Myocardial Infarction (Heart Attack) — STEMI vs. NSTEMI
Table of Contents
- Definition of Myocardial Infarction
- Epidemiology of Myocardial Infarction
- Etiology of Myocardial Infarction
- Classification of Myocardial Infarction
- Pathophysiology of Myocardial Infarction
- Symptoms of Myocardial Infarction
- Diagnostics of Myocardial Infarction
- Pathology of Myocardial Infarction
- Differential Diagnoses of Myocardial Infarction
- Therapy of Myocardial Infarction
- Complications of Myocardial Infarction
- Prevention of Myocardial Infarction
- Review Questions
- References
Image : “CPR training-03” by Rama. License: CC BY-SA 2.0
Definition of Myocardial Infarction
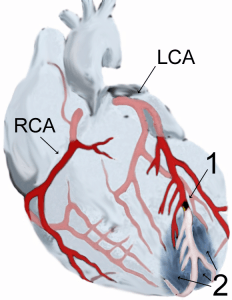
Image: “Myocardial Infarction” by J. Heuser . License: CC BY-SA 3.0
The term myocardial infarction refers to an ischemia of the myocardial tissue due to a complete obstruction or drastic constriction of the coronary artery. This is usually accompanied by an increase in cardiac enzymes, typical ECG changes and pain symptoms, or a thrombus or wall motion abnormality that is detected by means of medical imaging.
Epidemiology of Myocardial Infarction
Spread of myocardial infarction
Myocardial infarction is one of the most common causes of death in industrialized countries. Several million people suffer from myocardial infarction each year.
Regional differences can be observed, with Germany recording a significantly higher number of infarctions per year (300 infarctions/100,000 inhabitants) compared to the Mediterranean countries (100 – 200 infarctions/100,000 inhabitants). Sweden, Belgium and Japan have an even lower infarction rate of less than 100 infarctions/100,000 inhabitants.
Etiology of Myocardial Infarction
Causes of myocardial infarction
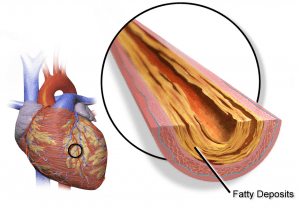
The main cause of myocardial infarction is the development of atherosclerosis in the coronary arteries, hence the name coronary heart disease. Coronary embolism is a more rare cause.
Classification of Myocardial Infarction
Distinction based on the type of myocardial infarction
Image: “Abbreviations used for ACS (Acute coronary syndrome)” by J. Heuser. License: CC BY-SA 3.0
The general distinction is based on ECG changes: STEMI (ST-Segment Elevation Myocardial Infarction) is distinguished from NSTEMI (Non ST-Segment Elevation Myocardial Infarction). Furthermore, the European Society of Cardiology differentiates between the following types:
- Type 1: The infarction is spontaneous and can be attributed to a primary coronary incident.
- Type 2: The infarction is related to ischemia, the cause of the ischemia being by e.g. coronary embolism or anemia
- Type 3: The symptoms preceding cardiac death or an autopsy point to myocardial ischemia.
- Type 4a: The myocardial infarction occurs as part of a PCI.
- Type 4b: The myocardial infarction is caused by a stent thrombosis.
- Type 5: The myocardial infarction develops in connection to a CABG.
Pathophysiology of Myocardial Infarction
How does myocardial infarction happen?
As a result of atherosclerosis, plaques start to form in the coronary arteries, which are at first still stable. Over the course of time, an unstable so-called vulnerable plaque forms. The rupturing of this plaque leads to a thrombotic obstruction of one of the coronary arteries, hypoxia of the tissue fed by the coronary artery, and ischemia, followed by the formation of necroses.
The rupture can be triggered by e.g. physical or psychological stress, drastic blood pressure fluctuations or in the course of circadian rhythms that are accompanied by changes in the coagulation activity (stronger coagulation early in the morning).
