Innate Immune System — Components and Complement System
Table of Contents
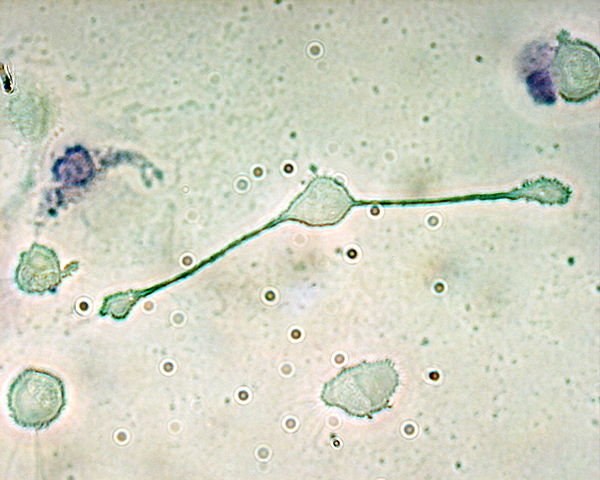
Image: Macrophage. By: The original uploader was Obli at English Wikipedia – Transferred from en.wikipedia to Commons., CC BY-SA 2.0, Link.
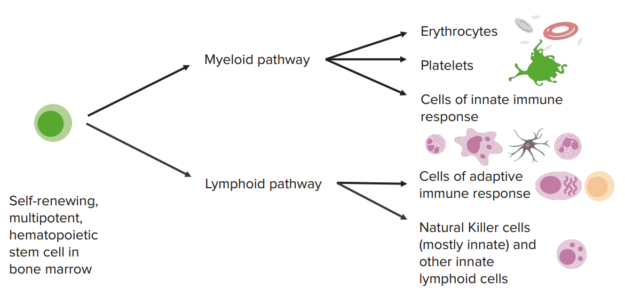
Hematopoeisis
Features and Components
The non-specific immune response has three important features that differentiate it from the specific immune response: it is innate, unspecific against pathogens and it has no immunological memory. Thus, it is also called the innate immunity. The innate immunity is determined by the genome and therefore it cannot adapt to environmental changes. Phylogenetically (in terms of evolution), it is older than the adaptive immune system.
Furthermore, the innate immune system can recognize antigens as a whole, which means that the antigens do not have to be degraded and presented first. The non-specific defense is especially fast and takes place within seconds and minutes after the first contact with an antigen.
On the one hand, the non-specific immune response is made up of numerous cell types with different functions. On the other hand, it consists of different non-cellular (humoral) components, which are messengers that are able to cause local or systemic reactions. These also include the complement system. The complement system is part of the non-specific immune response, but since it can also be activated by components of the specific immune response, it serves as a connection between both systems.
Remember: The non-specific immune response is
- innate (which means it is not acquired)
- unspecific against pathogens
- has no immunological memory
- can recognize antigens as a whole
- takes place very fast (within minutes)
Cellular components
Cells of the non-specific immune system can be found in all body tissues as well as circulating in the blood and lymphatic fluid. This ensures that the cells can react quickly to invading pathogens at any time. Most of these cells take up antigens via phagocytosis, e.g. neutrophil granulocytes. Dendritic cells, monocytes and macrophages belong to the so-called antigen-presenting cells. Those cells can take up antigens, phagocytize them, then present them for other cells and initiate a specific immune response.
On the contrary, eosinophil granulocytes perform exocytosis and release vesicles containing toxic substances and enzymes in their surrounding. Natural killer cells are lymphocytes and kill cells that have been infected with a pathogen or cells that show neoplastic changes by initiating a natural cell death (apoptosis) via cell-surface molecules.
Remember: Cellular components of the non-specific immune system are
- Dendritic cells
- Monocytes and macrophages
- Neutrophil and eosinophil granulocytes
- Natural killer cells
Moreover, all cells that are part of inflammatory processes are part of the non-specific immune response since they produce messenger substances. This includes e.g. endothelial cells, fibroblasts, thrombocytes and keratinocytes.
Phagocytic cells
- Neutrophils are short lived cells that leave blood and enter tissues
- Monocytes leave blood to develop into relatively long lived macrophages
Neutrophils and monocytes bind to the blood vessel endothelium using adhesion molecules and are attracted by a concentration gradient of chemotactic factors.
