Respiratory Physiology: Control and Regulation of Breathing
Table of Contents
- Introduction to Respiratory
- What can be controlled?
- Neural Inputs or Sensors
- Feedback Mechanism
- Effectors
- Respiratory Control Center
- Input to the Inspiratory Center
- Output from the Inspiratory Center
- Expiratory Center
- Apneustic Center
- Pneumotaxic Center
- Chemical Regulation Respiration
- Chemoreceptor
- Stimuli for Central Chemoreceptors
- Function of Central Chemoreceptors
- Peripheral Chemoreceptors
- Stimulus for Peripheral Chemoreceptors
- References
Introduction to Respiratory
A normal adult breathe’s with a respiratory rate less than 25 breaths per minute. The rate of respiration varies with state of the body. It changes with body activity, body temperature, heart status and during various disease processes. Target of the mechanism controlling respiration is to maintain arterial partial pressure of oxygen(Po2) and the partial pressure of carbon dioxide(Pco2) in normal range, even in the state of respiratory distress.
What can be controlled?
- Frequency of breathing
- Depth of breathing maintaining the tidal volume
Neural Inputs or Sensors
- Chemoreceptors
- Central chemoreceptors which are in the Central nervous system i.e in the brain and the spinal cord.
- Peripheral chemoreceptors that are In the carotid artery and the aorta.
- Pulmonary Receptors (Mechanoreceptors) – Receptors in the lungs
- Stretch Receptors which Prevent over-inflation of the lungs.
- Juxta-capillary receptors and Bronchial C fibers – These sense chemicals, stretch and pulmonary edema and respond by producing shallow breathing and producing mucous secretion.
- Joint and muscle receptors responsible for chest wall position and muscle tension.
- Irritant Receptors: These sense the presence of dust, chemicals and cold air and respond by producing cough reflex and/or bronchoconstriction.
Chemoreceptors in the CNS sense the changes in H+ ion concentration while the peripheral chemoreceptors sense the changes in the Po2 and Pco2 in the blood as well as the H+ ions concentration.
Pulmonary receptors are present in the visceral pleura surrounding the lungs and in the lung parenchyma. These receptors sense the stretch in the lungs produced when the lungs expand.
Feedback Mechanism
Stimuli from the chemoreceptor, pulmonary receptors and receptors in the joints and muscles around the chest stimulate the respiratory control center which in return commands the effectors to produce the desired effects.
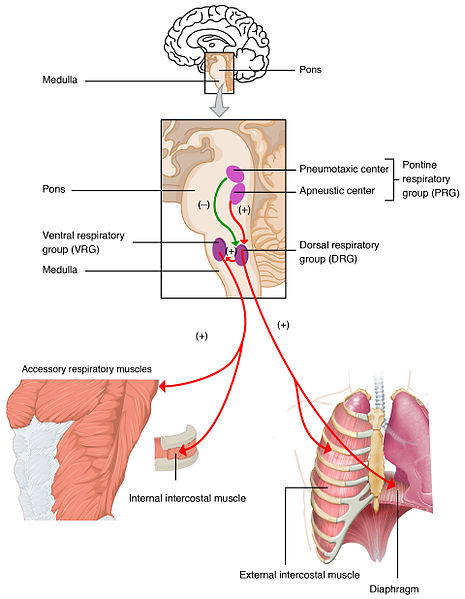
Effectors
These are the muscles and related tissues which are controlled by the CNS to regulate the respiratory effort. These maintain the respiratory activity as ordered by the brain through the respiratory control center. Effectors include diaphragm and the respiratory muscles (external and internal intercostal muscles; accessory muscles and abdominal muscles). Inspiration is controlled by the external intercostal muscles and the accessory muscles. Expiration is controlled by the internal intercostal and the abdominal muscles.
Respiratory Control Center
The respiratory center in the CNS lies in the brainstem in the pons and medulla. Effectors are signaled by the neurons in the medulla. These centres control the automatic, unconscious breathing activity. The motor cortex of the cerebrum has the voluntary control.
The control centers in the brainstem include the following:
- The apneustic center
- The pneumotaxic center
- Medullary Respiratory Centers (in the reticular formation of the brain)
- Ventral respiratory group of nuclei
- Dorsal respiratory group of nuclei
“Respiratory Control Center. Engineering Control System Approach” Image created by Lecturio
Input to the Inspiratory Center
Sensory fibers from the peripheral chemoreceptor reach the respiratory centers through the glossopharyngeal nerve and the vagus nerve and from the mechanoreceptor in the lungs through the vagus nerve.
