Vasospastic Angina (Prinzmetal Angina) — Definition and Treatment
Table of Contents
- Definition of Vasospastic Angina
- Epidemiology of Vasospastic Angina
- Etiology of Vasospastic Angina
- Risk Factors and Associations of Vasospastic Angina
- Pathology and Pathophysiology of Vasospastic Angina
- Clinical Presentation and Diagnosis of Vasospastic Angina
- Major Clinical Complications of Vasospastic Angina
- Differential Diagnosis of Vasospastic Angina
- Treatment and Management of Vasospastic Angina
- Progression and Prognosis of Vasospastic Angina
- Review Questions
- References
Definition of Vasospastic Angina
A sudden coronary artery spasm is leading to a reduction in coronary blood flow, thus causing severe chest pain (angina) at rest, is called vasospastic, Prinzmetal or variant angina. This type of angina occurs at rest, rather than on exertion without any initiating factors.
Usually, a cardiovascular event is associated with atherosclerosis of a major coronary artery but, in this case, the causative mechanism is ‘vasospasm’ which may or may not occur at the site of atherosclerosis. Multifocal spasms can also occur in the coronary system. An ECG at the time of the chest pain due to vasospastic angina may show ST segment elevation.
Epidemiology of Vasospastic Angina
Spread of vasospastic angina
Vasospastic angina is an uncommon cause of myocardial ischemia, responsible for approximately 5% of angina cases. Patients are generally younger than those with stable or unstable angina secondary to coronary artery atherosclerosis. Variant angina more commonly affects women.
This syndrome has a higher incidence in Japan, compared to Western countries. The overall incidence has decreased significantly over the past thirty years. It is believed that this decline is because of increased use of calcium antagonists to treat hypertension.
Etiology of Vasospastic Angina
Causes of vasospastic angina
Vasospastic angina is caused by spasm of the coronary arteries, which are the arteries supplying the heart. Coronary artery spasm can occur as a result of various risk factors, such as stress, smoking, cocaine use, insulin resistance and medications that have the effect of constricting blood vessels, such as triptans.
Rarely, coronary artery vasospasm may be triggered after coronary artery bypass surgery or near a drug-eluting stent. Generally, the specific trigger is unknown. Many patients don’t usually display the classical coronary risk factors, apart from heavy smoking.
Risk Factors and Associations of Vasospastic Angina
Risk factors of vasospastic angina
- Smoking
- Substance abuse
- Alcohol
- Cocaine
- Sumatriptan
- 5-fluoro-uracil
- Insulin resistance
Associations
Rarely, variant angina is associated with systemic vasomotor disorders such as a migraine and Raynaud’s phenomenon. This suggests the presence of a general vascular disorder.
Pathology and Pathophysiology of Vasospastic Angina
The underlying mechanism causing vasospasm in vasospastic angina is debateable, and many theories have been put forward in recent years. Vasospasm occurs in response to local vasoconstrictor stimuli in the coronary segment. Impaired regulation of myofibril contraction in smooth muscle cells of coronary vessels causes smooth muscle hyperactivity, resulting in vasospasm.
Other abnormalities of the endothelium, such as defects in an enzyme, endothelial nitric oxide synthetase, can lead to reduced levels of nitric oxide. Nitric oxide is a natural vasodilator, and its decreased synthesis can lead to vasoconstriction. Current studies also show that coronary artery vasospasm can result from impairment of K+ ATP-dependent channels and hyperactivity of an intracellular enzyme rho-kinase.
Sudden vasoconstriction resulting from any of the aforementioned phenomena leads to decreased coronary blood flow which causes myocardial hypoxia which triggers angina.