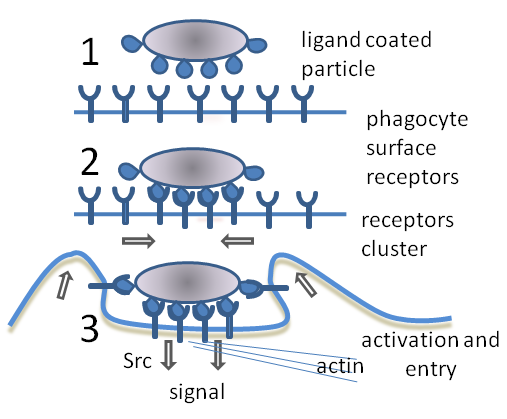
The phagocytic cells use pattern recognition receptors (PRR) to recognize pathogen-associated molecular patterns (PAMPs). The pathogen can also become coated with substances (opsonins) that are additionally recognized by the phagocytic cells.
- complement
- antibody
Once engulfed by the phagocytic cell, the pathogen is destroyed using reactive oxygen intermediates generated by a respiratory burst, and by a number of non-oxygen-dependent killing mechanisms.
Phagocytosis
Image: “Phagocytosis in three steps: Unbound phagocyte surface receptors do not trigger phagocytosis. Binding of receptors causes them to cluster. Phagocytosis is triggered and the particle is taken up by the phagocyte.” by Graham Beards. Licence: CC BY-SA 3.0
Microbicidal activity of phagocytic cells
Dendritic cells
Production of inflammatory mediators
Innate lymphoid cells
One type of ILC, the Natural Killer cell, induces apoptotic cell death in infected cells using:
- Fas/ FasL caspase pathway
- Granzyme/ Perforin pathway
Other types of ILCs have functions similar to the helper T-cells and regulatory T-cells of the adaptive response.
Cells of the adaptive immune response
Humoral and Local Acting Messenger Substances
The non-cellular components of the non-specific immune system include a range of different cytokines. These are proteins that influence growth and differentiation of cells. Cytokines of the non-specific immune system are interleukin 1 (IL-1), interleukin 6 (IL-6) and tumor necrosis factor-α (TNF-α) as well as interferon-α (INF-α).
IL-1, IL-6 and TNF-α activate additional inflammatory cells and serve as means of communication with the specific immune system. As so-called endogenous pyrogens, they also trigger the increase in body temperature. Fever ensures that immune cells can carry out their work in their optimal operating temperature and the immune response becomes efficient. INF-α, which is produced by granulocytes and fibroblasts inhibits the replication of viruses in the host cell and activates natural killer cells.
Another part of the humoral and local acting messenger substances are acute-phase-proteins, which are produced in the liver after stimulation of cytokines. They support the non-specific immune system and surround and confine the center of inflammation.
The blood concentration of acute-phase-proteins increases thousandfold within hours. Examples of acute-phase-proteins are: fibrinogen, procalcitonin and C-reactive protein (CRP). Negative acute-phase-proteins are substances, whose serum levels decreases in case of acute inflammation, e.g. albumin and transferrin. Some of these substances serve as diagnostic inflammation markers, such as CRP.
Last but not least are defensins. These substances are produced by epithelial cells of the skin and mucosa as well as by different immune cells. They react with bacterial components and thus assist in their destruction.
The Complement System
The complement system is a group of plasma proteins, it is involved in the defensive mechanisms against microorganisms and activated on the surface of its plasma proteins. Activation of the complement system triggers an enzyme cascade, which activates further functions of the immune system and boosts the non-specific immune response.
The process of covering the surface of pathogens with complement factors with the aim of making it recognizable for other cells that can eliminate the pathogen is called opsonization.Most of the approx. 30 proteins are produced in the liver.
The complement system can be activated via direct or indirect pathway. Indirect activation is done via components of the antigen’s cell wall. Direct activation serves as a connection to the specific immune response, since it requires the formation of antigen-antibody-complexes.
There is one more activation pathway of the complement system, enabled by the so-called mannose-binding-lectin, which is a substance produced through immune reactions with bacteria and can be found within the plasma.
Joint final pathway of both activation methods is the conversion of complement factor 3 (C3) to C3a and C3b, which in turn cleaves C5 in its active parts and forms a membrane attack complex (MAC) together with the remaining factors. This complex lyses the target cell. For the detailed process see figure.











Comentários
Enviar um comentário