Coarctation of the Aorta (CoA) in Children — Symptoms and Treatment
Table of Contents
- Overview
- Epidemiology of Coarctation of the Aorta
- Classification of Coarctation of the Aorta
- Pathophysiology of Coarctation of the Aorta
- Clinical Presentation of Coarctation of the Aorta
- Diagnostic Workup for Coarctation of the Aorta
- Differential Diagnosis of Coarctation of the Aorta
- Treatment of Coarctation of the Aorta
- Complications of Coarctation of the Aorta
- References
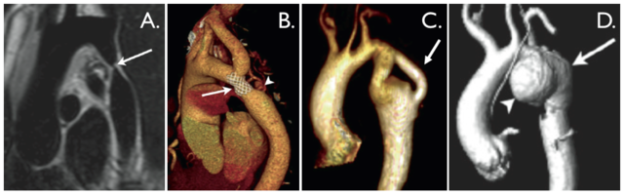
Image: “Aortic
coarctation. A. ‘Black-blood’ oblique sagittal view showing discrete,
tight coarctation at the aortic isthmus (arrow). B. 3D,
contrast-enhanced CT angiogram showing mildly narrowed bare metal stent
(arrow) that partially overlies the left subclavian artery origin. The
arrowhead shows a subtle pseudo-aneurysm at the distal end of the stent.
C. 3D, contrast-enhanced MR angiogram showing aortic arch hypoplasia
and coarctation with a ‘jump’ by-pass graft posteriorly (arrow). D. 3D,
contrast-enhanced MR angiogram showing large pseudo-aneurysm (arrowhead)
after previous patch angioplasty repair. The true lumen is shown
posteriorly (arrow).” By Hopewell N Ntsinjana , Marina L Hughes and Andrew M Taylor. License: CC BY 2.0
Overview
Coarctation of the aorta (CoA) is characterized by the abnormal constriction of the aorta due to localized medial layer thickening.
This constriction might appear as a shelf-like structure or a
membranous curtain-like structure. The involved region might be discrete
or it can be a long segment. A discrete short segment of CoA is the
most common form of the condition.
Epidemiology of Coarctation of the Aorta
CoA is one of the common forms of congenital heart disease with an
estimated incidence of 6–8% among patients with congenital heart
disease. CoA is more common in European and North American countries
compared to Asia.
The condition is more common in boys. The incidence
of CoA in symptomatic infants is not different between the two sexes.
The most common age of presentation is five years. Young children
usually present with congestive heart failure while adults are more
likely to present to the clinic because of persistent hypertension.
The condition might be isolated or more commonly associated with
other congenital heart defects such as a bicuspid aortic valve and
ventricular septal defects. The condition can cause symptoms of impaired peripheral circulation in young infants and can be associated with significant mortality due to the increased risk of congestive heart failure.
Patients with CoA are at an increased risk of developing subacute
bacterial endocarditis, hypertension and have a slightly decreased
survival curve compared to healthy individuals. It is estimated that up
to 90% of the patients with CoA who do not undergo surgical treatment
die by the age of 50 years.
The patient’s age at presentation, the size of the involved segment
and the presence of other preexisting heart defects are the most
important predictors of mortality and morbidity in patients with CoA.
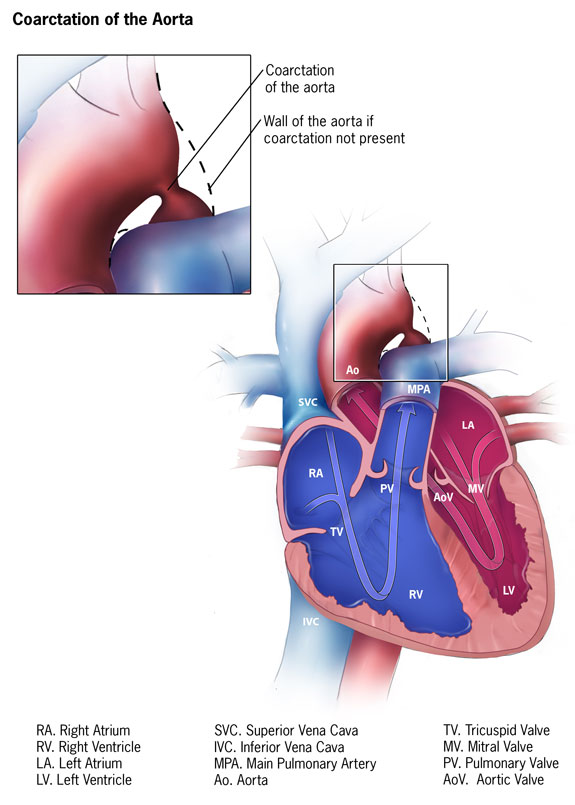
Classification of Coarctation of the Aorta
The coarctation of the aorta can be classified into three main types:
Preductal coarctation
This type of aortic narrowing occurs proximal to the patent ductus arteriosus. As
the blood flow to the aorta distal to the coarctation is dependent on
the ductus arteriosus, severe narrowing of this type can be
life-threatening.
