Vaginal Diseases and Vulvular Disorders: Bacterial Vaginosis, Vulvitis and more
Table of Contents
Image: “at obstetrics and gynecology” by seapachi. Licence: CC BY-SA 2.0
Colpitis
Colpitis (or vaginitis) refers to the inflammation of the vagina. The pathological vaginal discharge and epithelial reddening are typical symptoms.
The pH-value of the vaginal milieu is normally acidic. It is between 3.8 and 4.5. This way, an excessive proliferation of pathogenic germs is inhibited. Lactic acid bacteria are responsible for this milieu. They are called Döderlein’s bacteria and produce lactic acid based on estrogen.
Accordingly, the vaginal flora is disturbed if, for instance, lactic acid bacteria are inhibited. Cervical mucous and menstrual blood can lead to alkalization. Other irritations can be caused by lack of estrogen, diabetes mellitus, foreign bodies (e.g. tampons), vaginal douches, sexual contacts, or antibiotics.
Pathogens of Colpitis
An inflammation of the vagina can have several reasons. The most frequent causes are:
- Bacterial infections (bacterial vaginosis)
- Fungal infections with candida (vaginal thrush)
- Trichomoniasis
Bacterial Vaginosis
One major form of colpitis is bacterial vaginosis, which is—as the name suggests—a vaginosis caused by bacteria.
Pathogens of Bacterial Vaginosis
In the vaginal secretion of symptom-free, sexually active women, Gardnerella vaginalis can be found. It is assumed that the transmission occurs via vaginal intercourse. Additionally, bacteria from the perianal region and bacteria of sexual partners can change the vaginal flora. This can promote the proliferation of anaerobes like Gardnerella vaginalis. They then replace the lactic acid bacteria.
Clinical Presentation of Bacterial Vaginosis
Usually in this inflammation, neither reddening nor itching is present. Specific findings are the grey-white, very thin, sometimes foamy vaginal discharge and its fishy smell in the alkaline area. As a complication, an ascending infection can develop.
Diagnostics of Bacterial Vaginosis
Treatment of Bacterial Vaginosis
Once diagnostics are completed, treatment should be commenced. Administration of 5-nitroimidazole (metronidazole 2 x 400 mg for 5 days) is the established treatment. The healing rate is roughly 95%. Simultaneous treatment of sexual partners is not recommended.
Vaginal Thrush
Vaginal thrush refers to a fungal infection that leads to colpitis. In over 80% of the cases, theses fungal infections are caused by Candida albicans. In rare cases, they are caused by Candida glabrata. Frequently, candida are already colonizing vulva and vagina.
Therefore, vaginal thrush normally is an endogenous infection. If the vaginal flora is disturbed, the proliferation of germs is promoted. Hormonal fluctuation (e.g., pregnancy or oral contraceptives), antibiotic therapy, or immunodeficiency can also promote an infection.
Clinical Presentation of Vaginal Thrush
Itching, burning, pain, and discharge are typical symptoms of vaginal thrush. Vaginal thrush normally occurs together with vulvitis.
Diagnostics of Vaginal Thrush
Treatment of Vaginal Thrush
A first step is the local treatment with nystatin- and imidazole medication in the vagina and on the vulva; 5 – 7 days can be sufficient.
If the vaginal thrush is recurrent, systemic therapy with fluconazole becomes necessary. Treatment of the partner is not necessary since it is an endogenous infection. However, the rate for recurrences is quite high.
In case of a chronic recurrent vaginal thrush, high-dosage administration with fluconazole for several weeks is recommended. Also, regularly performed prophylactic antimycotic treatment can be reasonable.
Trichomoniasis
Bild: “Micrograph showing Trichomoniasis” von NEphron. Lizenz: CC BY-SA 3.0
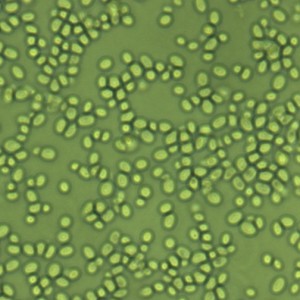
Trichomoniasis is caused by Trichomonas vaginalis. It is a facultative pathogenic protozoon. It affects the vagina, glandular ducts, urethra, and less frequently also the bladder, rectum, and cervix.
