Abnormal Uterine Bleeding and Endometrial Polyp — Symptoms and Diagnosis
Table of Contents
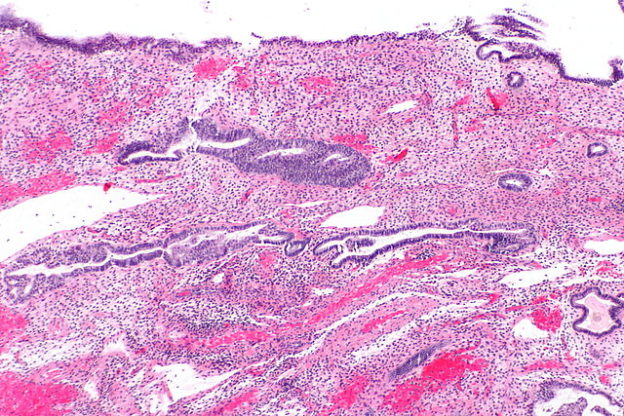
Image: “Histological image of endometrial polyp with fused glands.” by Nephron – Own work. License: CC BY-SA 3.0
Dysfunctional Uterine Bleeding
Abnormal uterine bleeding (AUB) is a frequent, distressing diagnosis. About 20% of females have excessive menstrual blood loss. These menstrual disorders have increasingly become relevant due to the alleged modernization of the female reproductive cycle with late conception, fewer conceptions, shortened breastfeeding and increased rates of sterilization.
DUB is a diagnosis of exclusion once all primary etiologies are ruled out.
The PALM-COEIN (FIGO) classification comprises of nine important etiological categories for AUB. They are Polyp, Adenomyosis, Leiomyoma, Malignancy and hyperplasia, Coagulopathy, Ovulatory dysfunction, Endometrial dysfunction, Iatrogenic, Not yet classified.
DUB as a terminology is abandoned in this classification.
Treatment of Abnormal Uterine Bleeding
Medical treatment
- Non-steroidal anti-inflammatory drugs
- Oral contraceptive pills
- Progestins
- GnRH (gonadal releasing hormone)
- Antifibrinolytic medications
- Danazol (synthetic androgen)
Surgical treatment
- Endometrial ablation
- Hysterectomy
- Thermal balloon ablation
We now focus on a few significant causes of AUB.
Endometrial Polyp
Frequently associated with abnormal uterine bleeding, endometrial polyps are characterized by benign finger-like projections of the endometrium. These are usually encountered in females younger than 40 years.
Image: “Histological image of endometrial polyp with fused glands.” by Nephron – Own work. License: CC BY-SA 3.0
Epidemiology
Accounting for about 25% of abnormal uterine bleeding, EPs occur in about 10% of women in reproductive age.
Classification
Also known as uterine polyps, they may be sessileor pedunculated. The latter is more common. The most frequent location is the uterine fundus.
Morphological classification of the endometrial polyps segregates them into following types:
Hyperplastic EP: originate from the basal endometrium layer which response only to estrogen stimulation.
Functional EP: the glandular component of these EPs responds to cyclic hormonal changes of the menstrual period and resembles the surrounding endometrium. This is also the fundamental reason behind the difficulty in diagnosis of these EPs by curettage secondary to tissue fragmentation during the same.
Atrophic EP demonstrated in the post-menopausal period represents the fibrotic transition of the stroma. Fibrosis culminates in incomplete removal by curettage.
Pathophysiology
The exact cause of endometrial polyps is still elusive. Hormonal factors are implicated. Supportive evidence is provided by the presence of endometrial polyps in postmenopausal women on tamoxifen.
Tamoxifen has partial estrogen agonist action, which potentially brings about endometrial abnormalities. Other situations associated with increased prevalence of EP include hormone replacement therapy, obesity, hypertension and history of cervical polyps.
Use of levonorgestrel IUD (Intrauterine device) potentially ameliorates the risk of EP.
Symptoms
Menstrual disorders are seen in about 82% of premenopausal women. Postmenopausal uterine bleeding is seen in postmenopausal women. EPs protruding through the cervix can cause dysmenorrhea. EPs remain asymptomatic in a small group of patients. The following table gives a rough estimate of the varied presentation forms of EP:
Special Forms
Multiple EPs are encountered in about 26 % of postmenopausal and 15 % of premenopausal patients.
Pathology
On gross examination, endometrial polyps appear of the same color as the surrounding endometrium. Microscopic examination reveals dense, fibrous stroma with glandular spacesand blood vessels lined by endometrial epithelium.
While the more common pedunculated polyps are connected to a pedicle, sessile polyps have a flushed attachment to the basal stroma.
