Infant Respiratory Distress Syndrome (IRDS) — Symptoms and Treatment
Table of Contents
Etiology and Pathophysiology of IRDS
Discussing the normal lung development is important to understand the pathophysiology of neonatal respiratory distress syndrome.
Fetal lungs during the intrauterine life are not functional and filled with fluid, where the oxygen is delivered to the fetus through the placenta. Fetal lungs start to produce the surfactant during the third trimester of the pregnancy. The surfactant reduces tension within the alveoli, thereby preventing their collapse at the end of the expiration which may result in atelectasis, and facilitating the alveolar expansion.
Surfactant production
- It’s synthesized by the alveolar type II cells by 20 weeks of gestation.
- It appears in amniotic fluid between 28 and 32 weeks.
- Mature levels are usually present after 35 weeks.
The major constituents of surfactant are:
- Dipalmitoyl phosphatidylcholine (lecithin).
- Apoproteins (surfactant proteins SP-A, -B, -C, -D).
- Cholesterol.
Phosphatidylglycerol:
Phosphatidylglycerol level begins to rise in amniotic fluid after 35 weeks of gestation and is used as a marker for fetal lung maturity. Instead of high levels of phosphatidylglycerol in mature lungs, immature lungs contain a larger amount of phosphatidylinositol than a smaller amount of phosphatidylglycerol.
Synthesis of the surfactant depends on gestational age, pH, temperature and perfusion:
- Gestational age: The earlier gestational age (prematurity), the more risk of RDS.
- pH: Any clinical condition causes fetal acidosis and may result in diminished surfactant synthesis.
- Temperatures: Such as cold stress can suppress surfactant synthesis.
- Perfusion: Intrapartum asphyxia, hypovolemia or hypotension can suppress surfactant synthesis.
The primary problem of Respiratory Distress Syndrome (RDS) is surfactant deficiency in the premature lungs which results in higher surface tension; thus, greater pressure is required to expand the alveoli, and small airways leading to instability of the lung at end-expiration, low lung volume and decreased compliance. These changes may result in the collapse of portions of the lungs (atelectasis) leading to a mismatch between ventilation and perfusion, which causes hypoxia, hypercapnia, and acidosis.
The combination of hypoxia, hypercapnia, and acidosis may result in pulmonary arterial vasoconstriction with increased right-to-left shunting through the foramen ovale and ductus arteriosus → thus the pulmonary blood flow is decreased resulting in ischemia of surfactant-producing alveoli and the alveolar bed with subsequent effusion of proteinaceous material into the alveolar spaces, resulting in pulmonary edema and increased airway resistance.
Risk Factors of IRDS
- Prematurity: The smaller the gestational age, the higher incidence of RDS.
- Maternal Diabetes: Maternal hyperglycemia causes fetal hyperinsulinemia which antagonizes the action of cortisol; therefore delays the maturation of surfactant production in the lungs.
- Cesarean section (C.S) without labor: A lack of stressful delivery results in reduced fetal cortisone production.
- Perinatal asphyxia: Due to the hypoxemic injury if the alveolar cells type 2.
- Male gender.
Clinical Manifestations of IRDS
The clinical manifestations arise mainly from the abnormal pulmonary function and the hypoxemia.
Symptoms of neonatal respiratory distress syndrome
RDS starts within minutes or hours after birth, and becomes progressively worse over the first 48 – 72 hours of life:
The affected infants are typically premature and show signs of respiratory distress:
- Tachypnea.
- Nasal flaring.
- Expiratory grunting, which results from expiration against a partially closed glottis.
- Cyanosis.
By auscultation:
- Breath sounds may be normal or diminished with a harsh tubular quality.
- Bilateral fine basal rales.
Course of RDS
Uncomplicated RDS typically progressed for 48 – 72 hours, can be followed by increased endogenous production of surfactant and resolution of the respiratory distress by one week of age. Treatment with exogenous surfactant improves the course of the disease and leads to a resolution of symptoms.
