasion on staging. Patients with T4 stage tumors usually need radiotherapy. Patients with T4 stage tumors and distant metastasis usually go for radiotherapy alone.
Like bladder cancer, the treatment of prostate cancer is also dependent on the presence of metastasis. Patients without prostatic cancer metastasis might either go for prostatectomy or radiation therapy alone. High-risk patients with comorbidities should receive radiotherapy instead of surgery. Radiotherapy alone or prostatectomy are equally effective and curative for localized prostate cancer.
Comentários
Enviar um comentário