Diagnosis
Dilatation and curettage has been the standard diagnostic methodology for EPs for many years. However, it has many limiting factors.
Evidence suggests hysteroscopy to be the optimal diagnostic tool for examination of the uterine cavity and subsequent focused treatment of EP. Transvaginal ultrasonography forms sufficient preliminary investigations for diagnosis of EP. Administration of intrauterine contrast elevates the sensitivity of the test.
Hysteroscopic polypectomy is considered the gold standard in the treatment of EP. It is now deemed essential to remove the endometrial basalis around the origin of EP to evade recurrence.
Therapy
Various treatment options can be compared as follows:
Prognosis
Small EPs managed conservatively are known to undergo spontaneous regression. Most of the EPs have an inconsequential course. Notwithstanding the benign nature of the majority of the endometrial polyps, about 0.5 % of polyps are proved to harbor malignant adenocarcinoma cells.
Evidence for the role of endometrial polyps in infertility and improvement after treatment of EP is equivocal.
Leiomyoma
Leiomyoma stands for smooth muscle tumor. The most common locations for the origin of leiomyomas are uterus, esophagus and small intestine.
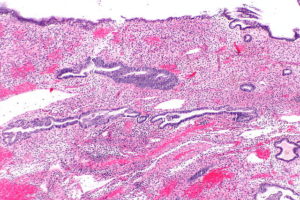
Image: “Histopathology of uterine leiomyoma.” by KGH. License: CC BY-SA 3.0
Also known variously as fibroid, myoma, fibromyoma, leiomyomas are typically benign. As a paradox to their benign nature, leiomyomas are potentially distressing to the female population of reproductive age. Being the most common tumors in women in this subset, they are responsible for the majority of patients with abnormal uterine bleeding.
Epidemiology
Leiomyomas are the commonest tumors in women with the prevalence of one in every four to five women. The highest incidence is in the fifth decade.
Classification
Taking into account the Wamsteker et al. classification, the following integrated classification is now adapted:
- Type 1: intracavitary leiomyomas with narrow attachment to the endometrium
- Type 2: less than 50% of the leiomyoma is intramural
- Type 3: at least 50% is intramural
- Type 4: completely extracavitary, but about the endometrium
- Type 5: intramural leiomyomas contained in entirety in the myometrium
- Type 6: subserosal leiomyomas which are less than 50% intramural
- Type 7: leiomyomas with a narrow stalk-like attachment to the serosa
- Type 8: leiomyomas unrelated to the myometrium; cervical lesions, “parasitic lesions”, lesions in the broad ligament
Types 0-2 are submucosal, while 2-5 are also termed as hybrid leiomyomas.
A simpler classification often followed is:
- Intramural leiomyomas: most common
- Submucosal leiomyomas: most often responsible for menorrhagia, infertility, and miscarriages
- Subserosal leiomyomas
Few other terms need to be mentioned:
- Parasitic leiomyomas: leiomyomas which are pedunculated, to begin with, but seek blood supply from surrounding tissues such as omentum and other pelvic structures and subsequently get disconnected from the uterus.
- Familial leiomyoma: with a defect in the fumarate hydratase gene on chromosome 1 it is associated with renal cell carcinoma.
- Fibromyoma of the breast: infrequent breast tumor; in women with a history of hysterectomy for leiomyomas
- Uterine lipoleiomyoma: contain simultaneous conglomerates of adipocytes and smooth muscle cells. Often benign, they are known to transform into liposarcomas.
- Paraneoplastic polycythemia: unregulated production of erythropoietin by some fibroids leads to polycythemia.
- Angioleiomyoma: vascular leiomyomas
- Piloleiomyomas: cutaneous leiomyomas
- Metastatic leiomyoma: metastases to lung and pelvis after surgical extirpation of uterine fibroids is a rare but well-described entity in literature.
- Red degeneration: characterized by acute onset of severe pain and abdominal tenderness, red degeneration most likely represents the accumulation of blood in the tumor secondary to venous obstruction. It is commonly looked upon as a complication of pregnancy.
Symptoms
Following symptoms are commonly witnessed in patients with leiomyomas:
Image: “CT image of uterine fibroid (leiomyoma).” by Rádiológ My own work – CT – Somatom Sensation Open 40. License: CC BY-SA 3.0
- Anemia
- Infertility
- Menorrhagia (excessive blood loss)
- Malignant transformation
- Abnormal menstrual bleeding
- Bladder compression.
