Appendicitis — Definition and Surgery
Table of Contents
- Definition and Background of Appendicitis
- Epidemiology of Appendicitis
- Etiology of Appendicitis
- Pathophysiology of Appendicitis
- Symptoms of Appendicitis
- Signs of Appendicitis
- Special Tests on the Physical Examination
- Atypical Presentations of Appendicitis
- Diagnosis of Appendicitis
- Investigations of Appendicitis
- Differential Diagnosis
- Therapy/Treatment of Appendicitis
- Complications of Appendicitis
- Prognosis of Appendicitis
- Prevention of Appendicitis
- Review Questions
- References
Definition and Background of Appendicitis
Appendix: The appendix is a small, blind-ended, hollow, finger-like extension located at the start of the large intestine (cecum). It is also known as the vermiform process, which means ‘worm-like’ in Latin. It is 6 to 9 cm long and 8 cm wide although sizes can vary. The appendix has its own short triangular-shaped mesentery, the mesoappendix, and is supplied by the appendicular artery, which is a branch of the posterior cecal artery. The somatic nerve referral is to the periumbilical area.
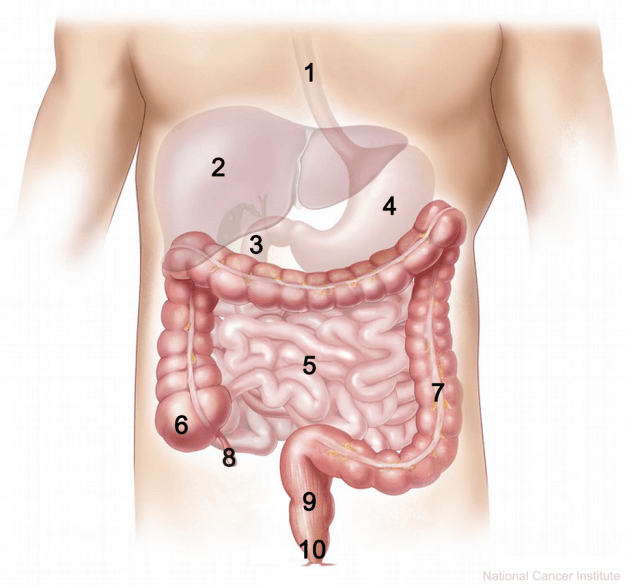
8 = appendix
Appendicitis: Appendicitis means inflammation (-itis) of the appendix. The appendix is often inflamed when it becomes blocked and infected. There is gradual swelling as the appendix fills with pus causing abdominal pain, vomiting, and acute illness. Since the appendix is a hollow structure, it can burst if left untreated. This perforation can rapidly lead to peritonitis and systemic sepsis, which is a life-threatening condition.
Surface anatomy of the appendix
The surface anatomy of the appendix is the right iliac fossa at a point called McBurney’s pointwhich lies at the lateral one-third of the way up the oblique line that joins the right anterior superior iliac spine to the umbilicus.
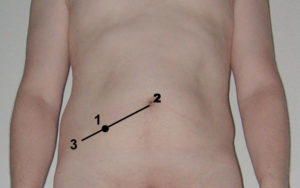
By Steven Fruitsmaak – I, Steven Fruitsmaak, am the creator. Based upon Image:A nude man standing.jpg, by Jasonz, which is GFDL. Edited with Adobe Photoshop., CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=1211886
Function of the appendix
The appendix is supposed to be a vestigial organ – meaning it has lost most of its original function. People can live normally without an appendix. The current theories suggest that the appendix may not be completely vestigial and its function is proposed to maintain gut flora, and act as part of our immune system as it contains gut-associated lymphoid tissue (GALT).
Histology of the appendix
Microscopy of a stained appendix slide reveals a very high density of gut-associated lymphoid tissue (GALT). The GALT-rich appendix harbors many immune cells (T-cells, B-cells, etc.), which protect the body from pathogens and are responsible for antigen detection. The crypts of Leiberkuhn contain many goblet cells which are responsible for the production of mucus.
