Goiter (Enlarged Thyroid) — Classification, Symptoms and Diagnosis
Table of Contents

Image: “Struma with large palpable knot pretracheal” by Drahreg01. License: CC BY-SA 3.0
Definition of Goiter
Goiter as a symptom
Goiter is a symptom that describes the enlargement of the thyroid gland.
The term “goiter” is purely descriptive in nature and thus reveals
nothing about the pathogenesis or the functional status of the thyroid
gland. Goiter may be associated with normal functioning thyroid gland
(euthyroid goiter), overactive thyroid gland (toxic goiter), or
underactive thyroid gland (hypothyroid goiter).
Goiters may extend into the retrosternal space, with or without
substantial anterior enlargement. Because of the anatomic relationship
of the thyroid gland to the trachea, larynx, superior and inferior
laryngeal nerves, and esophagus, abnormal growth may cause a variety of
compressive syndromes.
What does an enlarged thyroid mean?
An enlarged thyroid also known as goiter refers to the increase in
size of the thyroid gland. The thyroid is an endocrine organ located on
the anterior aspect of the neck region as two butterfly shaped lobes on
each side of the trachea each measuring 4-6 cm by 1.2-1.8 cm and a
central isthmus that measure 4-5 mm in diameter. An increase in any of
the above measurements refers to thyroid enlargement that may be
asymptomatic or present with features of mass effect.
Epidemiology of Goiter
Goiter — Common findings
The WHO estimates that two billion people, including 285 million
school-age children still have the iodine deficiency. Goiter is endemic
in areas where daily iodine intake is lower than 50 μg and congenital
hypothyroidism is risked when the daily intake further falls to 25 μg.
The prevalence of goiter in areas of severe iodine deficiency can be as
high as 80%. Overall, women are more often affected than men.
Classification of Goiter
Classification of goiter-size stages by WHO
| 0 | No goiter |
| Ia | Palpable goiter, not visible when bending the head back, solitary nodule |
| Ib | Palpable goiter, only visible when bending the head back |
| II | Visible and palpable goiter even without the reclining head |
| III | Goiter visible at a distance, with obstruction of the trachea and esophagus or spreading behind the sternum |
Classification of goiter after thyroid hormone function
| Euthyroid | Thyroid hormone level in the normal range |
| Hypothyroidism | Decreased thyroid hormone level |
| Hyperthyroidism | Increased thyroid hormone level |
Etiology and Pathogenesis of Goiter
Causes of goiter
A deficiency in thyroid hormone synthesis or intake leads to
increased thyroid-stimulating hormone (TSH) production. Increased TSH
causes increased cellularity and hyperplasia of the thyroid gland in an
attempt to normalize thyroid hormone levels. If this process is
sustained, a goiter is established.
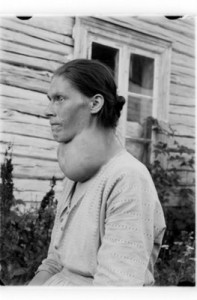
Image: “Women with struma” by Arkiv for Ringsaker, Hamar, Vang, Stange og Løten, Hedmarksmuseets fotoarkiv, HHB-00185. License: Public Domain
The most common cause in industrialized countries is an endemic iodine deficiency
(alimentary iodine deficiency). In countries where iodine is routinely
added to table salt and other foods a lack of dietary iodine is not the
main cause, other possible causes are responsible:
Inflammation
- Autoimmune disorders of thyroid (Graves’ disease, Hashimoto’s thyroiditis)
- Medications (phenytoin, lithium, anti-thyroid drugs, carbimazole)
Thyroid autonomy
Thyroid tumors
- Neoplastic production of TSH
- Acromegaly
- Iodine failed use
Symptoms of Goiter
An enlarged thyroid gland may present with:
- Features of mass effect such as discomfort to the enlarging mass, difficulty in breathing once the airway is compressed and difficulty in swallowing that arises from compression of the esophagus.
- Features of hyperthyroidism in toxic goiters which mainly arise from activation of the autonomic nervous system by the hormones from the glands. The features include fast heartbeat, increased sweating, anxiety, heavy menstrual bleeding, tremors and heat intolerance.
- Features of hypothyroidism in non-functional goiters which occur due to deficiency of the hormones. They include a slow heart rate, weight gain despite poor appetite, lethargy, scanty menstrual flow, infertility and cold intolerance.
- Features of invasiveness if the enlargement is cancerous which include weight loss due to increased basal metabolic rate and hoarseness of voice due to the encroachment of the recurrent laryngeal nerve by the tumor.
