Allergies (Allergic Diseases) and Atopy (Atopic Syndrome) — Pathophysiology and Most Common Diseases
Table of Contents
What is an Allergic Disease?
The term allergy refers to a specific excessive immune reaction to exogenous substances known as allergens. After contact with the allergens the immune system is sensitized (which cannot be clinically verified), allergen-specific lymphocytes and antibodies are formed. If the body comes into contact with the same allergen again, the already formed antibodies cause an allergic reaction in the organism.
The symptoms are diverse and can range from a mild skin irritation to an anaphylactic shock. The latter is an emergency that has to be treated immediately.
The term atopy is directly related to allergic diseases. It refers to the hereditary tendency to develop a certain type of allergic reaction (type I reaction). Sub-classes of atopy are diseases like atopic eczema (neurodermatitis), allergic rhinitis, and allergic bronchial asthma.
Atopic allergy — worldwide prevalence
Pathophysiology of Allergic Reactions
In order to organize the variety of allergic reactions, they are classified into four reaction types. The maximal hypersensitivity reaction of the respective type correlates with its own immune response, with one exception.
Immediate Reaction (Type I)
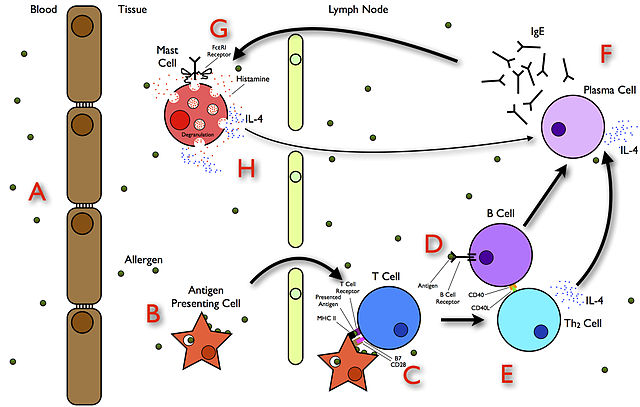
Image: “The Allergy Pathway” by SariSabban. License: CC BY-SA 3.0
In the immediate reaction, the immune response is mediated by IgE-antibodies. It reaches its maximum in a time frame of 30 minutes, or 4–6 hours. Typical allergen sources include foods, insecticides, house dust mite, pollen, animal hair, etc. The immediate hyperergic reaction of the immune system is based on the release of immediate mediators like histamine or Tumor necrosis factor (TNF), the formation of prostaglandins, and the synthesis of pro-allergic cytokines (Grevers; Röcken 2008, p. 28).
The release of these bioactive mediators can lead to local or systemic anaphylaxis; the latter can lead to circulatory collapse, shock, and sometimes death. A classification into four stages (see below anaphylaxis) is used in order to clinically assess the degree of an anaphylactic reaction.
Cytotoxic Reaction (Type II)
The cytotoxic reaction is a reaction of IgG-antibodies. They react to allergens located on the surface of a cell. By binding the antigen on the cell, the antibody either initiates the complement cascade or it activates killer cells. Both cases result in cytolysis.
The maximum of the type II reaction can be expected after 2 days. Clinical examples are the different forms of hemolytic anemia, thrombocytopenic purpura, tumor defense, and also transplant rejection. Although the type II reaction resembles an autoimmune reaction with respect to its progression, it is classified as an allergic reaction because the antigens expressed by the cell enter the body from the outside.
The antigens are typically medication like metabolites of penicillin, but also bacterial and viral antigens (Gravers; Röcken 2008, p. 32).
Immune Complex Reaction (Type III)
As with the cytotoxic reaction (type II), IgG-antibodies are also the cause of the immune complex reaction. However, in the case of type III reaction, they are directed against soluble antigens such as injected serum or infusions, liberated components of bacterial or viral pathogens, or inhaled components of mold fungus or house dust. Eventually, an immune complex made out of antigen and antibody forms. The immunological result is complement binding and the granulocytes and monocytes are activated.
Typical pathological manifestations of the type III reaction are – among others – vasculitis,serum disease, and glomerulonephritis. The maximum of this hypersensitivity reaction occurs 6–8 hours after allergen contact.
Delayed Reaction (Type IV)
Type IV is a delayed immune reaction in which T-lymphocytes are activated after antigen presentation, which, in turn, leads to the release of specific cytokines. In the course of this process, inflammations are mediated which are clinically manifested as, e.g., allergic contact dermatitis or drug-induced exanthem.