Stretch receptors in the lungs send signals through vagus nerve. Pco2 receptors in the bone-dura arachnoid matter in the CSF space also send signals through IX and X cranial nerves.
Output from the Inspiratory Center
Output or efferent fibers through the spinal cord synapse on the lower motor neuron in the cervical and thoracic region and through the phrenic nerve signal the diaphragm and through intercostal nerves signal the intercostal muscles. Contraction of these muscles produces the inspiratory activity.
Inspiration usually lasts for 2 seconds which is followed by the expiration, in which relaxation of the inspiratory muscles and contraction of the expiratory muscles occur leading to expiration.
Expiratory Center
The center for expiration lies in the ventral respiratory neurons in the medulla. These neurons are not fully active during quiet breathing. They are activated during exercise or in conditions when more gas exchange is required.
Apneustic Center
Location: It is located in the reticular formation in the lower pons.
Function: This center is responsible for the coordination between inhalation and exhalation. It specifically facilitates in the process of inspiration. This center sends signals to the dorsal respiratory group of neurons to prevent the switch off inspiratory ramp signals. It is responsible for deeper and longer inspiration. On stimulation, the duration of inspiration is increased resulting in deeper and prolonged inspiratory effort.
Pneumotaxic Center
Pneumotaxic Center is located in the upper pons. On its activation, it sends inhibitory impulses to the inspiratory area and turn off inspiration. It helps in limiting action potentials in the phrenic nerve in order to control the function of the diaphragm. As a result it limits the size of tidal volume and regulates the respiratory rate. If strong signals are produced, the rate of breathing is increased to 30 – 40 breaths /min and weak signals reduce the rate to few breaths /min.
Chemical Regulation Respiration
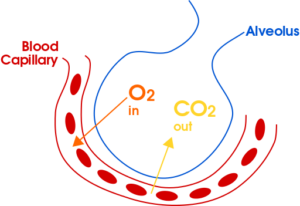
The respiratory system functions to maintain proper levels of CO2 and O2 and is very responsive to changes in the levels of these gases in body fluids.
Chemoreceptor
Sensory neurons responsive to chemicals, monitor levels of CO2, H+ and O2 and provide input to the respiratory center which adjusts pulmonary ventilation to keep these variables within the homeostatic limit.
“Central Chemoreceptor. Primary Sensor in Basal Conditions” Image created by Lecturio
Stimuli for Central Chemoreceptors
Main function of the central chemoreceptors is to keep arterial PCO2. Within limits. CO2 is not the main stimulus for the central chemoreceptors; instead H+ ions in CSF is the main stimulus. CO2 in blood passes through brain barrier and forms carbonic acid in CSF which disassociate into H and HCO3 ion. This H ion stimulates the respiratory center.
Function of Central Chemoreceptors
Main function is to maintain PCO2 in the brain and the CSF. H+ generated maintains the pH of the CSF and stimulates the respiratory center causing an increase in the breathing rate. Rise in respiratory rate leads to washing out of more CO2, PCO2 falls to normal.
Peripheral Chemoreceptors
These are located at the carotid bifurcation in the carotid body and in the arch of aorta in the aortic bodies. Sometimes they may also be present in thoracic and abdominal region along major arteries. These receptors detect changes in arterial O2, along with changes in CO2 and pH. Signals from these receptors are transmitted to respiratory centers in order to regulate respiratory activity. Each chemoreceptor receives special blood supply.
Stimulus for Peripheral Chemoreceptors
- Decrease in arterial Po2: Any decrease in arterial PO2 is detected by these receptors. They relatively respond to decrease in Po2 to less than 60mmHg. When PO2 of 100 to 60mmhg, rate remains almost constant; but, if arterial po2 falls below 60mmhg, respiratory rate increases slowly.
- Increase in arterial pco2: These receptors also detect increase in PCO2 but it is lesser effect. Changes in PCO2 is detected and responded properly by the central chemoreceptors.
- Decrease in arterial pH: A fall in the arterial pH leads to an increase in ventilation, mediated by peripheral chemoreceptor after sensing an increase in the H+ ions in the arterial blood. Only chemoreceptors of the carotid bodies respond to this change; not the aortic bodies.
“Peripheral Chemoreceptors. Representative Glomus Cell Stimulus/Response” Image created by Lecturio
In conditions like metabolic acidosis, decreased arterial pH stimulates the peripheral chemoreceptors directly and increase the respiratory rate. This is called the Kausmaal breathing.

Comentários
Enviar um comentário