Symptoms of Myocardial Infarction
Clinical signs of myocardial infarction
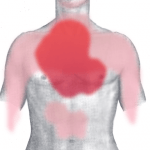
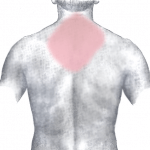
The typical symptoms include severe retrosternal pain that typically radiates into the left arm (Note: right arm pain is possible as well), neck and upper jaw and does not improve after nitroglycerin administration. These symptoms are observed in only about 40 % of patients.
- Image: “Pain in acute myocardial infarction (front)” by J. Heuser . License: CC BY-SA 3.0
- Image: “Pain in acute myocardial infarction (rear)” by J. Heuser. License: CC BY-SA 3.0
Painless infarctions – so-called silent infarctions – especially affect diabetic patients due to neuropathy or old age. These painless infarctions are present in about 20 % of all cases.
However, infarction pain can also be atypical, such as upper abdominal pain, feeling of faintness combined with fear and sweating, dyspnea, nausea or vomiting. These atypical pain symptoms are frequently found in women, diabetics or older people.
Diagnostics of Myocardial Infarction
History and physical exam for myocardial infarction
In the course of the disease, the typical retrosternal pain can be evaluated. A physical exam can reveal e.g. signs of cardiac decompensation or changes in blood pressure. Cardiac risk factors can be ascertained in the process as well or be unveiled during the physical examination.
Noticeable noises, especially in connection with complications, may be detected in the course of the auscultation. A pericardial rub can be heard, which suggests an underlying pericarditis. A systolic murmur occurs during ventricular septal perforation or mitral valve insufficiency. Pulmonary vascular congestion or a lung edema can cause bilateral basal rales.
Lab diagnostics for myocardial infarction
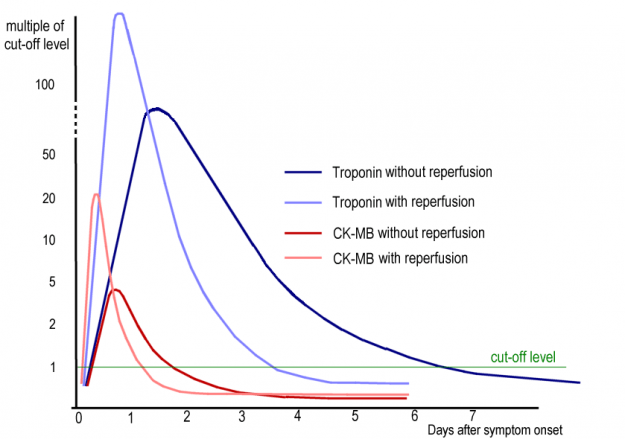
The classification of the heart’s enzymes provides information on the presence and extent of myocardial damage. The determination of Troponin I or T (depending on the lab) is considered the gold standard. Troponin as a cardiac marker is specific to the myocardial tissue.
It increases shortly after the infarction. About 70 % of patients show an increase three hours after the incident, and that number rises to 90 % six hours after the incident. This timeline stresses the necessity to measure cardiac enzymes again at a later time even if the initial result was negative.
Post MI reinfarction cannot be diagnosed by means of troponin-recording, since the troponin concentration only returns to normal after about one to two weeks. In contrast, myoglobin is unspecific and increases also when damage to skeletal muscles occurs, but goes back to normal after one day at the latest. CK-MB is specific to the infarction, but it only starts to rise four hours after the occurrence of ischemia. A CK-MB concentration of between six and twenty percent of the total CK indicates myocardial damage.
LDH can serve as a long-term marker of myocardial damage. It starts to increase only after six to twelve hours, but reaches its maximum after two to four days and stays at an increased level up to two weeks following the infarction. GOT, which is actually a marker for liver cells, also exists in the heart muscle and can be used for diagnostics as well. In that case, GPT, which is specific to the liver, has to be determined as well in order to distinguish heart disease from liver cell damage.
Image: “typical changes in CK-MB and cardiac troponin in Acute Myocardial Infarction” by J. Heuser. License: CC BY-SA 3.0
The following table provides an overview of the various parameters:
ECG diagnostics for myocardial infarction
In the case of non ST-segment elevation myocardial infarction, the ST-segment may be temporarily depressed and may be accompanied by a negative pre-terminal T-wave. The ECG changes of NSTEMI are often atypical, which means that an infarction can only be ruled out through repeated heart enzyme counts.
