Sarcoidosis — Symptoms, Diagnosis and Treatment
Table of Contents
- Definition of Sarcoidosis
- Epidemiology of Sarcoidosis
- Etiology of Sarcoidosis
- Pathology and Pathophysiology of Sarcoidosis
- Symptoms of Sarcoidosis
- Diagnosis of Sarcoidosis
- Differential Diagnoses of Sarcoidosis
- Therapy of Sarcoidosis
- Progression and Prognosis of Sarcoidosis
- Review Questions
- References
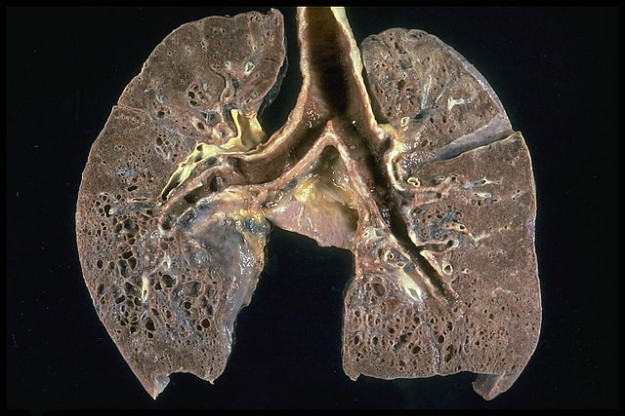
Image: “Sarcoidosis – Honeycombing: Prominent honeycombing is present in the lower lobes accompanied by fibrosis and some honeycombing in the upper lungs. ” by Yale Rosen. Licence: CC BY-SA 2.0
Definition of Sarcoidosis
Sarcoidosis – A Multisystem Disease
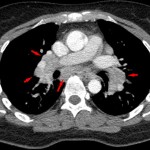
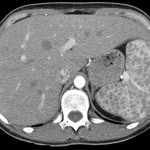
Bild: “CT Scan of Sarcoidosis: Stage II” by Hellerhoff. Licence: CC BY-SA 3.0
Sarcoidosis is a multisystem disease whose genesis is not yet completely known and which is characterized by non-caseating granulomas in the affected organs. The main locations for this disease to manifest itself in are the lungs and the hilar lymph nodes. One differentiates between acute sarcoidosis (this also includes “Löfgren’s syndrome”, a special form of the disease) and chronic sarcoidosis. It is important to understand that acute and chronic sarcoidosis progress differently, usually independent of one another. The chronic form of this disease does not follow the acute form of the disease as it is typical in many other illnesses.
Epidemiology of Sarcoidosis
Sarcoidosis as Interstitial Lung Disease
With incidents of 10/100,000 per year in Western Europe, sarcoidosis is among the most frequent interstitial lung diseases, whereby one has to assume that there is also a high number of individuals who have the disease but are not diagnosed. Sarcoidosis usually peaks between the ages of 20 and 40 and affects women slightly more frequently than men, especially the acute form of the disease.
Etiology of Sarcoidosis
Causes of Sarcoidosis
Image: Crystallographic structure of HLA-DQA1 (cyan) complexed with HLA-DQB1 (green) and HCRT (magenta) based on PDB 1uvq. Licence: Public domain.
The cause of sarcoidosis is not yet known. Various theories, however, describe a multifactor genesis in which both, genetic predisposition as well as certain environmental factors, seem to be relevant. In many cases, family members of an affected patient acquire the disease as well. Furthermore, studies have shown that a mutation of the gene BTNL2, as well as the HLA-DQB1 variant of the gene HLA, are associated with an increased risk for the disease.
The increased occurrence of the disease among hospital nursing staff members, among others, proof of bacterial nucleic acids or inhalation of talc or aluminum gathered from the patient’s medical history, all point to the influence of many environmental factors.
Pathology and Pathophysiology of Sarcoidosis
Sarcoidosis on a Cellular Level
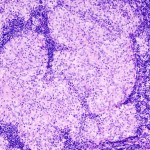
Caused by a disturbance of T cell function and increased B cell activity, immunological hyperactivity occurs. Macrophages accumulate locally and release mediators, which, in turn, cause those macrophages to change into epithelial cells. Some of these epithelial cells merge into giant Langerhans cells. Surrounded by lymphocytes (= lymphocyte accumulation), this is referred to as “granuloma”. The granulomas occurring within the scope of sarcoidosis do not show signs of necrosis in their center, which is why they are referred to as “non-caseating granulomas”. While this may not be as relevant for the exam, one of your patients may want to know about this in more detail: Within the aforementioned giant cells, shell-shaped calcified inclusions can be found here and there, the so-called “Schaumann bodies”. These were named after J. N. Schaumann, who was the first to recognize that sarcoidosis is a systemic disease that can attack several organs and not only the skin, which had been the theory until that time.