Typical triggers of the delayed reaction are metal ions, perfumes, preservatives, mycobacterium, bacteria, and yeast. The maximum of the reaction can be expected in a time frame of 48 and 72 hours.
Note:
What is an Allergen?
An allergen is an antigen that causes a hyperergic immune response. Numerous allergens are polypeptides or proteins, with fungi, pollen, and mites being among the most differentiated allergen sources (Holgate 1996, p. 1). However, many allergens are so-called haptens, which are small molecules that also trigger an immune reaction by binding to high-molecular structures.
Once the immune system is sensitized, it usually does not react to only one single allergen of a given allergen source. Moreover, not all persons react to the same allergens. Thus, allergens which frequently cause an immune response are called a major allergen, and those that rarely is an allergen source are called minor allergens.
Allergen properties influencing allergenicity, given that there is a genetic predisposition, are:
- Differentiated molecular structure
- Ability of the allergen to pass physical barriers
- Foreignness
- Stability
- Biochemical properties
- Solubility
- Concentration
Typical allergen sources are:
- Pollen allergens
- Fungus allergens
- Animal allergens
- Arthropod allergens (insect allergen, arachnoid allergen)
- Food allergens
- Medicinal allergens
Allergy Diagnostics
For allergy diagnostics, there are different tests available, which differ in method and in objective.
In Vivo Testing (Skin Tests)
A number of tests are skin tests. Some of these in vivo methods are:
- Rubbing test
- Skin prick test
- Scratch test
- Intradermal test
- Tuberculin test
In the following, two standard tests – the skin prick test and the patch test – are presented in detail concerning indication, administration, and conclusions.
Skin Prick Test
Image: “Pricktest” by Wolfgang Ihloff. License: CC BY-SA 4.0
The skin prick test is the most important method to test for immediate type allergies (type I). After a droplet of standardized allergen solution is placed on the surface of the inside of the forearm, the skin is then pricked with a thin needle called lancetwithout causing any bleeding.
If an immediate allergic reaction against one of the applied test allergens occurs, erythema and hives begin to form. The time frame for observation is between 20 minutes and 24 hours.
Patch Test
Patch testing is used to test for allergic contact dermatitis, which means that it excludes or identifies an allergic reaction of type IV (delayed type).
Administration
Suspected test substances are attached in small aluminum chambers to the back of the patient using small patches and left in place for 48 hours. After this, patches are removed and an immediate reading of the reactions is taken (day 2), as well as further readings on day 3, day 4, and sometimes also on day 7.
Image: “Patchtest” by Jan Polak. License: CC BY-SA 3.0
In order to avoid the corruption of the test and other irritations as much as possible, the patient is asked to keep his back free of water and soap for the duration of the test. The interpretation of the results is based on a scale of 0 (negative) to ++++ (erythema, blisters, erosion). A reaction exceeding ++++ is referred to as IR (irritant reaction, clearly delineated redness, decrescendo).
In Europe, there is a standard series of patch tests which includes frequent contact allergens like metals, excipients in rubber production, odorous and aromatic substances, and preservatives.
In Vitro Testing
In vitro tests are ancillary methods and can replace in vivo tests if these are contraindicated (e.g. in case of a risk of imminent anaphylactic shock). In vitro procedures use body secretions like blood or nasal secretion to determine the amount of produced antibodies or another immunological substance (allergy screening).
Disadvantage of in vitro tests
The tests do not provide evidence about the actual intensity of the allergic reaction in the patient. In vitro tests examine and determine the following (among other things):
- IgE: determination of overall IgE or specific IgE and IgE in umbilical cord blood
- ECP: eosinophil cationic protein; an indicator for the activation of eosinophils
- CAST: cellular allergen stimulation test for determining leukotriene concentration
- Tryptase: provides information about mast cell activity
- BDT: basophil degranulation test; determination of histamine concentration in isolated basophils
- CIE and CRIE: crossed immunoelectrophoresis or crossed radioimmunoelectrophoresis
Besides the in vivo and in-vitro procedures already mentioned above, there are more tests that can confirm or lead to a suspected diagnosis. The most important include:
- Different bronchial provocation procedures
- Subcutaneous provocation tests
- Provocation tests of the gastrointestinal tract
- Warmth, cold, pressure, and perspiration tests
Important Allergic Diseases
Due to the systemic immunological hyperresponsiveness, allergic diseases have a variety of appearances, which are classified in accordance with their site of manifestation (predilection sites). Here is a list of important allergic diseases; of these anaphylaxis and contact dermatitis will be explained in more detail.