The main reason for this type of coarctation is an intracardiac anomaly during the fetal life,
which eventually decreases the blood flow through the left heart side,
making the hypoplastic development of the aorta. 5% of the infants with
Turner’s syndrome also suffer from this type of coarctation.
Ductal coarctation
In this type of coarctation, the aorta narrows at the insertion of
the ductus arteriosus. Ductal coarctation basically arises at the
closing of ductus arteriosus.
Postductal coarctation
In this type of coarctation, which is more prevalent in adults, the
aorta narrows distally to the point of insertion of the ductus
arteriosus. In postductal coarctation, although ductus arteriosus is
open, the blood flow to the lower parts of the body is impaired.
The other associated conditions with this type of coarctation are
hypertension in the upper limbs, notching of the ribs (due to collateral
circulation) and weak pulses in the lower limbs.
The main reason for this coarctation is the development of a muscular artery into an elastic artery during fetal life,
which leads to the fibrosis and coarctation of the ductus arteriosus
upon birth, thus narrowing the aortic lumen. Aortic narrowing can
present in the forms of either aortic coarctation or aortic stenosis.
Pathophysiology of Coarctation of the Aorta
The exact etiology of CoA is unknown in most cases, but certain risk factors have been linked to the condition. Turner syndrome and Takayasu arteritis are two possible diseases that have been associated with an increased risk of CoA.
Patients with CoA have a significantly increased afterload pressure
on the left ventricle. This is associated with increased stress on the
left ventricular wall and ventricular hypertrophy. Eventually, it can
put the patient at an increased risk of developing congestive heart
failure.
Patients with CoA are at an increased risk of developing persistent hypertension.
The exact mechanism of hypertension in this group of patients is poorly
understood. It is, however, noted that patients with CoA usually have
an exaggerated activation of the renin-angiotensin system which might
explain why they have persistent hypertension.
Patients with CoA might eventually develop a slight improvement in
their symptoms due to the formation of arterial collaterals that pass
the obstructed region of the aorta.
Clinical Presentation of Coarctation of the Aorta
Patients with other congenital heart defects are more likely to present earlier to the clinic. Symptoms of the early presentation of CoA include:
- Difficulty during feeding
- Tachypnea
- Development of congestive heart failure
Patients who have severe CoA might present with acute congestive
heart failure, especially at the time of ductus arteriosus closure.
Patients presenting with CoA later in life are usually diagnosed
incidentally while they are being investigated for persistent
hypertension. At this stage, patients can complain of headaches, chest
pain, and fatigue. Due to the association between CoA and intracerebral
aneurysms, the presentation of CoA in some patients can be that of
life-threatening intracranial hemorrhage.
Patients who present late to the clinic might have a pressure
difference between the arms and legs of more than 20 mm Hg, a sign that
is highly suggestive of CoA.
Symptoms
In all mild cases, the symptoms may be absent. However, when present, the symptoms include:
Difficulty in breathing: The heart is unable to pump
the blood completely to the systemic circulation. Pulmonary circulation
is also disturbed resulting in difficult breathing and shortness of
breath.
Episodes of fainting or near fainting: When the blood supply to the brain is reduced, the patient can experience episodes of fainting or near fainting.
Abnormal fatigue, tiredness and muscle weakness: The
heart is unable to properly pump the blood which results in the reduced
oxygenation of body tissues. The reduced oxygenation is the main reason
for the fatigue, tiredness, and weakness experienced by the patient.
Poor appetite or problem feeding: Infants have trouble breathing and have difficulty feeding.
Problems with blood flow: At the narrowing of aorta in CoA, the normal blood flow is disturbed.
Paleness and Cold feet: The heart is pumping against
high pressure, which causes it to pump poorly. Infants appear pale and
may become very fussy or very weak. The symptoms can quickly progress to
shock and require admission to an intensive care unit.
