Anatomy and Diseases of the Vertebral Artery
Table of Contents
- Course of the Vertebral Artery
- Branches of the Vertebral Artery
- Segments of the Vertebral Artery
- Relations of the Vertebral Artery
- Vertebrobasilar Occlusion and Vertebral Artery Syndrome
- Pathophysiology of Vertebrobasilar Occlusion
- Epidemiology of Vertebral Artery Syndrome
- Clinical Approach to the diagnosis of Vertebral Artery Syndrome
- Management of Vertebral Artery Syndrome
- References
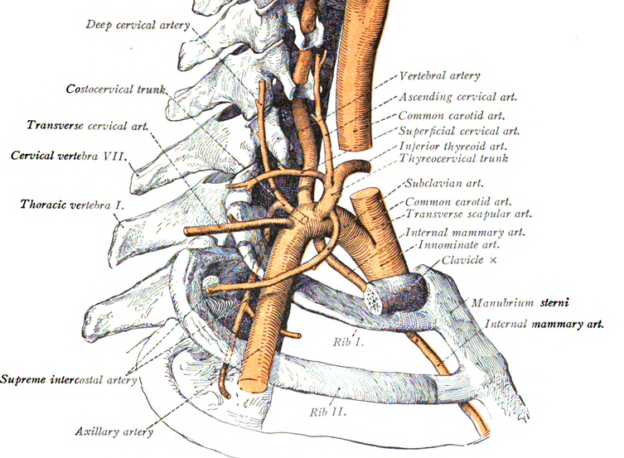
Image: “The branches of the subclavian artery and the course of the vertebral artery in the neck (schematic).” by DR. Johannes Sobotta (Life time: 1945) – Original publication: Atlas and Text-book of Human Anatomy Volume III Vascular System, Lymphati system, Nervous system and Sense Organs Immediate source: http://babel.hathitrust.org/cgi/pt?id=ien.35558004773517;view=1up;seq=5. License: Public Domain/a>
Course of the Vertebral Artery
This artery moves upwards and backward just posterior to the internal carotid artery passing through the transverse foramina of the C6 cervical vertebrae. In some people, the vertebral artery can also originate from the brachiocephalic artery or arch of the aorta.
When the vertebral artery originates from the aorta, it passes a little higher into the foramen transversarium at the level of C5. There may be normal variations in the usual course of the vertebral artery. In 90 % of the cases, the vertebral artery enters the transverse foramen of 6th cervical vertebra; it enters at the level of C5 in 5 % of cases. In about 2 % of cases, the vertebral will enter at C4 and C7 and in approximately 1 % of cases the vertebral artery will enter the transverse foramen at the C3 vertebra.
Branches of the Vertebral Artery
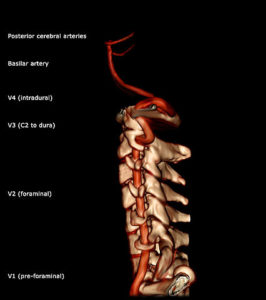
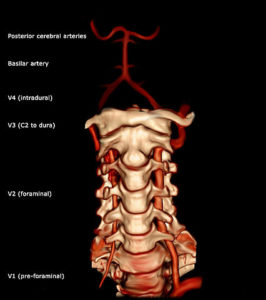
Image: “Vertebral Artery segments – lateral projection.” by Frank Gaillard – Own work. License: CC BY-SA 3.0
The vertebral artery gives off many small branches including spinal branches that supply the spinal cord in the cervical region. The largest branch of the vertebral artery supplies the cerebellum and is known as the posterior inferior cerebellar artery (PICA). The vertebral artery terminates by joining with the vertebral artery from the other side, and together the two vertebral arteries form the single basilar artery.
Segments of the Vertebral Artery
The vertebral artery is typically divided into 4 segments:
First segment (V1) – Pre-foraminal segment: this first segment extends from the origin of the artery to the transverse foramen of C6
Second segment (V2) – Foraminal segment: this second segment extends from the transverse foramen of C6 to the transverse foramen of C2 from where it exits.
Third segment (V3) – Atlantic or extradural segment: extends from the transverse foramina of C2 to the entry into the foramen magnum (into the skull, i.e., becomes intracranial but extradural), after crossing the dura mater.
Fourth segment (V4) – Intra-dural segment: extends from the dura to the confluence with the other vertebral artery, to form the basilar artery (intracranial, intradural)
Relations of the Vertebral Artery
Anterior relations of the Vertebral Artery
Image: “Vertebral artery based on 3d surface rendered CTA.” by Frank Gaillard – Own work. License: CC BY-SA 3.0
Anteriorly, the vertebral artery is related to the common carotid artery, vertebral vein, thoracic duct othe n left side and right lymphatic duct on the right side.
Posterior relations of the Vertebral Artery
The posterior relations of the vertebral artery include the ventral rami of C7 and C8, the transverse process of C7 and the inferior cervical ganglion.