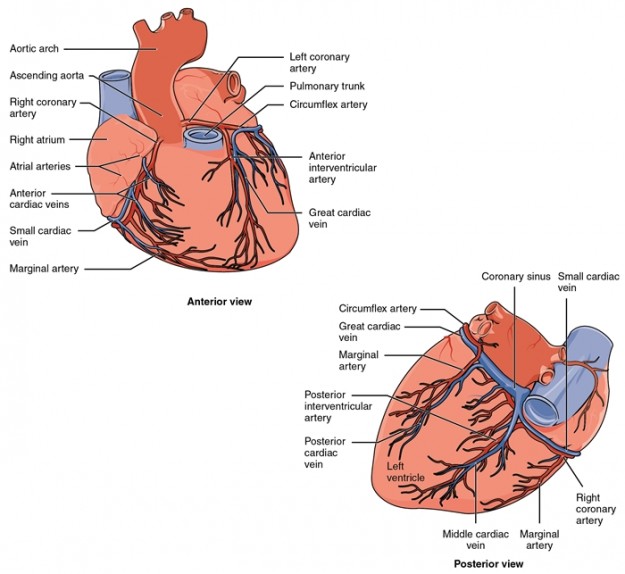
In vasospastic angina, focal coronary artery spasm occurs and significantly reduces the diameter of the coronary artery lumen, causing temporary occlusion and leading to myocardial ischemia. This vasospasm can occur in normal appearing arteries, or arteries affected by atherosclerosis. The most common artery affected is the right coronary artery; the second most commonly affected is the left anterior descending artery.
The exact mechanisms that cause coronary artery spasm are not understood well. Some theories that have been proposed relate to endothelial dysfunction and increased contractility of vascular smooth muscle. With endothelial dysfunction, there is an imbalance between relaxing and contracting factors that are produced by the endothelium.
One important mechanism is related to decreased nitric oxide (NO) production by the dysfunctional endothelium, which is normally made from L-arginine by endothelial NO synthase. As NO has potent smooth muscle relaxation and vasodilator effects, reduced levels can contribute to vasoconstriction. Increased activity of phospholipase C (PLC) has also been reported, which is an enzyme that mobilizes intracellular calcium and may cause smooth muscle contraction.
Another theory is that repeated episodes of coronary vasospasm may cause neointimal hyperplasia, contributing to stenosis in the artery. Rho-kinase is also believed to play a role in the pathogenesis of this condition, involved in regulating vascular smooth muscle contractility.
It is important to note that patients with variant coronary syndrome may have significant atherosclerosis of their coronary arteries. However, the episodes of pain they get are not related to increased oxygen demand (which happens with changes in activity, heart rate or blood pressure).
Other factors that have been suggested that contribute to the pathogenesis of coronary artery spasm include autonomic nervous system dysfunction, magnesium deficiency, chronic low-grade inflammation and increased oxidative stress (with smoking). Genetic factors may be involved, as there is a three-fold greater incidence in Japanese people, compared to Caucasians. It is possible that certain genetic mutations predispose to coronary artery spasm, such as those affecting the endothelial NOS gene.
Clinical Presentation and Diagnosis of Vasospastic Angina
Symptoms of vasospastic angina
Patients experience very severe central chest pain, which is the same type of pain as classic angina. These attacks tend to happen at rest, or during normal activity, but some patients may also experience these attacks during or after exercise, including those who have co-existing fixed coronary artery stenosis.
Patients typically experience attacks of angina in clusters, from midnight to early morning(midnight – 8.00 am). Patients with variant coronary syndrome may also experience asymptomatic ischemic episodes. If coronary artery spasm causes a prolonged disturbance to coronary blood flow, it can cause a myocardial infarction.
Syncope may also occur if there are disturbances to the heart rhythm, such as asystole, atrioventricular block or ventricular tachyarrhythmias. Fatal arrhythmias and sudden cardiac death can also occur.
Symptoms include:
- Chest pain at rest
- Shortness of breath
- Palpitations
Diagnosis of vasospastic angina
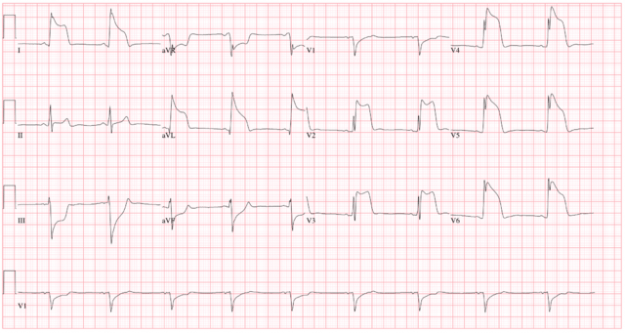
Diagnosis can be confirmed by an ST segment elevation (> 1 mm) on the ECG recorded immediately after or during chest pain. A 24-hour ambulatory ECG recording is done to pick any ECG changes to rule out angina pectoris. Holter monitoring for 24 hours can even pick any silent ischemic episodes occurring during the day.