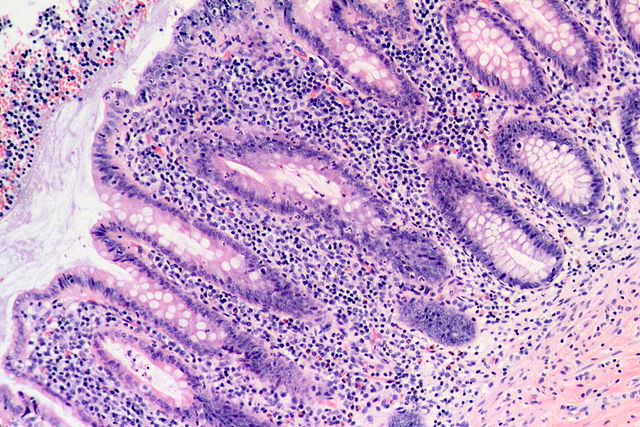
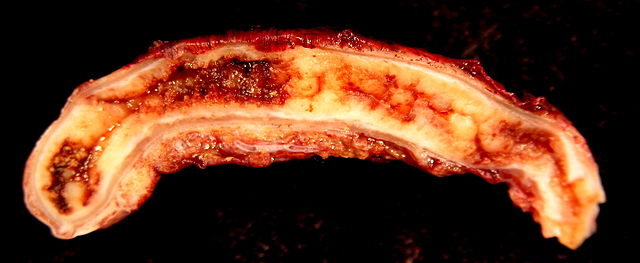
Image: “Acute Appendicitis.” by Patho. Licence: CC BY-SA 3.0
Epidemiology of Appendicitis
The appendicitis is one of the most common surgical emergencies worldwide but is more common in the West compared to the East (related to the typical low-fiber western diet). In 2013, there were 72,000 deaths globally from appendicitis. Appendicitis mostly affects teenagers and young adults but can occur at any age. It affects males slightly more than females. The lifetime risk of appendicitis is around 6%.
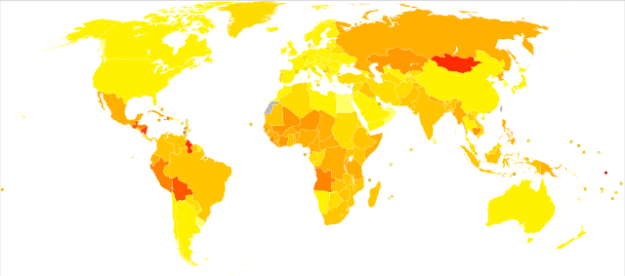
Image: “Age-standardised disability-adjusted life year (DALY) rates from Appendicitis by country” by Lokal_Profil. License: CC BY-SA 2.5
Etiology of Appendicitis
The majority of cases of appendicitis (50 – 80%) arise due to a primary obstruction. Usually, the appendicular wall muscles push the material back into the large intestines; if this fails, bacteria may thrive and cause an infection. (The appendix can also become inflamed and sterile when no bacteria are present.)
The obstructive agents include:
- *Fecoliths
- *Lymphoid hyperplasia – lymphadenopathy, infective mononucleosis, measles, respiratory infection (Streptococcal. Spp)
- Foreign bodies
- Intestinal worms
- Gallstones
- Tumors
(*Most common causes)
Common bacterial agents:
- Escherichia coli
- Bacteroides fragilis
(These bacteria are commonly found in the gut as part of the normal commensal flora).
Pathophysiology of Appendicitis
The obstruction of the appendix leads to a build-up of goblet cells, which continue to produce large amounts of mucous in spite of the obstruction. This causes abdominal pain in the periumbilical area. There is an inflammatory response consisting of swelling, and an infection from bacterial overgrowth, leading to an accumulation of pus; further, there is an invasion by neutrophils and activation of inflammatory mediators.
The infection and swelling cause further distension and an increase in the intra-luminal pressure. The pressure primarily occludes the venous drainage before occluding the arterioles; this leads to engorgement and congestion. At this point, the pain will localize to the right iliac fossa and surgical intervention will be needed as it rarely resolves past this point. The patient will now have systemic signs of illness, such as a fever, tachycardia, nausea, and anorexia.