Anteromedial relations of the Vertebral Artery
The anteromedial relations of the vertebral artery include the inferior thyroid artery and middle cervical ganglion.
The second segment of the artery remains in the transverse foramina. The third segment starts from C2 (also known as the axis) and moves in a lateral direction through C1 (also known as the atlas). As this segment moves through the cervical region, it enters into the skull by piercing the dura and arachnoid and continuing as the fourth segment of the vertebral artery.
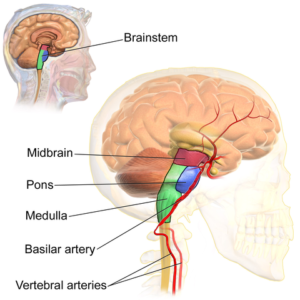
The fourth segment joins the contra-lateral vertebral artery from the opposite side at the lower border of the pons and continues as the basilar artery.
Vertebrobasilar Occlusion and Vertebral Artery Syndrome
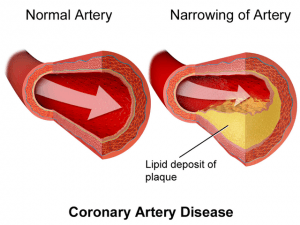
The vertebral artery is an important component of the blood supply to the brain. If there is an impairment to blood flow through the vertebral artery (or arteries), this may lead to stroke which can further lead to paralysis and even death. Causes of vertebrobasilar occlusion include atherosclerosis of the blood vessel as well as vertebral artery dissection.
Pathophysiology of Vertebrobasilar Occlusion
- Atherosclerosis is a very common disease of the vertebral artery leading to narrowing and occlusion of the lumen of the vertebral artery. Stenosis of both the arteries may lead to vertebrobasilar ischemia. Development of collateral circulation is very effective even in the event of occlusion of the vertebral artery. Vertebral artery stenosis due to atherosclerosis may lead to cerebral ischemia, in the posterior circulation, also known as the hindbrain.
- Lipohyalinosis is the second common cause, which can lead to atherosclerosis. This leads to weakening of the wall of the vessel which eventually ruptures. This is mostly associated with hypertension. Almost all intracerebral hemorrhages occur due to rupture of small penetrating vessels, rather than the vertebral artery itself. This leads to hemorrhages in the deeper structures of the brainstem.
- Embolic occlusion of the vertebrobasilar system can occur due to thromboembolism from the heart (such as may occur in atrial fibrillation), the aortic arch, the subclavian artery, and the vertebral arteries. Embolus from these arteries flow along the blood into the basilar artery and occlude the arterial system of the brain.
- Vertebrobasilar artery dissection may occur due to trauma, such as hyperextension of the neck, chiropractic manipulation of the cervical spine and whiplash injury. This may also occur spontaneously in both healthy people as well as people who suffer from connective tissue disease.
- Aneurysms may occur in the vertebral artery and lead to complications such as hemorrhage due to rupture.
Epidemiology of Vertebral Artery Syndrome
Vertebral artery disease can lead to stroke. Among the total number of strokes, approximately 20 % occur after the disturbance of vertebrobasilar circulation.
Risk factors for vertebral artery disease
All these risk factors are associated with atherosclerosis and stroke. Some of these are modifiable and some are not modifiable.
Non Modifiable Risk Factors include:
- Age
- Family history of stroke
- Race/Ethnicity
Modifiable Risk Factors include:
- Hypertension
-
- Coronary and other heart diseases
- Diabetes mellitus
- Drug abuse
- Giant cell arteritis
- Obesity and physical inactivity
- Previous stroke
- Smoking
Clinical Presentation of Vertebral Artery Stroke Syndromes
Sudden occlusion of blood flow through the vertebrobasilar system leads to sudden death due to stroke, or major disability, such as the Locked-in syndrome. Focal neurological deficits may be observed if smaller branches (also known as the perforators) of the vertebrobasilar system are involved. The symptoms depend on the part of the brain or brainstem that has suffered ischemic injury.
Clinical History of Vertebral Artery Stroke Syndromes
Signs and symptoms of the disease depend on the etiology of the stroke. Embolic phenomenon leads to sudden symptoms which may occur without any prodromal symptoms. However, patients may have brief spells of similar symptoms that resolve spontaneously and last minutes to few hours, also known as transient ischemia (TIA), prior to the stroke.