Transmission occurs via sexual contacts. Risk for infections amounts to 70%. In the last years, the number of infections has severely regressed and is now below 1%.
Clinical Presentation of Trichomoniasis
A characteristic sign of trichomoniasis is a severe, liquid, foamy discharge, which sometimes is green-yellow. Also, symptoms like burning, itching, and sometimes dysuria and reddening can be observed.
A potential complication of trichomoniasis is an accompanying bacterial vaginosis.
Diagnostics of Trichomoniasis
Treatment of Trichomoniasis
Systemic administration of 5-nitroimidazoles (1×2 g metronidazole) has a healing rate of 90%. Treatment of the partner is necessary. Condoms can prevent transmission.
Unspecific Colpitis
Unspecific colpitis cannot be traced to one particular pathogen.
Vulvitis
Vulvitis is defined as dermatitis of the labia of women. In almost all cases, it is accompanied by a form of vaginitis.
Etiology of Vulvitis
Primary causes of the disease can be fungi, bacteria, or viruses. Secondarily, an inflammation of the outer genitals can also be caused by mechanical causes or by hormonal changes.
Pathogens of Vulvitis
With 95% of the cases, the fungus Candida albicans is the most frequent pathogen of vulvitis. Bacteria like A-streptococci, Staphylococcus aureus, and Treponema pallidum are the second most frequent cause. Viruses like herpes simplex and varicella zoster as triggers are rather rare.
Secondary causes can be mechanical; for example, maceration, which is a consequence of obesity. An inflammation of the outer genital can also be caused by chemical irritation of the skin due to vaginal douches or detergents. Vulvitis can also be a secondary consequence ofpregnancy and of estrogen deficiency during post-menopause. In patients with diabetes mellitus, infections with Candida albicans are frequent.
Clinical Presentation of Vulvitis
There are three main symptoms that should be known. They are the most prominent manifestations of inflammations of the outer genitalia:
- Vaginal discharge
- Pruritus: The scratching caused by the strong itching often worsens the infections. If children present with this kind of itching, worms should be considered as a differential diagnosis.
- Burning and pain during walking, urination, and cohabitation.
Examination shows the typical signs of inflammation; reddened and swollen skin is visible. Candidosis is often accompanied by clumpy white discharge. The native specimen and Sabourand agar show evidence of the fungal infection. In herpes genitalis infections, fine vesicles can be seen. If an inflammation of the hair follicle is present (i.e., folliculitis), one often observes a small red area that is painful and sensitive to pressure.
Treatment of Vulvitis
Against fungal infections, clotrimazole, which is an antimycotic, is applied locally. Bacterial vulvitis can be treated locally with antiseptical povidone iodine and orally with cephalosporin. If a S. aureus infection is left untreated, folliculitis can develop into an abscess. This must be opened surgically. For relief of pain and itching, the patients can apply cortison balm and chamomile hip baths.
Bartholinitis
Bartholin glands are located on the inside of the inner labia. Their excretory duct lies in the introitus area. Bartholinitis is an inflammation of the Bartholin gland that leads to painful swelling. In most cases, it is unilateral. If the excretory ducts are obstructed due to a stasis of the glandular secretion (Bartholin cyst), an infection with intestinal germs can occur.
Etiology of Bartholinitis
- Neisseria gonorrhea
- Staphylococcus aureus
- Escherichia coli
- Anaerobe bacteria (bacteroides, peptococci, peptostreptococci)
Clinical Presentation of Bartholinitis
If the secretory ducts are obstructed, swelling occurs, which can reach the size of a ping-pong ball. This cyst is painful when infected and can even lead to problems walking.
Treatment of Bartholinitis
In case of a large cyst or an abscess, treatment consists in marsupialization, which is performed under general anesthesia. If the bartholinitis is recurrent, extirpation of the Bartholin gland can be performed.
Condylomata Acuminata
Condylomata accuminata are papillary, pointy epitheliomas, which mainly affect the vulva, vagina, porta uteri, and the anal region.