- Features of inflammation if the enlargement is infective or autoimmune in nature such as pain in the neck.
- Hemorrhage and/or necrosis may be a result of traumatic injury to the organ.
Non-specific symptoms of goiter
Most goiters are asymptomatic. A visible thyroid enlargement can only
be seen from a volume of about 40 ml. The enlargement of the thyroid
gland can be accompanied by a mechanical compression of surrounding
organs (tracheal and/or Esophagus compression).
The extent to which goiter is symptomatic essentially depends on the
location. In the case of retrosternal or retrotracheal growth, it may
restrict the larynx and trachea in their anatomical position so much that dysphagia, dyspnea and hoarseness may occur.
In the case of esophagus compression, the patient may complain of
globus or pressure sensation in the throat, as well as problems with
swallowing. It may accompany pain in thyroid region and cough.
| Common Symptom | Restricted Organ/Tissue |
| Stridor, hoarseness, dyspnea | Compression of the trachea |
| Dysphagia, globus sensation | Compression of the larynx and/or trachea |
| Inflow congestion | Compression of the neck veins |
Specific symptoms of goiter
Clear indications of the possible presence of goiter are diffuse or nodular enlargement of the thyroid tissue.
Diagnosis of Goiter
First signs of goiter
Avoiding necklaces, turtlenecks or an increase in the collar size can
be regarded as the first indication of the presence of goiter.
Anamnestic response in suspected goiter
A detailed medical history may provide the first evidence for the presence of a goiter. What should be questioned in detail:
- Duration and progression of thyroid enlargement
- Possible exposure of the head and neck region
- Recently occurred hoarseness
- Hormonal changes (puberty, pregnancy, menopause)
- Taking medications
- Iodine intake
- Family history
Goiter clinic
You should start with a physical examination i.e. inspection of the
enlargement. At the beginning of a first-glance examination, you may
work with the goiter-size stages classification provided by WHO (see
above). You should examine the thyroid gland with a straight back and a
bowed head. You should pay attention to a possible visible enlargement
as well as nodes and signs of upper inflow congestion.
Palpation is the second step of examination. During the physical
examination, it allows making further judgment in regards to the
extension of a goiter and other clinical signs of malignancy. Important
points in this case are:
- Mobility of tissues;
- Any enlargement of tissues;
- Uniform consistency of tissues;
- Possibly, to palpate lumps and nodes;
- Buzz under the palpating fingers;
- Increased sensitivity to touch;
- Tenderness;
- Lymph node enlargement.
In addition to palpation, you may also use auscultation.
If there is an increased blood supply to the thyroid tissue, this can
be perceived as an audible buzz auscultation. If it happens, you should
think of the presence of hyperthyroidism.
Further diagnosis in the presence of goiter
With an anamnestic history and physical examination of the suspected goiter, the following examinations should take place:
- Ultrasonography of the thyroid gland for accurate detection of thyroid enlargement and morphological differentiation of the various forms of goiter.
- Determination of TSH, TRH, free T3 and free T4 for the evaluation of thyroid function.
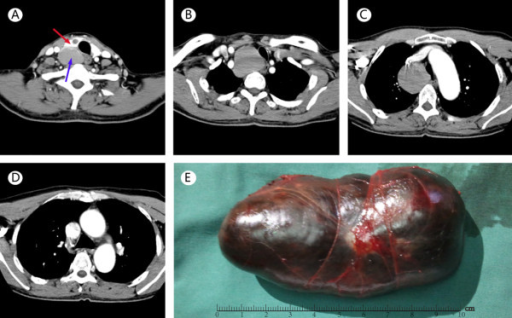
Image:
“CT scanning and complete excision of giant thyroid goiter in posterior
mediastinum. (A) Enhanced CT scanning reveals the right thyroid lobe
(in red arrow) with a small cyst and a giant goiter (in blue arrow) in
low density on the back of the right lobe. (B) CT clavicle cross section
reveals the giant goiter was located in the posterior mediastinum,
compressing the trachea and esophagus. (C) CT of the chest reveals the
goiter is well beyond the aortic arch and compressing the superior vena
cava. (D) CT of the chest reveals the lower edge of the goiter reaches
the carina of the trachea. (E) The tumor is in a complete capsule with
large tension,” by Openi. License: CC BY 2.0
With a multinodular or nodular goiter, the following questions are to
be answered: Is a thyroid autonomy available? Is it a benign change or a
tumor, if the tissues have changed? In order to get a differentiated
answer to these questions, the following further diagnostic modalities
should be considered:
- Laboratory tests;
- Scintigraphy;
- Unenhanced computed tomography;
- Magnetic Resonance Imaging;
- Fine-needle biopsy.