Rare sequels include:
- Ascites
- Benign metastasizing leiomyoma
- Disseminated peritoneal leiomyomatosis
- Intravenous leiomyomatosis
- Leiomyosarcoma
Pathogenesis
Leiomyomas are estrogen-responsive neoplasms. In concert with the estrogen levels, they increase during pregnancy and often regress after menopause. Chromosome 12 abnormalities are implicated in the majority of leiomyomas.
Pathology
Leiomyomas on gross examination appear to be grayish-white, well defined, circumscribed, multi-nodular masses protruding into the endometrial cavity and compressing the same. The cut surface has a whorled appearance due to intersecting muscle fibers and white fibrous tissue.
Hemorrhage, cystic degeneration and calcification can often be appreciated. Often resembling the normal myometrium, the tumor cells are spindle-shaped, elongated with a cigar-shaped nucleus.
Diagnosis
Leiomyomas are diagnosed with pelvic ultrasonography. Doppler studies may be indicated to assess the vascularity of the tumor. Some advocate biopsy to establish the tissue diagnosis.
Treatment
Various treatment modalities available and the rationale for the specific use of each of them can be summarized as follows:
Masterly inactivity: advocated in patients nearing menopause with manageable symptoms. Repeat assessment after 6 months is the norm.
Medical management:
- NSAIDs for pain, dysmenorrhea
- Iron supplementation for anemia secondary to blood loss
- Oral contraceptives and progesterone: equivocal benefit in treating dysmenorrhea and menorrhagia.
- GnRH analogs: reduce the size of the myomas by about 50 %
- Gestrinone and RU-486: experimental drugs.
Surgical treatment:
- Hysterectomy: gold standard for complete removal. Laparoscopic hysterectomy or laparoscopically assisted vaginal hysterectomy can be performed. Laparoscopic supracervical hysterectomy is for patients who are unwilling for laparotomy. Good pelvic support is a pre-requisite in these patients.
- Hysteroscopic transcervical resection mainly for submucosal myomas
- Myomectomy: viable option for those who are keen to preserve their reproductive ability. Laparoscopic myomectomy is also feasible.
- Embolization
- Myolysis by electrodesiccation or cryotherapy.
Leiomyosarcoma
Leiomyosarcomas are malignant smooth muscle cell sarcomas. They are most prevalent in the uterus, stomach, small bowel and are also encountered in the retroperitoneum.
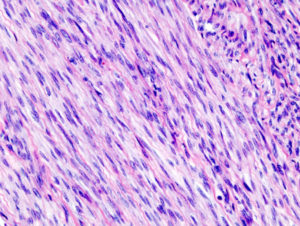
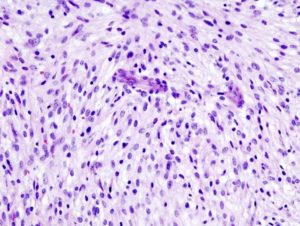
Image: “Histopathology of uterine leiomyosarcoma.” by KGH. License: CC BY-SA 3.0
Leiomyosarcomas comprise 2 to 5 % of all uterine malignancies. These malignant smooth muscle cell sarcomas with frank invasion into the uterine wall have the highest prevalence in peri-menopausal women, from 40-60 years of age.
Prior pelvic radiation is a proven risk factor. Evidence against the use of tamoxifen as a risk factor is inconclusive. Similarly, parity and time of menarche and menopause as contributory factors have equivocal evidence.
Earlier presumptions about the malignant transformation of leiomyoma into leiomyosarcoma have almost been demolished. Being the most common of the uterine sarcomas, the majority of the leiomyosarcomas originate de novo.
Pathology
Leiomyosarcomas on gross examination are usually large, fleshy with hemorrhage and necrosis. On microscopic examination, the presence of atypical cells, pleomorphism, frequent mitoses and coagulative necrosis sets them apart from the benign leiomyomas.
Symptoms
Vaginal bleeding is the most common presentation.
Diagnosis
No imaging study, unfortunately, is sensitive and specific enough to distinguish leiomyosarcoma from the benign leiomyomas. Histologic examination of the entire uterus is definitive.
Staging
Based on FIGO staging, simplified staging for leiomyosarcoma is as follows:
- Stage 1: limited to the corpus
- Stage 2: confined to the corpus and cervix
- Stage 3: spread outside the uterus, but confined to the pelvis
- Stage 4: spread outside the true pelvis.
Therapy
Radical generous surgical extirpation when feasible is the only practical treatment which is potentially curing if managed when the sarcoma is small and confined to the uterus.
Leiomyosarcoma is traditionally not chemo- and radiosensitive and hence use of adjuvant therapy is rather experimental. There is naive evidence that adjuvant radiation leads to 62 % 5-year survival as compared to 46 % with surgery alone.
Doxorubicin holds a promising future in the treatment of advanced leiomyosarcoma.