Signs
There are two signs of coarctation of the aorta which should be checked upon physical examination:
Simultaneous high blood pressure (BP) in the arms and low blood pressure in the legs.
The blood pressure is higher in the blood vessels branching out before
the obstruction (in this case, the arms) and lower in the area beyond
the point of obstruction. This difference in blood pressure between the
arms and the legs is referred to as a gradient.
The quality of the pulse in the arms and the legs
will also be different, with a bounding pulse in the upper extremities
and weak or totally absent pulse in the lower extremities.
If both of these signs are identified by the clinician, then the
patient is referred to a cardiologist for their further evaluation.
Diagnostic Workup for Coarctation of the Aorta
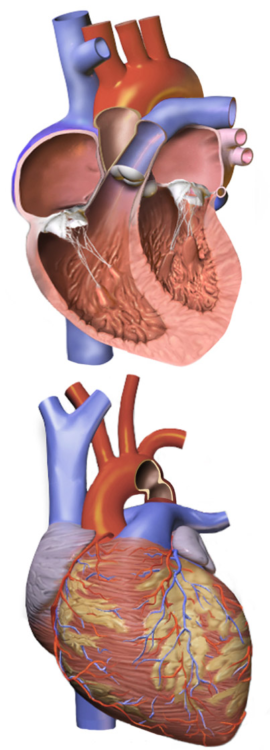
Image: “Illustration demonstrating a narrowing of the large blood vessel (aorta) that leads from the heart.” By BruceBlaus. License: CC BY-SA 4.0
Patients with CoA might present with cardiogenic shock.
In that case, care must be taken to exclude sepsis as the cause of
shock. Blood, urine and cerebrospinal fluid cultures are indicated in
patients presenting with shock.
Patients might have elevated levels of creatinine and blood urea
nitrogen due to impaired kidney perfusion, especially if they are
started on angiotensin converting enzyme inhibitors.
An electrocardiogram might reveal left ventricular hypertrophy.
Patients with early onset of CoA semiology usually exhibit signs
suggestive of congestive heart failure on their chest x-rays, such as:
- Pulmonary edema
- Cardiomegaly
- Increased pulmonary vascular markings
Patients who present late might have cardiomegaly and rib notching due to collateral vessels formation.
Echocardiography is very helpful in the evaluation of congenital
heart diseases. It can help in the exclusion of other preexisting
cardiac abnormalities. Doppler echocardiography is useful in the
measurement of the gradient pressure at the site of coarctation to
determine the degree of obstruction.
Other imaging modalities, such as magnetic resonance imaging and computed tomography scanning of the thoracic and abdominal aorta, are very helpful in identifying the aortic pathology and determining the size and site of coarctation.
In a few patients, cardiac catheterization might be needed to
determine the degree of the aortic obstruction, its exact anatomical
location, and size. Recent imaging modalities such as echocardiography
and MRI have made cardiac catheterization a second-line diagnostic
modality for the evaluation of CoA.
After surgical correction, a biopsy might be examined for
histological characterization of the lesion. When the histological
examination is performed, one might see a thickened medial layer of the
aortic wall that is usually opposite to the insertion of the patent
ductus arteriosus.
Chest x-ray
Imaging allows the resorption of the lower part of the ribs to be
seen. The classic “figure 3 sign” seen on the X-ray results from the
post-stenotic dilation of the aorta.
Echocardiogram
It is the definitive test for coarctation. It can provide images of the heart and aorta and helps in the identification of the exact area of obstruction.
MRI
An MRI (magnetic resonance imaging) is an imaging study which is
performed inside a magnet which allows the observation of very finely
detailed images of the heart, collateral blood vessels and the aorta
Differential Diagnosis of Coarctation of the Aorta
The successful diagnosis of the coarctation of the aorta depends on
the history of the patient, the presentation of the symptoms and
vigilant detection of signs by the clinician.
Further confirmation can be done with the help of lab and imaging investigations.
For the accurate diagnosis of patients with coarctation of the aorta,
the main symptoms and signs, as mentioned above, should be considered.
The other clinical conditions which can confuse the diagnosis of
coarctation of the aorta due to similar presentation are:
Endocardial fibroelastosis
History: Excessive sweating, breathlessness, wheezing, failure to thrive.
Physical Examination: Tachypnea during feeding and grunting
respiration with intercostal retractions. Expiratory wheezes or rales in
the lung bases.