Symptoms of vertebrobasilar strokes include:
- Vertigo – common – and this may be the only symptom
- Nausea and vomiting
- Disturbance of consciousness
- Headache
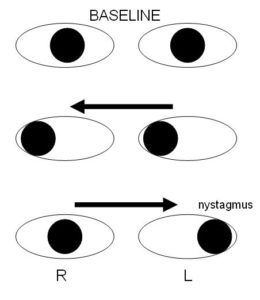
- Visual disturbance (oculomotor signs such as nystagmus, diplopia and pupillary changes)
- Visual field defects
- Speech disturbance (for example, dysarthria and dysphonia)
- Sensory changes over the face and scalp
- Ataxia
- Contralateral motor weakness (may cause a ‘drop attack’)
- Sensory disturbance affecting pain and temperature
- Incontinence
There may be a history of vascular risk factors. Vertebral dissection may be mistaken for musculoskeletal pain, since neck and occipital pain may occur, in the setting of exertion and excess mechanical activity or straining.
When the cerebellum is affected, symptoms include nystagmus, cranial nerve impairment, hemiplegia and loss of touch and vibration. Medial medullary syndrome and lateral medullary syndrome are important clinical syndromes in the setting of vertebral artery disease.
Neurological Examination Findings in Vertebrobasilar Syndromes
A key presenting feature of patients with vertebral artery syndrome is altered a state of consciousness or coma. In addition, the patient typically presents with signs of hemiparesis or quadriparesis. In some patients, facial nerve palsy with dysarthria, dysphagia, and dysphoniaalong with some disturbance of oculomotor and pupillary structures may occur.
The following syndromes may occur in the setting of vertebral artery disease:
Image: “Internuclear ophthalmoplegia” by Samir at the English language Wikipedia, License: CC BY-SA 3.0
- Lateral medullary or Wallenberg’s syndrome
- Medial medullary or Dejerine’s syndrome
- Cerebellar infarction
- Locked-in syndrome
- Internuclear ophthalmoplegia
- One-and-a-half syndrome
- Millard-Gubler syndrome
- Top-of-the-basilar syndrome
- Raymond-Céstan syndrome
- Foville’s syndrome
- Weber’s syndrome
- Benedikt’s syndrome
- Posterior cerebral artery occlusion
Clinical Approach to the diagnosis of Vertebral Artery Syndrome
The following investigations should be considered in the diagnosis of vertebral artery syndrome:
- Baseline labs: CBC, ESR, blood chemistry, clotting and lipid profile.
- If the patient is less than 45 years old, identifying a hypercoagulable disorder includes checking for:
- Lupus anticoagulant and anticardiolipin antibodies
- Antithrombin III deficiency
- Radiological investigations:
- CT scan of the brain, non-contrast: this is the first test done in the Emergency setting. CT scan is done to identify hemorrhage. CT Scan is not a sensitive tool to identify ischemia in the vertebral artery system or posterior circulation and should not be relied upon to do so.
- MRI scan of the brain is a more sensitive tool to identify ischemia.
- MR angiography is typically done simultaneously with the MRI, to identify abnormalities of the blood vessels, such as occlusion and/or dissection.
- ECG is done in all patients who are unconscious or have signs of stroke. 20 % of patients with stroke will have arrhythmias.
- Echocardiography: This is done to identify a possible cardioembolic source of the clot, if the stroke is presumed to be embolic. This is particularly important in younger patients, to identify valvular defects, valvular vegetations and other sources of emboli.
- Cerebral angiography is not done routinely. However, angiography is done to identify aneurysms, dissection, vasculitis or other unusual causes of stroke.
Management of Vertebral Artery Syndrome
Patients with vertebral artery stroke, as with any stroke, should be managed in a designated stroke unit with a neurologist, ideally trained in stroke care. General measures like preventing aspiration when the patient is bedridden to avoid pneumonitis, controlling body temperature, blood sugar, and blood pressure are crucial both to recovery and the likelihood of ever returning home.
Treating hypertension is a complex topic: however, in the setting of hypertensive emergency, gentle lowering of blood pressure may be reasonable. Patients should have frequent neurological assessments to evaluate for neurological worsening. Maintaining an airway and gag reflex is critical: patients who lose their gag reflex should be considered for endotracheal intubation. Addressing bowel and bladder care as well as maintaining critical care is crucial to improved outcomes.
Once the patient is stabilized, secondary prevention of another stroke is crucial. In the case of ischemic stroke, antiplatelet medication is important. In the US, antiplatelet options include aspirin, clopidogrel or dipyridamole. The routine use of intravenous heparin is not appropriate in the management of ischemic stroke.
In the setting of vertebrobasilar disease, angioplasty and stenting are not standard of care in the US.
Once the patient is medically stable, rehabilitation with aggressive physical therapy (physiotherapy) and occupational therapy as well as speech therapy has been shown to improve patient outcomes.
All of these measures are generalizable and do not apply to all patients. For example, some patients may be appropriate for palliative care: for example, those who are neurologically devastated, those who have a Living Will and/or those whose family determines that their comfort is most important. When this occurs, the patient no longer needs to be in a stroke unit, but rather in a setting more appropriate for the final hours of their life, with comfort as the primary goal of care.
Comentários
Enviar um comentário