Allergic Emergencies
- Insect sting allergy
- Iatrogenic allergen exposure
- Anaphylaxis
Allergic Skin Diseases
- Image: “Neurodermitis” by Eisfelder. License: CC BY-SA 3.0Atopic dermatitis (neurodermatitis)
- Allergic contact dermatitis
- Urticaria (hives)
- Quincke’s edema
- Vasculitis
- Drug-induced exanthema
- Eosinophilia diseases
- Mastocytosis
Allergic Diseases in the ENT Area
- Allergic rhinitis
- Nasal polyps (polyposis nasi)
- Oral allergy syndrome
Allergic Diseases of the Eye
- Allergic rhinoconjunctivitis
- Atopic keratoconjunctivitis
- Eyelid edema
- Eyelid eczema
- Blepharitis
Allergies of the Lower Respiratory Tract
- Allergic bronchial asthma
- Churg-Strauss syndrome
- Allergic bronchopulmonary aspergillosis (ABPA)
- Exogenous allergic alveolitis
Allergic Diseases of the Gastrointestinal Tract
- Food allergies and food intolerance
- Celiac disease
- Histamine intolerance
- ASS intolerance
Anaphylaxis: Allergic Emergency
Definition
In contrast to an anaphylactoid reaction, anaphylaxis in the narrower sense is a reaction caused by a type I allergy. Since it happens very quick, unexpected, and can have a dramatic development, it represents a potential emergency and is to be treated accordingly.
Pathophysiology of Anaphylaxis
The most frequent pathomechanism of anaphylaxis is the IgE-mediated hypersensitivity reaction of the immediate type. Triggering allergens comprise a broad spectrum and range from antibiotics (especially penicillin), vaccines, local anesthetics to foreign proteins (antiserum, antitoxins) and certain foods (leguminous vegetable, crustaceans, milk, milk products etc.).
Specifically, the pathomechanism of anaphylaxis follows the pattern of the type I reaction: After successful sensitization against the specific antigen, a renewed exposure to the antigen causes the massive release of biochemical mediators from mast cells and basophils. The results are spasms of smooth muscles, increased mucus secretion, and the activation of inflammatory cells.
Mast cell mediators
Beside the scientifically proven anaphylaxis of type I reactions, there are other models for the explanation of anaphylactic reactions which shall be briefly mentioned here: the immune complex /complement-mediated anaphylaxis, anaphylaxis induced by physical stimuli, and anaphylaxis due to apparent abnormalities of the arachidonic acid metabolism (aspirin intolerance).
Symptoms and Progression
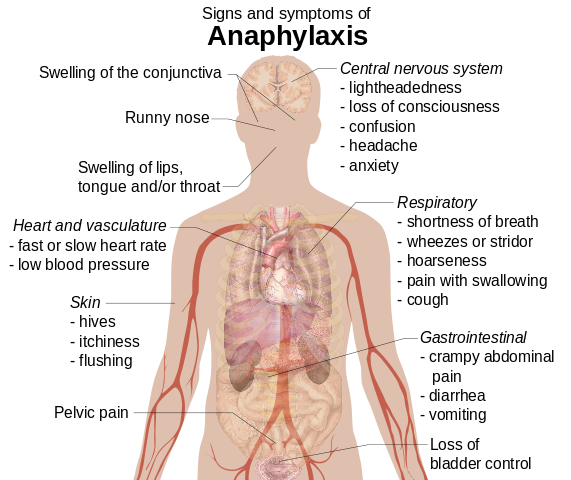
Usually, anaphylaxis occurs unexpectedly. Symptoms differ with regard to severity. Additionally, every case of anaphylaxis affects different organs.
One of the first signs of an imminent anaphylactic reaction is a sensation of warmth or tingling of the skin (often at the ball of the hands and/or the soles of the feet), and sensation of fear. In the further progression, obstruction of the airways with dysphonia, hoarseness, and sensation of suffocation can occur. If not treated, it can result in bronchospasms with imminent respiratory arrest.