Dilated cardiomyopathy
Symptoms: Dyspnea on exertion, shortness of breath, orthopnea, edema, fatigue
Signs on physical examination: Tachypnea, Tachycardia and hypertension/hypotension.
Pediatric Valvar-Aortic stenosis
Symptoms vary based on the age of presentation and the severity of the obstruction.
Signs on physical examination:
In neonates: reduced/absent pulses, tachycardia, Tachypnea.
In childhood: systolic ejection murmur present at the left middle and right upper sternal border, 4th heart sound present.
Pediatric Viral Myocarditis
Symptoms: Irritability, periodic episodes of pallor, lethargy, fever, anorexia, failure to thrive
Signs on physical examination: Diminished cardiac output,
tachycardia, weak pulse, cool extremities, pale or mottled skin,
Hepatomegaly, rales sound may be heard.
Hypertension
Systolic BP > 140 mmHg and Diastolic BP > 90 mmHg
A complete history and physical examination are necessary to find out the underlying etiology.
Treatment of Coarctation of the Aorta
The choice of treatment depends on a number of factors which include:
- Age of the patient
- Risks and benefits of the procedures
- Anatomy of the aortic obstruction
Surgical Treatment
Surgical repair is the most time-tested and traditional treatment
for most patients with CoA, particularly for infants and younger
children. The surgical procedure is done through an incision on the left
side of the chest cavity, and the heart-lung machine is not required
for it.
The hospital stay usually lasts from four to seven days following the
surgery, with the first few days spent in an intensive care unit to
vigilantly monitor the vitals.
High blood pressure is commonly observed in these patients post
surgery. While in the hospital, it is managed with intravenous (I/V,
into the bloodstream) medicines. After the patient has been checked out,
oral medications are prescribed to be administered at home.
The risks of this surgical procedure are very low, and the observed outcomes are excellent.
Catheterization Treatment
The cardiac catheterization is basically a test performed by using catheters (small tubes) placed into the peripheral (in any arm or leg) blood vessels
and then maneuvered into the larger blood vessels and the heart. In the
past 25 years, a number of such procedures using specialized catheters
have been developed for repairing of the heart.
The coarctation of the aorta can be opened up from the inside using
the balloon dilation method or by placing an internal stent. The
catheterization procedure usually takes several hours and is performed
under anesthesia.
The patients are strictly observed overnight in the hospital and can
otherwise resume their normal activities within a few days of the
procedure. In case stents are placed, aspirin is recommended for a
number of months to prevent the formation of blood clots.
Other precautions to prevent the risk of infection are also needed.
Antibiotics are given before general dental work and some other usual
medical procedures (this is known as bacterial endocarditis
prophylaxis).
Following the successful treatment, the patients with coarctation of the aorta are able to lead a normal lifestyle and most likely have a near-normal lifespan.
However, limited exercise restrictions can be indicated for the
patients with continued aortic obstruction, high blood pressure or
dilation of the aorta. These patients need lifelong regular cardiology
evaluations with imaging of their heart so that they can be monitored
for later problems.
Recoarctation is more prevalent when the repair is done during
infancy. Balloon angioplasty is the usual treatment option for
recoarctation, although repeated surgery can be indicated for some
patients.
Complications of Coarctation of the Aorta
High blood pressure
High blood pressure is usually common in patients with coarctation as they get older,
even after successful repair through either surgery or catheterization,
and they need antihypertensive medications for a long time. This
problem is more likely to occur when the intervention is done in older
children or adults.
High blood pressure can lead to thickening of the heart muscle and can bring about changes in the blood vessels.
The elevated blood pressure increases the risk of stroke, coronary
artery disease, kidney damage and other health problems. It is very
important to maintain normal blood pressure for future health.
Recoarctation
The repaired area of the aorta—either by surgery or
catheterization—may become narrowed again, which is called
recoarctation. With recoarctation, the pre-treatment blood pressure
difference between the arms and legs (major sign for diagnosis of the
coarctation of the aorta) on physical examination returns and further
evidence of aortic obstruction is observed via echocardiogram or MRI.
Aneurysms
Aneurysms—i.e., weakening of the walls of the aorta—can also occur at
the site of the repair after both surgery and catheterization, although
the significance of this is still unclear to the clinicians and
surgeons.
Bicuspid aortic valve stenosis
The bicuspid aortic valve, which is often associated with the
coarctation of the aorta, may develop some sort of narrowing (termed as
stenosis) or leaking (termed as regurgitation) over time and thus
require further treatment.
Comentários
Enviar um comentário