Severe RDS or those inadequately treated may develop:
- Hypotension
- Cyanosis
- Pallor increase
- Grunting decrease or disappear
- Mixed respiratory-metabolic acidosis
- Apnea and irregular respirations which indicate fatigability
Complications of neonatal respiratory distress syndrome
- Image: “Pulmonary Interstitial Emphysema” by Rivard.M. License: CC BY-SA 3.0Respiratory failure
- Alveolar air leaks (interstitial emphysema, pneumothorax)
- Pulmonary hemorrhage
- Intraventricular hemorrhage
Diagnosis of IRDS
Diagnosis of neonatal respiratory distress syndrome (RDS) is based mainly on the previously mentioned clinical picture of a premature infant, in conjunction with:
Characteristic chest x-ray findings in RDS
- Diffuse reticulogranular pattern (ground glass appearance)
- Air bronchograms: Outline of air filled large airways against opaque lungs
They are often more prominent early in the left lower lobe because of superimposition of the cardiac shadow.
Arterial Blood Gas (ABG) in RDS
- Typically shows hypoxemia which response to oxygen supplementation
- Disease worsens, hypercapnia develops
- Metabolic acidosis
Differential Diagnosis of Dyspnea after Birth
Transient tachypnea
Symptoms:
Usually follows an uneventful normal term vaginal delivery or cesarean delivery with early onset of tachypnea, sometimes with retractions or expiratory grunting + typically, cyanosis that is relieved by minimal oxygen.
Examination:
Lungs usually clear without rales or rhonchi
Chest X-ray shows:
- Prominent pulmonary vascular markings
- Fluid lines in the fissures
- Over aeration
- Flat diaphragm
- Pleural fluid
Transient = Hypoxemia, hypercapnia, acidosis are uncommon
Persistent pulmonary hypertension of the newborn (PPHN)
Persistence of the fetal circulatory pattern of right-to-left shunting through the POA and foramen ovale after birth is due to very high pulmonary vascular resistance.
Clinically:
Should be suspected in all term and post-term infants with cyanosis unresponsive to 100% oxygen with or without fetal distress.
Chest X-ray:
- May be normal or
- May show parenchymal opacification in the chest, depending on etiology
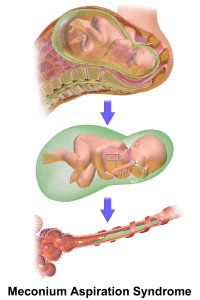
Meconium aspiration
Image: “Meconium Aspiration Syndrome (MAS)” by BruceBlaus. License: CC BY-SA 4.0
Occurs in term or post-term infants
Occurs either in utero or more often with the first breath, thick and particulate meconium is aspirated into the lungs, resulting in:
- Small airway obstruction and consequent → respiratory distress that presents within the first hour of birth
- Partial obstruction of some airways → may lead to pneumothorax or pneumomediastinum
Chest X-ray:
Image: “Chest X-ray of female neonate with meconium aspiration” by Kinderradiologie Olgahospital Klinikum Stuttgart. License: CC BY-SA 4.0
- Patchy infiltrates, coarse streaking of both lung fields
- Increase anteroposterior diameter
- Flattening of the diaphragm
Choanal Atresia
It is the most common nasal malformation. It may be isolated or part of a dysmorphic syndrome. Suspect choanal atresia in who presents with cyclic cyanosis that is aggravated by feeding and relieved by crying.
The severity of symptoms depends on:
- The ability of the infant to breathe through the mouth.
- Whether one or both choanae are obstructed.
- Unilateral choanal atresia may remain undiagnosed until the infant develops a first upper respiratory infection.
- Failure to pass a catheter through the nose 3 – 4 cm into the oropharynx is suggestive of the diagnosis.
- Investigations: Diagnosis is confirmed by a CT scan with intranasal contrast, which shows narrowing at the level of the pterygoid plate.
Definitive treatment:
- The first step in management consists of placing oral airway + lavage feeding.
- Repairing the obstruction with surgery or endoscopy.
Congenital Diaphragmatic Hernia
Antenatal history is significant for polyhydramnios in the mother.
Symptoms: Immediately develop bluish discoloration of extremities soon after birth, respiratory distress.
Examination:
- Tachypnoea and nasal grunting.
- Inspection: Abdomen has scaphoid shape.
- Auscultation: Poor air entry on the left with a shift of cardiac sounds to the right.
X-ray shows:
Image: “Congenital right sided diaphragmatic hernia in a neonate, chest X-Ray” by Kinderradiologie Olgahospital Klinikum Stuttgart. License: CC BY-SA 4.0
- Air or fluid-filled bowel loops in the hemithorax.
- The shift of cardiac shadow to opposite side.
- Placement of orogastric tube before chest X-Ray helps determine the position of the stomach.
Management: If the infant has a CDH, or if the diagnosis is suspected in the delivery room:
- First step: Immediate placement of orogastric tube and connecting it to continuous suction, to prevent bowel distension and further lung compression.