If appendicitis continues untreated, the lack of blood supply leads to ischemia and eventually to necrosis. The walls of the appendix become weakened and pus begins to spread into the walls (muscular layer) forming focal abscesses (acute suppurative appendicitis). The pus contains dead lymphocytes from the inflammatory reaction, bacteria, cellular debris and fluid. This can progress further with large hemorrhagic ulceration and gangrene covering the full thickness of the appendix to the serosa (acute gangrenous appendicitis).
If the appendix ruptures, the infection spreads to the abdominal cavity and causes an infection of the lining known as peritonitis (suppurative peritonitis). This widespread infection is very dangerous and can be fatal if it spreads to the bloodstream causing septic shock.
This is a general outline of the pathogenesis. Note, however, that there are variations depending on the causative agent, the presence of bacteria and whether appendicitis resolves or progresses.
The process can be summarized as the following:
- Obstruction
- Increase in intraluminal pressure
- Mucosal edema and ulceration
- Decreased lymphatic and venous drainage
- Thrombosis/occlusion of appendicular arteries
- Bacterial proliferation and inflammation
- Lymphadenopathy
- Abscess
- Gangrene
- Perforation (1 – 2 days)
- Peritonitis +/- sepsis
Symptoms of Appendicitis
Acute appendicitis has a typical presentation of symptoms:
- Abdominal pain
- Nausea
- Vomiting
- Anorexia
- Constipation
Abdominal pain – usually starts periumbilically as the somatic nerve referral is to the periumbilical area (i.e. innervation of the appendix enters the spinal cord at the same point as the nerves of the umbilicus). The abdominal pain is typically very severe and colicky, keeping the patient awake. The pain later localizes to the right lower quadrant as the appendix irritates the parietal peritoneum.
Nausea and vomiting – Nausea is almost always present, whereas vomiting is less common.
Anorexia – Loss of appetite is common in acute appendicitis.
Bowel habit – The patient may also be constipated and may have reduced bowel movement. Diarrhea can also be present.
Signs of Appendicitis
Special Tests on the Physical Examination
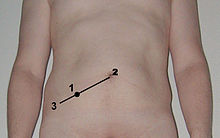 Image: “Location of McBurney’s point illustrated on the abdomen of a male subject.” by Steven Fruitsmaak. License: CC BY-SA 3.0McBurney’s sign – Deep tenderness at McBurney’s point is a sign of acute appendicitis. As already discussed, the McBurney’s point is the point on the right side of the abdomen, lateral one-third of the distance between ASIS (anterior superior iliac spine) and the umbilicus. It is also used to locate the appendix in surgery as it is the site of the appendix base where it attaches to the caecum.
Image: “Location of McBurney’s point illustrated on the abdomen of a male subject.” by Steven Fruitsmaak. License: CC BY-SA 3.0McBurney’s sign – Deep tenderness at McBurney’s point is a sign of acute appendicitis. As already discussed, the McBurney’s point is the point on the right side of the abdomen, lateral one-third of the distance between ASIS (anterior superior iliac spine) and the umbilicus. It is also used to locate the appendix in surgery as it is the site of the appendix base where it attaches to the caecum.- Rovsing’s sign – When pressure is applied to the left iliac fossa deeply and continuously, the patient with acute appendicitis feels pain in the right iliac fossa.
- Obturator sign – Pain on flexion and internal rotation of the right hip, due to the irritation from obturator internus.
- Psoas sign – pain when the right hip is passively extended/actively flexed. This movement relies on the iliopsoas muscle that may irritate the appendix or be inflamed itself.
- Digital rectal examination painful on the right – signs of the low-lying pelvic appendix; this may be present without abdominal rigidity.
Atypical Presentations of Appendicitis
- Lack the typical progression and may start with pain in the right lower quadrant.
- Flank or right upper quadrant pain and right-sided tenderness on digital rectal examination may be signs of retrocecal/retroperitonitis appendicitis (approximately 2 – 3%).
