Sinusitis (Sinus Infection) in Children — Definition and Symptoms
Table of Contents
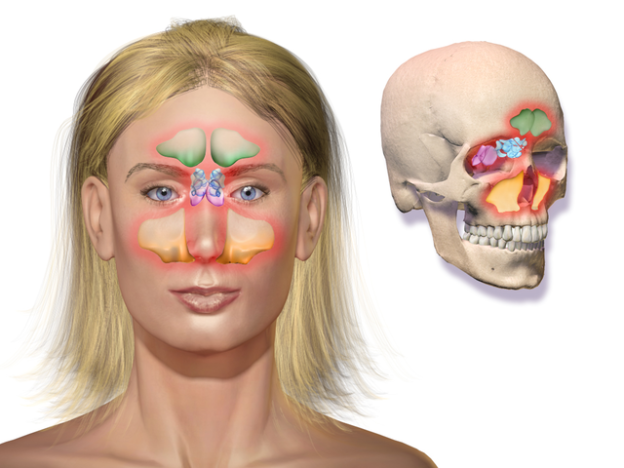
Image: “Sinusitis.” by Blausen.com staff (2014). “Medical gallery of Blausen Medical 2014”. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. – Own work. License: CC BY 3.0
Overview
Acute sinusitis in children can be defined as the acute inflammation of the mucosa of the paranasal sinuses or the nasal passages with a duration of less than 4 weeks. This inflammatory condition can be caused by viral infections, bacteria or fungi. Non-infectious etiologies of acute sinusitis can be allergies or irritants.
Epidemiology of Sinusitis in Children
Upper respiratory tract infections are very common in children with an estimated incidence of 6 episodes per patient-year. Approximately, 8 % of these upper respiratory tract infection episodes are complicated by rhinosinusitis in children aged between 6 and 35 months of age.
There are no differences in the incidence of rhinosinusitis among boys and girls, but the condition is becoming more common in both sexes within the last decade.
Children, who are born with genetic disorders that impair mucosal ciliary movement, or who have impaired secretory immune response, are predisposed to recurrent rhinosinusitis episodes.
Etiology and Pathophysiology of Sinusitis
The most common etiology of rhinosinusitis in children is viral in origin. Secondary bacterial infections of the sinuses are a common complication in children. Streptococcus pneumoniae, Moraxella catarrhalis, staphylococcus aureus and nontypeable Haemophilus influenzae are the most commonly identified bacterial etiologies of bacterial rhinosinusitis in children.
For bacteria to colonize the nasal and paranasal sinuses and cause symptoms in children, certain pathological changes must happen first within the nasal and paranasal passages.
The most important pathophysiological change encountered is the obstruction of the sinus drainage pathways. A common cause of obstructed sinus drainage pathways in children is otitis media. The normal metachronous movement of mucous towards the natural ostia of the sinuses is disrupted by mucosal inflammation.
Additionally, children with recurrent bacterial rhinosinusitis usually have some evidence of ciliary impairment and altered mucus quantity or quality. The most common causes of altered mucus quantity and quality in children include asthma and other allergic conditions.
Viral upper respiratory tract infections can also alter the composition and quantity of the mucus within the nasal and paranasal sinuses, which can put the child at an increased risk of acquiring a secondary bacterial infection.
Clinical Presentation of Sinusitis in Children
When a child presents with symptoms and signs suggestive of an upper respiratory tract infection, one should pay attention to the severity of the symptoms and the possibility of the presence of a complicating rhinosinusitis.
Most common colds have a runny nose with mucus and improve by 10 days. Sometimes, colds also include fever for 1 to 2 days; however, for acute bacterial sinusitis, the pattern of illness is persistent, severe, or worsening.
- Persistent sinusitis (common) includes nasal discharge (any quality), daytime cough (which may be worse at night), or both for at least 10 days without improvement.
- Severe sinusitis: It occurs when there is concurrent fever with purulent thick nasal mucus discharge that is thick, colored, or cloudy for at least 3 consecutive days, with more severe facial pain and headache.
- Worsening sinusitis: It starts with a viral cold but later worsens with bacterial infection and there is a new onset of nasal discharge, a daytime cough, or a high-grade fever after initial improvement.
Differentiate of viral sinusitis from bacterial sinusitis
Almost all children with viral upper respiratory tract infections have rhinosinusitis; therefore, we will focus on differentiating bacterial from viral sinusitis. This distinction is important because viral rhinosinusitis resolves spontaneously, while bacterial rhinosinusitis in children requires specific antimicrobial therapy.
Diagnosis of acute bacterial sinusitis
The diagnosis of acute bacterial sinusitis is made when the child has two major criteria or one major criterion and two or more minor criteria from the clinical diagnostic criteria of bacterial sinusitis in children.
The major criteria include the:
- Presence of facial pain, facial congestion
- Nasal congestion, nasal discharge which can be purulent
- Loss of the sense of smell
- Presence of purulent discharge on intranasal examination and, finally, the presence of fever
The minor criteria for the diagnosis of acute bacterial sinusitis in children include the presence of:
- Headache
- Halitosis
- Fatigue
- Dental pain
- Cough and ear pain
Once the diagnosis of acute sinusitis is suspected in a child, the treating physician should look for any clues that point towards a possible bacterial etiology rather than a viral one. The most crucial differences between bacterial and viral acute sinusitis in children in favor of bacterial sinusitis are the duration of respiratory symptoms of more than 10 days, the presence of purulent nasal discharge and a high-grade fever, and worsening of the symptoms after an initial temporary improvement.