Symptoms of Sarcoidosis
General Symptoms of Sarcoidosis
While it would be best to further differentiate between acute and chronic sarcoidosis, there are some general symptoms that many patients with sarcoidosis display:
- Fatigue and exhaustion
- Fever
- Weight loss
- Night sweats
Acute Sarcoidosis
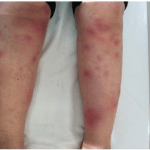
In cases of acute sarcoidosis (10 % of cases), the fever is frequently high. Usually, the skin, lymph nodes, and joints (in cases of polyarthritis) are affected. An acute attack on the lungs manifests itself as dyspnea and cough and even thoracic pain. A special form of the disease is Löfgren’s syndrome. The following triad of symptoms of Löfgren’s syndrom is a popular topic for exams:
- Polyarthritis (it usually affects the ankle joints)
- Bihilar lymphadenopathy
- Erythema nodosum (it especially affects the extensor sides of the lower legs)
Chronic Sarcoidosis and Study Table
Chronic sarcoidosis usually progresses slowly with few symptoms which is why it is usually diagnosed by accident or so late in the progression that there is already structural damage to organs.
The following is an overview of the key locations where the disease manifests itself as well as the symptoms associated with it:
Diagnosis of Sarcoidosis
Diagnosing Sarcoidosis in the Lab
After the clinical findings have been established, the laboratory diagnosis may deliver further indications that may support the suspected diagnosis:
In acute cases of the disease, the inflammatory parameters are usually significantly elevated (especially the erythrocyte sedimentation rate, ESR).
In chronic cases of the disease, approximately half of them have elevated IgG levels. Furthermore, calcium levels in blood or urine may be elevated as the epithelial cells produce vitamin D. In some cases, leukocytopenia (leukopenia) or lymphocytopenia (lymphopenia) may occur. As the activity parameter and to control the progression, either ACE (angiotensin converting enzyme) or the soluble interleukin-2-receptor are frequently used. In cases of high disease activity, both of them are elevated, during remission or with successful therapy, they normalize.
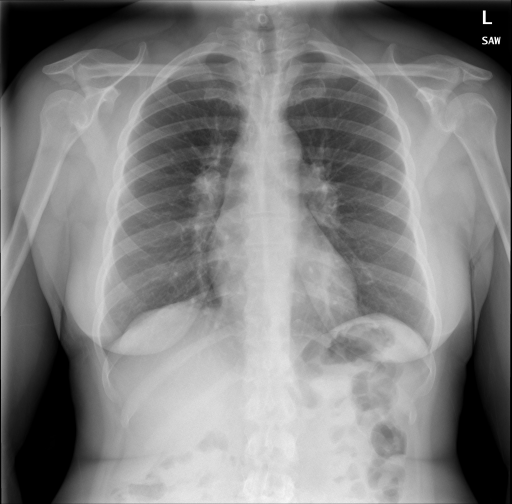
Diagnosing Sarcoidosis via Radiology
The next step should be chest X-rays. According to the results, one can classify chronic sarcoidosis into five different stages according to Scadding:
In cases of unclear or not quite specific radiological findings but with typical clinical signs present, it may be necessary to follow up with an HRCT (high-resolution CT). The HRCT will show changes in pulmonary structure sooner than chest X-rays: Interlobular septal thickening or fine nodular densification are signs of fibrotic changes in pulmonary tissue.
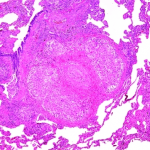
Transbronchial Biopsy and Histology in Cases of Sarcoidosis
The histological examination of affected tissue is another important step in diagnosing sarcoidosis. The results of the biopsy can prove the presence of non-caseating granulomas or histologically rule out other differential diagnoses, respectively. In cases of pulmonary tissue involvement, performing a bronchoscopy along with a transbronchial biopsy and bronchoalveolar lavage (BAL) are appropriate. The latter may reaffirm typical findings: In cases of active sarcoidosis, the CD4/CD8 quotient is > 5 (the higher the quotient, the more probable the diagnosis) and a shift of the T helper/T suppressor ratio in favor of the T helper cells can be seen (caused by the lymphocyte alveolitis).
Sarcoidosis and the Pulmonary Function Test
Pulmonary function may reveal signs of restrictive ventilation disturbance, especially if pulmonary fibrosis has already begun. Reduced O2 diffusion capacity is a very early and sensitive parameter for sarcoidosis activity.