Presence of hormone receptors has led to hormone therapy trial in leiomyosarcoma. It is rather unfortunate that the sole presence of the receptors alone does not proportionately predict hormone responsiveness.
Prognosis
The overall prognosis of leiomyosarcoma is rather dismal. While the 5-year survival of stage I disease barely reaches 50 %, the cumulative 5-year survival for the other stages is abysmally low, about 20 %.
Leiomyosarcomas greater than 5 cm in women more than 50 years of age have consistently poor outcome.
Summary
Abnormal uterine bleeding is a nightmare for many women. Primary uterine neoplasms responsible for AUB are endometrial polyps, leiomyomas and rarely leiomyosarcomas. Dysfunctional uterine bleeding is a diagnosis of exclusion.
Endometrial polyps are benign finger-like projections of the endometrium which often lead to menstrual disturbances. Hysteroscopic polypectomy is the gold standard treatment.
Leiomyomas are benign smooth muscle cell neoplasms with origin usually in the uterine myometrium. They are inculpated for varied presentations such as abnormal bleeding, infertility, dysmenorrheal and urinary disturbances. While surgical excision is the definitive treatment, the medical line of management exists to ameliorate the symptoms.
Leiomyosarcomas are rare uterine smooth muscle cell sarcomas with poor prognosis. Radical surgical extirpation when feasible is curative.
Review Questions
The correct answers can be found below the references.
1. Which of the statements is false regarding endometrial polyps?
- Endometrial polyps are benign projections of myometrium into the endometrium.
- Endometrial polyps cause abnormal uterine bleeding.
- Expectant treatment can be considered for small, asymptomatic polyps.
- Hysteroscopic polypectomy is the optimal therapy.
2. Which of the following statements is true regarding leiomyomas?
- Leiomyomas often transform into leiomyosarcomas.
- Leiomyomas are rare uterine tumors.
- Most of the leiomyomas are asymptomatic.
- Intramural leiomyomas are most common.
3. Which is the best treatment modality for leiomyosarcomas?
- Chemoradiation
- Radiation
- Surgical excision
- Hormonal therapy

I want to share with you all on how Dr Itua saves my life with his powerful Herbal medicines, I was diagnosed of Oral/Ovarian Cancer which i suffered from for 5 years with no positive treatment until when My son came to me in the hospital when i was laying down on my dying bed waiting for god to call out my name to join him in heaven.
ResponderEliminarMy son was so excited that very day he came across Dr Itua on Blogspot, we decided to give him a try although we Americans are so scared to trust Africans but i really have no choice that time to choose life in between so we gave a try to Dr Itua Herbal medicines, god wiling he was a good man with a god gift. Dr Itua send us the herbal medicine it was three bottles. I take it for three weeks instructor and this herbal medicines heal me, cure my Oral/Ovarian Cancer completely I have been living for 9 months now with healthy life no more symptoms.
I'm sponsoring Dr Itua in LA Advert on Cancer patent seminar which my son will be participating too and other patent Dr Itua has cured from all kind of human disease, also if you are sick from disease like,Epilepsy,Breast Cancer,Prostate Cancer,Throat cancer,Thyroid Cancer,Uterine cancer,Fibroid,Angiopathy, Ataxia,Arthritis,Brain cancer,Hiv,. Vaginal cancer,Herpes,Colon-Rectal Cancer,Chronic Disease.Amyotrophic Lateral Scoliosis,Brain Tumor,Fibromyalgia,Fluoroquinolone Toxicity,Multiple myeloma,Tach Diseases,Leukemia,Liver cancer,
Esophageal cancer,Gallbladder cancer,,Bladder cancer,Gestational trophoblastic disease,Head and neck cancer,Hodgkin lymphoma
Intestinal cancer,Kidney cancer,Hpv,Lung cancer,Adrenal cancer.Bile duct cancer,Bone cancer,Melanoma,Mesothelioma,Neuroendocrine tumors
Non-Hodgkin lymphoma,Cervical Cancer,Oral cancer,Hepatitis,Skin cancer,Soft tissue sarcoma,Spinal cancer,Pancreatic Cancer, Stomach cancer
Testicular cancer,
Syndrome Fibrodysplasia Ossificans ProgresSclerosis,Alzheimer's disease,Chronic Diarrhea,Copd,Parkinson,Als,Adrenocortical carcinoma Infectious mononucleosis,Vulvar cancer,Ovarian cancer,,Sinus cancer, Here Is The Wonderful Healer Contact. Name_ Doctor Itua, Email Contact: drituaherbalcenter@gmail.com, Phone/WhatsApp: +2348149277967