- Endotracheal intubation and mechanical ventilation are also priorities for severe CDH.
⇒ CDH is sometimes associated with primary pulmonary hypertension of the newborn (PPHN):
- Continuous pulse oximetry is valuable in the diagnosis and management of PPHN.
- If PPHN is present with the right to left ductal shunting, then Pa02 may be higher from a preductal (right-hand) sampling site.
- Cardiac ultrasonography can be performed to rule out congenital heart diseases.
Management of IRDS
Prevention of neonatal respiratory distress syndrome
As the respiratory distress syndrome is a disease of prematurity, the most effective preventive method is to avoid the pre-term labor. However, if the pre-term labor can’t be avoided, RDS can be prevented, or its severity decreased by the following interventions:
1. Antenatal corticosteroids therapy:
- Steroid enhances surfactant synthesis and release and accelerates lung maturity.
- Indications: All pregnant women at risk of pre-term labor, or below 34 weeks.
- Dose: Betamethazone 12mg/IM, two doses 24 hours apart.
2. Exogenous surfactant replacement therapy:
Several studies have revealed benefits of exogenous post-natal surfactant administration in preterm infants born < 30 weeks gestation.
3. Continuous positive airway pressure (CPAP):
Indications:
- Premature infants at risk (e.g., low birth weight infants, born at or below 28 weeks gestation).
- Already established RDS but without respiratory failure.
CPAP is considered alternative to endotracheal intubation or mechanical ventilation to prevent the development of atelectasis.
Treatment of neonatal respiratory distress syndrome
General Supportive Measures:
Early supportive measures aim to control the inadequate exchange between the oxygen and carbon dioxide exchange, metabolic acidosis and circulatory insufficiency.
Thermal regulation:
Avoid the neonatal hypothermia by placing the infant in an isolette or radiant warmer and core temperature maintained between 36.5 and 37°C.
Image: “Necrotizing enterocolitis” by RadsWiki. License: CC BY-SA 3.0
Fluid Supply:
You should be careful with the administration of fluid, as the kidneys have limited concentrating abilities and administration of large volumes of fluid may increase the risk of Patent Ductus Arteriosus (PDA) and necrotizing enterocolitis (NEC).
Nutrition:
Early nutrition is important and should meet the metabolic needs of the infants.
Cardiovascular Support:
Blood pressure of a premature infant should be monitored, and hypotension should be treated with:
- Normal saline (with caution)
- Vasopressors
- Stress doses of hydrocortisone (in persistent hypotension).
Specific Interventions:
The specific interventions to premature infants are based mainly on:
- Gestational age
- Respiratory status of the infant within the first hour after delivery
- Humidified oxygen should be provided in low concentration to keep Pao2 between 50 and 70 mm Hg (85 – 95% saturation) to maintain tissue oxygenation and avoiding the risk of oxygen toxicity; pH should be maintained > 7.25.
- CPAP at a pressure of 5–10 cm H2O should be provided if initial oxygen supply with the concentration greater than 60% couldn’t maintain Pao2 above 50 mmHg.
- Assisted Mechanical Ventilation is indicated if a respiratory failure occurred (Pco2 > 60 mm Hg, pH < 7.20, and Pao2 < 50 mm Hg despite 100% oxygen).
Review Questions
The answers are below the references.
1. The incidence of respiratory distress syndrome (RDS) increases with all of the following risk factors except:
- Maternal diabetes.
- Prematurity.
- Caesarean section delivery.
- Female gender.
2. The main pathophysiological cause of neonatal respiratory distress syndrome is…
- …surfactant deficiency.
- …hypoplasia of the lungs.
- …incomplete development of the alveoli.
- …alveoli that are abnormally filled with fluid.
3. A premature infant was born at 28 weeks of gestation, and, after 3 hours of birth, he developed tachypnea and intercostals retractions. An X-Ray was asked and a diagnosis of respiratory distress syndrome (RDS) was made and, after 100% oxygen therapy, the APG of the infant showed: Pco2 > 60 mm Hg, pH < 7.20, and Pao2 < 50 mm Hg. The most appropriate next step in management is:
- Give higher concentrations of oxygen.
- Start Continuous Positive Airways Pressure (CPAP).
- Start Assisted Mechanical Ventilation.
- Administrated exogenous surfactant.





Comentários
Enviar um comentário