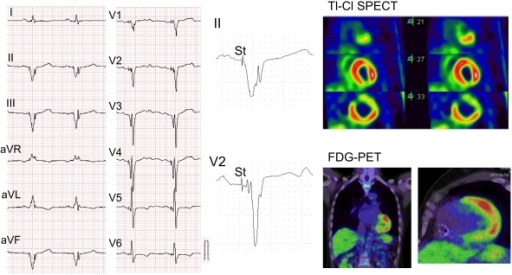
Cardiological Diagnosis of Sarcoidosis
As mentioned above, sarcoidosis may attack many organs and it would, therefore, be prudent to also follow up with cardiac diagnostic tests (ECG, echocardiography) and an ophthalmological examination, possibly even other specialist consultations, should such a suspicion exist.
Assessing Chronic Sarcoidosis Activity
First and foremost, in order to assess the disease activity, especially in cases of chronic sarcoidosis, observing the progression of the clinical signs as well as the laboratory findings is appropriate (ACE, soluble IL2-receptor, inflammatory parameters, calcium). The parameters of the pulmonary function test (the diffusion capacity in particular) are suitable to monitor the progression. Depending on symptoms, the corresponding organ-specific changes must be monitored regularly (i.e. chest X-rays in cases of pulmonary involvement and bihilar lymphadenopathy, an ECG in cases of cardiac arrhythmia, etc.).
Differential Diagnoses of Sarcoidosis
Clinical pictures similar to sarcoidosis
Sarcoidosis can mimic many diseases. Differential diagnoses include, among others:
- Tuberculosis (presents with caseating granulomas, however!)
- Hodgkin’s disease (morbus hodgkin) (This is the reason why a lymph node biopsy followed by histology is so important.)
- Pneumoconioses (Occupational history: branches of the industry that work with beryllium, for instance.)
- Exogenous allergic alveolitis
- In cases of acute sarcoidosis: arthritis of another genesis
Therapy of Sarcoidosis
As acute sarcoidosis as well as chronic sarcoidosis stage I in particular show high spontaneous cure rates, it is routine to first watch and wait while monitoring the patient und forego the side effects of long-term steroid therapy to begin with.
Indications for Corticosteroid Therapy in Cases of Sarcoidosis
- Starting with stage II, with simultaneous restricted pulmonary function
- Hypercalcemia and hyperuricemia (threat of chronic renal insufficiency)
- Involvement of the eyes, liver, CNS, myocardium or skin
- Severe general symptoms, severe arthritis (i.e. Löfgren’s syndrome)
Should the patient not respond to therapy with glucocorticoids after three months, it does not seem promising to continue on with it. In this case, a combination of immunosuppressive drugs (i.e. azathioprine, methotrexate, anti-TNF-alpha) can be tried.
In cases of local symptoms such as uveitis or skin lesions, steroids can be administered locally as well.
Should the patient complain about severe pains (with arthritis, for instance), the additional supportive administration of non-steroidal antirheumatic drugs (NSAR) is appropriate.
In cases of pronounced pulmonary fibrosis, a lung transplant is the last resort.
Progression and Prognosis of Sarcoidosis
Remission and Spontaneous Cure Rates with Sarcoidosis
Acute sarcoidosis has a remission rate of > 95 % within two years. Chronic sarcoidosis stage I also has a spontaneous cure rate of up to 70 % within one to three years. With regard to stage II, the cure rate is only approximately 50 % and with regard to stage III, the rate drops all the way to 20 %.
The risk factors for a more progressive and chronic progression are patients over the age of 40 when first diagnosed, hypercalcemia, lupus pernio, uveitis, neurosarcoidosis, cardiac involvement, pulmonary sarcoidosis stage III.
The mortality rate for sarcoidosis is at less than 5 %.
Review Questions
The answers are below the references.
1. In which of the following syndromes do cystic changes in the phalanges take place within the scope of a chronic form of extrapulmonary sarcoidosis?
- Löfgren’s syndrome
- Heerfordt’s syndrome
- Jüngling syndrome
- Raynaud’s syndrome
2. What findings match the clinical picture of sarcoidosis the least?
- Increased erythrocyte sedimentation rate (ESR).
- A lower CD4/CD8 quotient in the cytological examination after bronchoalveolar lavage.
- Hypercalciuria
- Lymphopenia
3. Which diagnostic tool is most likely to be used to monitor the progression of chronic sarcoidosis?
- Pulmonary function test and determining diffusion capacity.
- Thoracic high-resolution CT.
- Regular bronchoscopies and transbronchial biopsy.
- Assessment of peripheral oxygen saturation.



Comentários
Enviar um comentário