Image: “ Diagram showing a representation of myocardial infarction on an ECG” by JHeuser. License: CC BY-SA 3.0
In case of an ST-segment elevation myocardial infarction, the ECG shows typical changes, such as the monophasic ST-segment elevation, which transitions directly into the T-wave, with pathologically enlarged Q-spikes. Various other ECG changes are typical depending on the stage of the infarction:
- Initial stage: Up to six hours after the infarction, typically characterized by pointed elevation of the T-wave, which is called anoxic T-wave
- Acute infarction: Few hours up to days after the infarction, characterized by the typical monophasic ST-elevation
- Intermediate stage: The ST-elevation and R-spike decrease, so-called poor R-wave progression occurs, as well as enlargement of the Q-spike, which, as a Pardee-Q, signals the end of the myocardium, and a pointed negativity of the T-wave develops
- Final stage: More than six months after the infarction, the changes of the QRS complex remain, while the ST-segment and the T-wave go back to normal
Localization of infarction
Depending on in which lead of the ECG that changes are detected, this provides information on which coronary artery is likely obstructed and where the infarction is located. In exams, students are often asked to explain the process of how anterior myocardial infarction leads to ECG changes in leads V1-V6, aVL and I.
This frequently affects the proximal part of the anterior interventricular artery. Changes in leads V1 and V2, however, point to a posterior myocardial infarction, where the posterior descending artery is being affected frequently.
Medical imaging for myocardial infarction
Echocardiography as another diagnostic tool helps to detect wall motion abnormalities, determine the remaining function and exclude complications, such as cardiac valvular defects.Cardiac catheterization is considered the gold standard and should be performed as quickly as possible in case of STEMI. MRI cardioangiography serves as another means of detecting wall motion abnormalities and determining the size of infarction scars.
Pathology of Myocardial Infarction
The pathology can be traced back to the insufficient perfusion of cardiac tissue. At a perfusion rate of less than 25 % of the normal blood flow, the tissue is damaged irreversibly, and after six to twelve hours, damages in the shape of yellowish focuses become visible light microscopically.
A complete myocytolysis takes place, the cell nuclei starts to pale and the cross striations get blurred. Granulation tissue with a hemorrhagic edge and numerous peripheral leukocytes develop a few days later. After only two weeks whitish scar tissue develops.
Differential Diagnoses of Myocardial Infarction
Symptoms similar to myocardial infarction
The typical pain symptoms can also point to an unstable angina pectoris, with the exception that there is no increase in troponin. Especially when pain spreads to the upper abdomen, the symptoms can be mistaken for an acute abdomen. Another differential diagnosis to be considered is the Takotsubo-cardiomyopathy, which is often caused by emotional stress.
ECG changes can also be caused by other diseases. ST-elevation can, e.g., also occur in the course of a pericarditis or left ventricular hypertrophy, or low Q-spikes in the course of lung embolisms, the WPW-syndrome or hypertrophic cardiomyopathies.
Furthermore, all other causes of thorax pain have to be distinguished from myocardial infarction, those including lung embolism, aortic dissection, tension pneumothorax and spontaneous rupture of the esophagus (Boerhaave-syndrome). Myocarditis and pericarditis as well as musculo-skeletal thorax pain also count as possible exam answers on the subject.
Therapy of Myocardial Infarction
Treatment of myocardial infarction
Oxygen (4 – 8 l/min per nasal O2 tube) can be administered from the initial treatment until the diagnosis is confirmed. Additionally, it is recommended to elevate the upper body for relief (30º) in the case of dyspnea or heart insufficiency. Administering nitroglycerin (1 capsule or 2 puffs = 0.8 mg, 1 – 5 mg intravenously through a perfusor. Note: contraindicated in case of systolic blood pressure 90 mmHG and simultaneous administration of PDE-5 inhibitors), and morphine (3 – 5 mg intravenously every 5 – 10 minutes) can be administered when severe pain occurs.