In the ENT area, there are typical symptoms are like a dry cough, increased lacrimation, itching of the palate, and further rhinitis and conjunctivitis symptoms. Skin reactions ranging from itching to formation of angioedema (Quincke’s edema). Next to this, complaints in the gastrointestinal tract like nausea, vomiting, and diarrhea are also possible.
The most dangerous form of an anaphylactic reaction is the anaphylactic shock since it can quickly lead to death due to the insufficient blood supply to vital organs.
For the exact assessment of the respective symptomatic presentation, the division of anaphylaxis into five stages (stage 0—4) has proven to be helpful:
Stage classification of anaphylactic reactions (by Müller-Werdan)
Acute Treatment of Anaphylactic Shock
Due to the possibly severe progression of anaphylactic reactions resulting in a manifested shock, immediate action is vital. After termination or elimination of the allergen exposure, alarge-volume venous line, if possible, has to be established for volume substitution with 0.9 % NaCl solution. Simultaneously, 0.3 mg of adrenaline should be given subcutaneously or intramuscular in order to treat severe allergic reactions.
Additional emergency measures are, sufficient supply of oxygen (5 – 10 l/min) and hypovolemic shock positioning. For suppression of the histamine-mediated reactions, antihistamines, glucocorticoids, and beta-2-sympathomimetics are the medication of choice. In case of circulatory or respiratory arrest, the ABCD-scheme is to be followed:
A = airway management
B = (ensure) breathing
C = circulation: chest compression, defibrillation
D = drugs
Allergic Contact Eczema
Definition and Epidemiology
Allergic contact eczema is a T-cell-mediated type IV reaction. In contrast to type I reactions in which the patient reacts to a number of environmental allergens, contact allergy usually is mono- or oligovalent. Approximately 5 – 15 % of all patients who consult a dermatological clinic suffer from a type of contact allergy (Heppt, Renz, Röcken 1998, p. 192).
Etiology and Pathogenesis
Roughly 3,000 different substances can act as triggering allergens for contact dermatitis. Usually, they are so small in molecular structure that they trigger the allergy by binding to high-molecular substances. These small molecules are called haptens.
Contact allergens can be found in plants, clothes, jewelry, cosmetics, and local therapeutics. Some allergens can also be found in aerosols and are therefore very volatile (airborne contact dermatitis). Other allergens, however, only turn into a hapten by being exposed to UV light. In the chronified stage, the smallest amount of daylight is enough to cause an eczema exacerbation (photo contact dermatitis).
Contact allergies primarily develop on the basis of a toxic or chronic eczema (Heppt 1998, p. 196). It is therefore not surprising that contact eczema is especially common for certain occupations, like craftsmen and construction workers (exposed to dichromate) or medical staff (exposed to disinfectant, latex).
Symptomatology
Clinically and morphologically, the allergic contact eczema is divided into acute dermatitis and chronic eczema. However, in clinical practice, both forms cannot always be strictly separated since they often transition into each other.
Although allergic contact dermatitis can generally occur in any part of the body including the mucosa, the hands represent the most frequent location due to the occupational context.
Diagnostic
Often, the suspicion of a contact allergy can already arise during anamnesis and thorough examinations of eczema. Here, special attention should be placed on location and morphologyof eczema. A reliable diagnosis, however, can only be obtained with a patch test (see above).
Treatment
The prioritized therapy of the allergic contact eczema is the absolute avoidance of the hapten. Of course, the prerequisite for this is the identification of the allergen. Since the range of potential triggering allergens is enormous and identification of the causative substance can take a long time, treatment requires good medical knowledge and a lot of empathy for the patient.
Therapeutically, an internal steroid therapy is in most cases not recommended since efficacy is low and the side effects are excessively high. Therefore, treatments mostly rely on externally applied medication. Attention should be paid to the substances contained in the medication; in case of existing sensitization against one of the contained substances, this medication should not be given in order to minimize the risk for further sensitization.
Prognosis: Development and Prophylaxis
The prognosis strongly depends on the dissemination of the respective allergen. Widely spread environmental allergens that cannot be eliminated by the patient or the physician, usually lead to continuous symptoms with partially severe socioeconomic consequences for the affected person.
When there is evidence for a cumulative toxic eczema, the physician should try through continuous symptomatic therapy and patient education to avoid possible further sensitization against this allergen.





Comentários
Enviar um comentário