Differential Diagnosis of Goiter
Various forms of goiter
The diagnosis of goiter initially leads to the differentiation into diffuse and nodular goiter.
| Goiter Form | Description | Disease |
| Euthyroid goiter (bland goiter) | Benign, with euthyroid serum levels and normal thyroid function. | With normal serum levels without direct clinical significance. |
| Euthyroid nodular goiter/ multinodular goiter | Nodular goiter, at the beginning mostly euthyroid; in the further course, there are signs of hyperthyroidism. | Hyperthyroidism |
| Diffuse goiter (struma parenchymatosa | Not definable enlargement of the thyroid gland with uniform growth; common cause: iodine deficiency. | Puberty goiter, Graves’ disease |
| Basedow’s goiter | Diffuse parenchymal goiter with abundant vascular development, liquid colloid and epithelium tumor. | Graves’ disease |
| Lymphatic goiter Hashimoto (struma lymphomatosa Hashimoto) | Over the years, increasing focal or diffuse lymphocytic or plasma cellular infiltration of the thyroid, formation of lymphocytic follicles; final stage: fibrosis and disappearance of goiter parenchyma. | Hashimoto’s thyroiditis |
| Neonatal goiter | Thyroid enlargement in the newborn, endemic in iodine-deficient areas. | Goiter in the new-born |
Differential diagnosis of thyroid enlargement
Main cause for the diffuse goiter is an alimentary iodine deficiency
situation in industrialized countries. Consequence of this is a
TSH-independent adaptive response in the form of hyperplasia. If there
is an enlarged thyroid gland, you have to think about a differential
diagnosis should include:
- Diffuse goiter parenchymatosa;
- Hypertrophic Hashimoto’s thyroiditis;
- Graves’ disease;
- De Quervain’s thyroiditis;
- Invasive sclerosing thyroiditis (“Riedel’s thyroiditis”);
- Amyloidosis;
- Acromegaly.
Differential diagnosis of euthyroid nodular goiter
After noting an euthyroid nodular goiter, possible malignant and
inflammatory changes, as well as functional autonomies, have to be
excluded. It should be included in the differential diagnosis in case
of:
- Graves’ disease
- Functional autonomy (focal or disseminated)
- Malignant tissue changes (thyroid cancer)
- Hashimoto’s thyroiditis

Image:
“Sonogram of the thyroid gland (right lobe in longitudinal section) in
Hashimoto’s thyroiditis in the hypertrophic form. Typical echo
disorder..” by Drahreg01. License: CC BY-SA 3.0
Laboratory diagnosis of nodular and multinodular goiter
For the avoidance of medullary thyroid carcinoma (MTC), the
determination of thyroid autoantibodies is recommended via sonographic
examination of:
- Thyroid peroxidase antibodies (TPO antibodies) and
- TSH receptor antibodies (TRAB).
Other laboratory parameters to check the thyroid function are:
- Free Triiodothyronine (T3);
- Free Thyroxine (T4);
- Thyroid-stimulating hormone (TSH);
- Thyroid releasing hormone test (TRH test);
- Microscopic antibodies (MAbs);
- Thyroglobulin antibodies (TgAb).
Differential diagnosis of multinodular goiter
A particular challenge in the differential diagnosis of thyroid disease is a multinodular goiter. By means of ultrasonography and scintigraphy, you should be able to identify suspicious focal or disseminated autonomies (a cold/hot node) and make further analysis. The aim of examination is the detection or exclusion of thyroid autonomy.
If conspicuous nodes are detected by scintigraphy, they would require
further clarification, which, in turn, should take place by means of
fine-needle biopsy. The main purpose of the fine-needle biopsy in this
case is the selection of thyroid nodules for the earliest possible
histological evaluation of clinically normal or malignant tumors (thyroid carcinoma).
Differential Diagnosis of Throat Swelling
Not every throat swelling should be regarded automatically as a
goiter. Goiter is abnormal swelling of the thyroid gland only with a
definite underlying cause. A throat swelling can also occur as part of
an increase in the volume of parathyroid glands, salivary glands, lymph
nodes and the skin, the blood vessels, the muscles or the skeletal
system. The differential diagnosis takes the following specific causes
into consideration:
| Possible Disease | Frequency |
| Goiter | Frequently |
| Lymphadenopathy due to infections, sarcoidosis, lymphadenitis, etc. | Very often |
| Salivary gland swelling (tumor/stone/inflammation) | Less common |
| Thrombosis or tumor-related superior vena cava syndrome | Rarely |
Management of Goiter
Treatment of individual goiter forms
The treatment of goiter is required only in case of complaints, a
proven thyroid autonomy or well-secured malignancy. Initially, the motto
“wait and watch” should be applied with asymptomatic patients. However,
if waiting is contraindicated, there is a possibility of drug therapy (levothyroxine, iodide).