Etiology of Condylomata Acuminata
An infection with HPV (human papilloma virus) can trigger the formation of condylomata acuminata. Serotypes 6 and 11 are responsible for changes like pointy condylomas. Infection with papilloma viruses HPV-16 and -18 can lead to the formation of cervical or anal carcinoma.
Clinical Presentation of Condylomata Acuminata
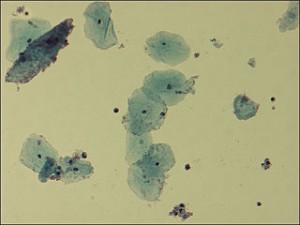
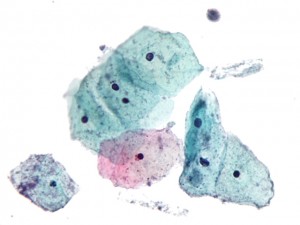
Examination shows pointy, papillary changes of epithelial cells. They are arranged in a cockscomb-like manner.
Histology shows koilocytes. These are squamous epithelial cells with a perinuclear halo, which means that these cells have a bright halo around their nucleus. Koilocytes are a sign of HPV infection.
Treatment of Condylomata Acuminata
Treatment options depend on the severity of the disease. A first step is topical treatment. In cases of mild infestation, denaturation using podophyllin cream or 60% tricholoric acetic acid is possible. For extreme infestations, surgical treatment using electric sling abrasion or a CO2laser has to be performed.
Lichen Sclerosus: Vulvar Itching
Lichen sclerosus is a chronic disease and a degenerative change of the dermis. It consists in a shrinking of the vulva and sclerotization of subcutaneous fat tissue.
Etiology of Lichen Slerosus
Lichen sclerosus is caused by skin shrinking due to a lack of estrogen.Older women often suffer from estrogen deficiency in post-menopause.
Clinical Presentation of Lichen Sclerosus
Due to the unbearable pruritus, scratch defects sometimes occur. Examination shows depigmentation, scratch defects, and superinfection. The shrinking is accompanied by shiny vulvar skin.
Diagnostics of Lichen Sclerosus
Histological examination involving punch biopsy or excision should be performed in order to exclude vulvar carcinoma and vulvar intra-epithelial dysplasia.
Treatment of Lichen Sclerosus
Lichen sclerosus is treated with cortison creams for at least 4 weeks exceeding the point at which the patient is free of complaints. Fatty ointments should be applied before any event of skin stress (urination, defecation, cohabitation). Treatment with corticoids is supposed to prevent skin shrinking and synechia (adhesion of the labia).
As long as there is no contraindication, systemic administration of estrogen should be considered. In any case, however, local estrogen treatment should occur. When symptoms persist, laser therapy or surgical interventions like denervation can be necessary.
Popular Exam Questions on Diseases of the Vagina and the Vulva
Solutions can be found below the references.
1. Which is the most frequent pathogen of bacterial vaginosis?
- Gardnerella vaginalis
- Trichomonas vaginalis
- Neisseria gonorrhoeae
- Staphylococcus aureus
- Herpes genitalis
2. Which is the standard treatment of an infection with Gardnerella vaginalis?
- Chamomile hip bath
- Metronidazole for 5 days
- Fluconazole
- Metronidazole for at least 1 month
- Ascorbic acid
3. Which prophylactic measures can be taken to possibly prevent recurrent bacterial vaginosis?
- Prophylactic metronidazole therapy
- Treatment of the partner is necessary
- Administration of lactic acid bacteria
- Fluconazole
- Regular prophylactic antimycotic treatment
4. Which is the most frequent pathogen of vulvitis?
- Herpes zoster
- Staphylococcus aureus
- Candida albicans
- Bacteria
- Trepomona pallidum
5. Which cells are the typical sign of the histology of a HPV infection?
- Keratinocytes
- Koilocytes
- Melanocytes
- Fibroblasts
- Macrophages
6. What is the minimum duration of treatment when using corticoid creams against Lichen sclerosus?
- Up to 2 weeks after the point at which the patient is symptom-free
- 8 weeks are sufficient
- 4 weeks
- 4 weeks after the point at which the patient is symptom-free of complaints
- 1 week





Comentários
Enviar um comentário