Diagnostic Workup for Sinusitis in Children
Proper history taking and a physical examination is required in a child who presents with upper respiratory tract infection symptoms to differentiate between viral and bacterial etiologies. Patients with suspected acute bacterial sinusitis should be offered advanced confirmatory tests whenever possible before starting antibiotic therapy.
Laboratory investigations are usually not helpful in children with acute sinusitis as leukocytosis is rarely seen. Children with severe acute bacterial rhinosinusitis who are ill and toxic might have leukocytosis and neutrophilia.
- Culture and sensitivity test: The best diagnostic test to confirm the diagnosis of bacterial sinusitis in children is a culture and sensitivity test from the paranasal sinus cavity. The presence of more than 104 colony-forming units/mL on bacterial culture is confirmatory of bacterial sinusitis in children.
- Sinus aspiration is rarely used in children because it is considered as too invasive, painful and impractical. Endoscopic-guided middle meatus cultures can provide sinus aspirates to confirm the diagnosis of acute bacterial rhinosinusitis, but their validity has not been tested in children.
- Imaging studies can provide more clues towards the diagnosis of acute sinusitis in children, but they have several drawbacks. First, computed tomography studies might show sinus abnormalities even in healthy children. Second, skull X-rays and computed tomography scans cannot differentiate between viral and bacterial sinusitis. Third, imaging studies of the sinuses in children with viral upper respiratory tract infections can show sinus abnormalities in more than 80% of the cases without any clinical symptoms and signs suggestive of sinusitis.
Because of these reasons, imaging studies in children should be reserved only for complicated and recurrent cases.
Imaging studies are more useful in excluding the diagnosis of acute sinusitis rather than confirming it. A negative computed tomography scan is very reliable in excluding acute sinusitis as the cause behind headache and facial pain in a child.
Magnetic resonance imaging studies of the brain are useful in excluding complications of acute bacterial sinusitis such as brain abscess and cerebrovascular venous thrombosis.
Treatment of Sinusitis in Children
Once the diagnosis of acute bacterial rhinosinusitis in a child is made, empirical antibiotic therapy should be started. Additionally, symptomatic treatment of nasal and sinus congestion is indicated to decrease the severity and duration of the symptoms.
Antibiotics therapy
Amoxicillin as first-line treatment
The antibiotic of choice for acute bacterial sinusitis in children is amoxicillin-clavulanate. The dosage of amoxicillin-clavulanate is usually dependent on the severity of the bacterial sinusitis. Children with non-severe sinusitis usually receive a standard dose defined as 45 mg/kg/d orally 3 times a day. High-dose amoxicillin-clavulanate is defined as 90 mg/kg/d orally twice a day and should be reserved for children with severe bacterial sinusitis.
Ceftriaxone (a substitute for oral antibiotics): Children who are unable to tolerate oral medication should be given a single dose of ceftriaxone 50-mg/kg/d intravenously or intramuscularly.
Patients with penicillin allergy
If the diagnosis of penicillin-resistant Streptococcus pneumoniae sinusitis is suspected, young children allergic to amoxicillin with a serious type 1 hypersensitivity to penicillin can be treated with a combination of clindamycin (or linezolid) and cefixime. Linezolid is excellent againstpneumoniae, but lacks activity against H influenzae and M catarrhalis. Levofloxacin, which has a high level of activity against both S. pneumoniae and H. influenzae, may be prescribed instead of amoxicillin-clavulanate and linezolid. Children with delayed hypersensitivity reaction to penicillin can also receive cefixime plus clindamycin.
In contrast to adults, short-term antibiotic therapy is not recommended in children. Instead, 10 days up to two weeks of empirical antibiotic therapy is recommended. Children usually show significant improvement of their symptoms within 5 days from the initiation of antibiotic therapy.
Adjuvant Therapy
Adjuvant therapy for acute sinusitis might include intranasal corticosteroids, saline nasal irrigation or lavage, topical or oral decongestants, mucolytics, and topical or oral antihistamines.
Intranasal corticosteroids have showed objective clinical improvement in children with acute bacterial sinusitis and are recommended as an adjunctive therapy.
Saline nasal irrigation or lavage (not saline nasal spray) has been used to remove debris from the nasal cavity and temporarily reduce tissue edema to promote drainage from the sinuses.
Topical or oral decongestants, mucolytics, and topical or oral antihistamines. These are not generally recommended for acute bacterial sinusitis in children. Antihistamine therapy is useful in reducing typical allergic symptoms in children with atopy who also have acute sinusitis. Adequate hydration and mucolytic agents might be useful in children with acute bacterial rhinosinusitis as they facilitate sinus drainage and can achieve symptomatic relief.
Surgical drainage
Children who fail to respond to medical therapy or who have too often recurrences should be offered surgical drainage of their sinuses. Surgical approaches include the following:
- Adenoidectomy
- Functional endoscopic sinus surgery
- Uncinate removal, anterior ethmoidectomy, and maxillary antrostomy – the most common forms of surgery
- Balloon sinuplasty
Functional endoscopic sinus surgery is the best therapeutic option and has been shown to achieve success in about 75% of the cases of complicated, persistent bacterial sinusitis.
Comentários
Enviar um comentário