In addition, a radioiodine therapy or surgical therapy may be
considered. In some cases, radioactive iodine is used to treat an
overactive thyroid gland which results in the destruction of thyroid
cells.
Having said that, each therapeutic procedure should be reviewed in
terms of its suitability prior to taking action. Thus, the majority of
patients with a nodule would first require no treatment, whereas, the
treatment with malignancy is unquestionable. The thyroid surgery is
obligatory for malignancy!
In the case of euthyroid diffuse goiter iodine deficiency is the main cause. Thus, the goal of any treatment should be the correction of iodine deficiency.
In the case of retrosternal or mediastinal goiter expansion, with the impairment of adjacent organs of the respiratory and digestive tract, a thyroidectomy in the affected region should be considered.
In the case of euthyroid diffuse goiter iodine deficiency is the main cause. Thus, the goal of any treatment should be the correction of iodine deficiency.
In the case of retrosternal or mediastinal goiter expansion, with the impairment of adjacent organs of the respiratory and digestive tract, a thyroidectomy in the affected region should be considered.
Prevention of goiter
Goiter prevention is largely influenced by its specific etiology. Preventive measures may include;
- Correction of iodine deficiency and avoidance of dietary goitrogens. This is achieved through intake of iodine supplemented foods more often.
- Careful use of levothyroxine combined with anti-inflammatory medication therapy plays a vital role in prevention and reduction of goiters due to autoimmune thyroiditis.
- Use of levothyroxine in patients with a previous diagnosis of nodular hyperplasia who have had a lobectomy, prevent its subsequent development in the contralateral lobe.
- In the case of newborns screened for positive congenital hypothyroidism. Controlled use of levothyroxine during the postpartum period greatly reduces risks involved with congenital goiters due to inborn errors of metabolism.
Important to Remember
- Goiter is a symptom, not a disease.
- Initially, it indicates the enlargement of the thyroid gland.
- Rough classification of goiter: diffuse and nodular goiter types.
In case of a goiter suspicion, you should always exclude a possibly present malignancy.
Evidences of a goiter include:
Evidences of a goiter include:
- Thyroid enlargement;
- Nodules under the palpating fingers;
- Dysphagia;
- Dyspnea;
- Hoarseness;
- Difficulty swallowing, etc.
The examination of the eventually degenerated thyroid tissues occurs via ultrasonography, scintigraphy and fine-needle biopsy.
In addition to goiter, further possible changes of the neck should be taken into consideration when a throat swelling is present. They may indicate entirely different diseases, such as swollen lymph nodes or the increase in the volume of salivary glands.
In addition to goiter, further possible changes of the neck should be taken into consideration when a throat swelling is present. They may indicate entirely different diseases, such as swollen lymph nodes or the increase in the volume of salivary glands.
Review Questions
The answers are below the references.
1. A lack of iodine cannot result in:
1. A lack of iodine cannot result in:
- lowering of thyroid stimulating hormone (TSH) plasma concentration.
- reduction of triiodothyronine plasma concentration.
- thyroid enlargement (goiter).
- growth failure.
- disturbances of intellectual development.
2. Triiodothyronine (T3) and thyroxine (T4) hormones are
formed in the thyroid. The precursor of these hormones is deposited
extracellularly in the follicles from which the finished thyroid
hormones are released by intracellular proteolysis. What is located in
the follicles of the thyroid gland?
- Thyroglobulin
- Thyrotropin-releasing hormone (TRH)
- Iodate
- Thyroxine-binding globulin
- Transthyretin
3. Disorders in the synthesis of thyroid hormones and
regulation of the thyroid function are associated with a variety of
symptoms in children and adults. Hyperthyroidism can be caused by
autoantibodies that are bound to receptors with the thyroid epithelial
cells. Which receptors are activated by these autoantibodies?
- Somatostatin
- Thyreocalcitonin
- Thyroid-stimulating hormone (TSH)
- Thyreostatin
- Thyroliberin (TRH)

I am very much obliged to you for sharing this necessary knowledge. This information is very helpful for everyone. So please always share this kind of information. Thanks once again for sharing it. Best surgeon in Bakersfield CA
ResponderEliminar