Furthermore, all patients receive aspirin (initial dose 150 – 300 mg) as well as heparine (UFH 70 IE/kg KG or NMH) and a P2Y12 inhibitor such as clopidogrel (initial dose 300 mg). Intramuscular injections should be avoided since they lead to an unspecific increase of CK-levels. The administration of beta blockers and ACE-inhibtors respectively AT1 receptor antagonists is also indicated unless there is a contraindication.
A cardiac catheter has to be used for diagnosis in the case of non ST-segment elevation myocardial infarction, which can be performed between 2 to 72 hours after the incident, depending on the risk factors of the respective patient. In the case of ST-segment elevation myocardial infarction, the obstructed coronary vessel has to be revascularized as quickly as possible by means of PCI, because “Time is Muscle“. The primary PCI is the therapy of choice and should be performed within 90 minutes.
Alternatively, a conservative therapy of fibrinolytics and thrombolytics for reperfusion can be performed. The substances used are streptokinase, alteplase, reteplase and tenecteplase, all of which accompany heparin therapy. Alternatively, fondaparinux or enoxaparin may be administered. It is crucial to ensure that no contraindications such as hemorrhages exist and that the STEMI is fresh, in which case an acute PTCA is not possible.
Note, no fibrinolytic treatment with non-St segment elevation MI.
Subsequently, more therapy is necessary to avoid coronary rethrombosis. Dual platelet inhibition is typically employed in this process, and in the case of aspirin it is combined with ticagrelor, prasugrel or clopidogrel. The platelet aggregation inhibition using ASS has to be continued throughout life, whereas the inhibition by means of P2Y12 inhibitors is only used for 12 months following the infarction.
Besides, all patients receive cholesterol-lowering agents, such as statins. The intake of beta blockers decreases the reinfarction risk as well as the risk of arrhythmia related to sudden cardiac death.
Complications of Myocardial Infarction
The complications that come with myocardial infarction are extensive, and their severity depends on the degree of myocardial damage.
One can distinguish between early and late complications, the transition between those phases lying at about 48 hours following the infarction. The early complications include cardiac arrhythmias that develop when an area of the myocardium is under-supplied. Ventricular fibrillation, which accounts for 80 % of deaths due to myocardial infarction, frequently occurs within the first few four hours following the infarction. Premature ventricular contractions or atrial fibrillation can occur as well.
Depending on what area is damaged, right or left heart failure and cardiogenic shock may occur, or damage in the papillary muscle may lead to an insufficiency of the atrioventricular valves. After ventricular fibrillation, congestive heart failure due to cardiac insufficiency is the second most frequent cause of death in patients of myocardial infarction.
The long-term complications include myocardial aneurysms that can rupture. The myocardium may rupture, too. Arterial embolisms, arrhythmias and insufficiencies also count as long-term complications. As a result of the infarction, pericarditis can occur up to six weeks later.
Prevention of Myocardial Infarction
How to prevent myocardial infarction?
Since 95 % of the cases of acute coronary syndrome are manifestations of coronary heart disease, the disease can be prevented. This means that first and foremost the risk factors, especially the main risk factors, which are high cholesterol, arterial hypertension, diabetes mellitus and nicotine abuse must be addressed. Patients themselves should strive to live a healthy lifestyle by paying attention to nutrition and exercise. However, these approaches can be supported with drugs.
Review Questions
The answers are below the references.
1. What does a typical STEMI-ECG look like?
- ST-segment depression with direct transition into a T-wave
- ST-segment elevation with negative preterminal T-wave
- A pointed depression of the T-wave, the so-called anoxic T
- The Pardee-Q, a reduced manifestation of the Q-spike
- A monophasic ST-segment elevation with direct transition into a T-wave
2. The gold standard of lab diagnostics is the determination of
- LDH
- Troponin I/T
- CK-MB
- Myoglobin
- GOT
3. Which medication is contraindicated when administering Sildenafil at the same time?
- ASS
- P2Y12 inhibitors
- Nitroglycerin
- Heparin
- Oxygen



Comentários
Enviar um comentário