- Children can present with just general abdominal pain and anorexia.
- 0.1% of pregnancies experience appendicitis. Caution should be exercised as there is a higher risk of complications.
- Pain localizes to the left lower quadrant in ‘situs inversus totalis.’
Diagnosis of Appendicitis
Diagnosis is usually based on a detailed history and physical examination, along with investigations such as blood tests and imaging. The diagnosis must be made quickly to prevent further progression. Some scoring systems may be useful confirming diagnoses:
Alvarado scoring system (also called MANTRELS Score)
- 0-3: Appendicitis less likely. The patient can be discharged without imaging.
- 4-6: Possible. CT evaluation is needed.
- 7-8: Probable. Surgical consultation
- 9-10: Very probable: Surgical consultation
Typical presentations can be confirmed using blood tests (revealing leucocytosis) and imaging if required. However, atypical presentations almost always require radiological investigations. The most common types of imaging which are used include ultrasound and CT.
Investigations of Appendicitis
Differential Diagnosis
False-positive diagnoses can occur and normal appendices can occasionally be removed; this can be partially avoided with the use of imaging. The following conditions should be considered when the diagnosis is not certain:
- Pseudoappendicitis – mesenteric adenitis (lymphadenitis caused by Yersinia enterocolitica often preceded by a sore throat) is mostly seen in children; it typically mimics appendicitis.
- Infections – gastroenteritis, urinary tract infection, lobar pneumonia, systemic viral infection
- Gynecological conditions – testicular torsion, urinary tract infection, ectopic pregnancy, ovarian torsion, salpingitis (PID), endometriosis
- Other bowel conditions – New-onset inflammatory bowel disease (Crohn’s, Ulcerative Colitis), Meckel’s diverticulitis, diverticulitis, intussusception, intestinal obstruction, colonic carcinoma
- Other appendix conditions – carcinoid tumor, adenocarcinoma
- Other – abdominal trauma, renal colic, pancreatitis, peptic ulcer perforation, cholecystitis
Therapy/Treatment of Appendicitis
All suspected cases warrant hospital admission.
- If a patient presents in an emergency scenario, life support pathways should be followed: Airways, Breathing, Circulation, (A B C etc ) to stabilize the patient.
- Supportive treatments: Intravenous fluids, opiate analgesia (morphine), perioperative Intravenous antibiotics (reduces infective complications).
- IV Antibiotics: e.g. Metronidazole and Cefuroxime administered immediately if sepsis is suspected and perioperatively with IV hydration.
- Active observation: Can be useful if the diagnosis is uncertain.
- Appendectomy: Surgery is the gold standard treatment for appendicitis offering a rapid improvement in symptoms, low recurrence rate and evasion of the life-threatening complications of appendicitis more than any other treatment option. It is important that surgery is carried out as soon as possible; it can be conducted via open surgery or laparoscopically.
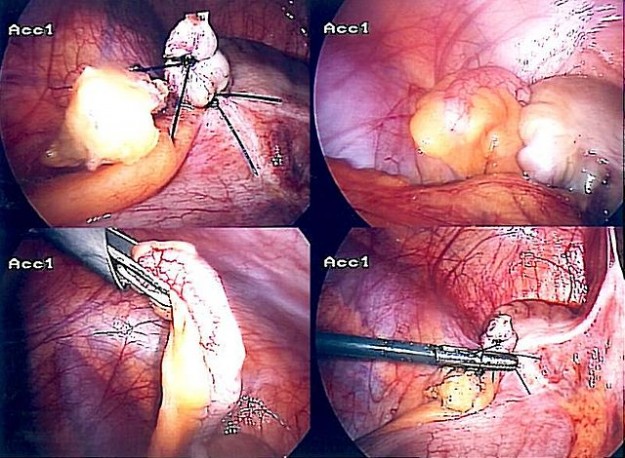
Appendectomy
Spontaneous resolution can occur, but, without surgery, there is an increased risk of re-admission. The procedure is usually carried out as an emergency procedure. Laparoscopic surgery offers reduced scarring and a quicker recovery time; hence, it is preferred over open surgery. An incision is usually made over McBurney’s point (as discussed earlier), which represents the appendix base.
The procedure was carried out over 300,000 times in the United States alone (2011) and represented over 2% of all procedures.
Contraindications: Inflammatory bowel disease; postoperative healing response is impaired; therefore treat with DMARDs (disease modifying anti-rheumatoid drugs).
Sepsis: If suspected: The sepsis pathway should be followed immediately.
- High-flow oxygen
- Blood cultures
- IV antibiotics
- Fluid challenge
- Measure lactate
- Measure urine output
Recovery – hospital stays usually last a few days after surgery. However, if a complication arises, it can be extended to a few weeks. It also depends on whether the appendix has ruptured, as this is an indication of severity. It is advised that the patient rests and avoids physical activity (some movement is encouraged). Full recovery takes 4 – 8 weeks, again depending on severity.
Complications of Appendicitis
- Perforation – Between 16 – 30% suffer from perforation (higher in the extremes of age and when a fecolith is a cause).
- Peritonitis – Spread of infection from a perforated appendix can cause peritonitis. It is very serious and can be fatal if the infection spreads to the bloodstream, causing septic shock. Rapid treatment is essential. Signs of peritonitis include increasingly severe abdominal pain, nausea, and vomiting, anorexia, fever and oliguria/anuria.
- Appendicular mass – Presentation is usually fever with a palpable mass; the mass is formed when small bowel and omentum cover the inflamed appendix. Surgery is an option, along with initial conservative management (nil by mouth with antibiotics). Need to rule out other causes of such masses like colonic cancer.
- Appendicular abscess – Can result from an unresolved appendicular mass that enlarges. Ultrasound and CT scans can reveal abscesses which usually can be treated by drainage during open appendectomy or percutaneously with radiological guidance.
- Wound infection – Risk depends on the severity of the case. Perioperative antibiotics reduce the risk.
Prognosis of Appendicitis
The surgical procedure is relatively safe with a mortality of 0.8/1000 (non-perforated) and 5/1000 for perforated cases. This relies on early detection, management, and rapid surgical treatment to avoid further complications.
If the patient presents with severe appendicitis with perforation, the prognosis is significantly worse as there is a risk of life-threatening peritonitis and sepsis.
Prevention of Appendicitis
There is no way to prevent appendicitis. However, there is a lower occurrence in people with a fiber-rich diet. Early detection and treatment is essentially a cure and prevents further progression of the disease.
Review Questions
The correct answers can be found below the references.
1. A 17-year-old male is brought to the emergency department complaining of severe right lower quadrant pain. It has been going on for 1 – 2 days and has started in the umbilical region. He now has a temperature of 100.5 Fahrenheit (38.1 degrees Celsius) and is very nauseous. He has not vomited but has not eaten in over a day. You diagnose appendicitis and begin fluids and basic supportive measures (e.g. pain relief). What is the next step?
- Observe the patient
- Refer to a surgeon for an appendectomy
- Start on IV antibiotics
- Send home
- X-ray abdomen
2. The patient is consequently referred to surgery. The surgeon performs laparoscopic surgery to remove the appendix. Which one of the following is not an advantage of laparoscopic surgery over open surgery?
- Faster recovery time
- Less invasive
- Less scarring
- Reduced post-operative disability
- Longer operating time
3. A 35-year-old female presents with worsening abdominal pain in the right iliac fossa and the physician demonstrates rebound tenderness. He suspects acute appendicitis. The doctor proceeds to perform another test; with the patient supine, he flexes the knee and hip at 90 degrees and then internally rotates the right hip (holding and moving ankle away from her body, whilst allowing her knee to move inwards only). During this procedure, the doctor observes the patient’s face and notices that she grimaces in pain. It is repeated with the left hip, but there is no pain noted. Which muscle is coming into contact with the inflamed pelvic appendix and has an irritating effect on it?
- Superior gemellus
- Obturator externus
- Piriformis
- Obturator internus
- Gluteus minimus
Comentários
Enviar um comentário