Image: “ECG of a Patient with Prinzmetal’s Angina” by Gogradgme. License: CC BY-SA 3.0
Electrocardiography is the key to diagnosing vasospastic angina. ECG changes demonstrate transient ST segment elevation during the attack of chest pain, which resolves when the pain settles. ST segment elevation represents transmural myocardial ischemia, and is accompanied by reciprocal ST depressions.
Other changes in the ECG that may be detected include a taller T wave, a taller and wider R wave and loss of the S wave. On occasion, negative U waves may present in the same leads as the ST segment elevation, after the ST elevation starts to resolve. In addition, arrhythmias may be detectable during an episode of variant angina, such as ventricular tachycardia, atrioventricular block and bradyarrhythmia.
If silent episodes of coronary spasm or arrhythmias are suspected, then ambulatory electrocardiographic monitoring with a Holter monitor should be utilized. This is also helpful for recording ECG changes during symptomatic episodes.
Serum cardiac enzymes are typically within normal limits, and coronary artery catheterization often reveals normal coronaries.
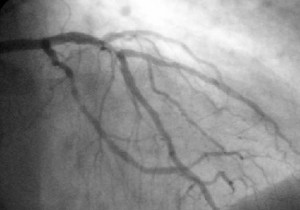
Gold Standard for diagnosis – Induction of Vasospasm during angiography: Intracoronary or intravenous administration of ergonovine or intracoronary infusion of acetylcholine can be used to induce coronary spasm during angiography confirming vasospastic angina.
Intravenous ergonovine test: Non-invasive induction of vasospasm can be achieved by the administration of ergonovine intravenously with 12-lead ECG monitoring. ST segment elevation and induction of angina confirm vasospastic angina.
Exercise testing
Exercise testing with ECG monitoring has variable results. Changes that can be detected in response to exercise include ST elevation, ST depression or no change. ECG changes may point to fixed artery stenosis, coronary artery spasm or no problems.
Coronary angiography
In many cases of variant angina, there is usually an absence of organically stenosed arteries detected on an angiography. However, there are some patients who do have coronary artery stenosis co-existing with coronary artery spasm.
Provocation testing can be used for the definitive diagnosis of coronary variant syndrome. Coronary vasospasm can be provoked during an angiography by injecting acetylcholine and ergonovine into the coronary arteries.
Blood tests
With vasospastic angina, blood tests are generally negative for cardiac enzymes, including troponins and CK-MB.
Major Clinical Complications of Vasospastic Angina
In a few patients, this variant angina may lead to complications, such as severe ventricular tachyarrhythmias or bradyarrhythmias, sinus arrest or even AV block resulting from a severe ischemic episode following vasospasm. Sudden cardiac arrest, with or without syncope, can occur due to ischemia-induced ventricular fibrillation. Atherosclerosis can also occur later at the site of vasospasm leading to local coronary thrombosis.
Differential Diagnosis of Vasospastic Angina
Most common clinical pictures similar to vasospastic angina
- Angina pectoris (stable angina is exercise-induced, demonstrates ST depression and fixed narrowing is usually present).
- Myocardial infarction (vasospastic angina can lead to this if prolonged – an AMI causes prolonged, more severe pain, with positive cardiac enzymes).
- Pulmonary embolism (pain is pleuritic in nature – worse on inspiration, associated with specific risk factors, no ST elevation).
- Pericarditis (pleuritic pain, improved on sitting up and leaning forward).
Other clinical pictures similar to vasospastic angina
- Anxiety Disorders
- Aortic Dissection
- Cocaine Toxicity
- Coronary Artery Atherosclerosis
- Esophageal Motility Disorders
- Esophageal Spasm
- Gastroesophageal Reflux Disease (GERD)
- Isolated Coronary Artery Anomalies
- Panic Disorder
- Unstable Angina
Treatment and Management of Vasospastic Angina
Treatment of vasospastic angina
Patients identified to have variant coronary syndrome should be started on treatment as early as possible. This is very important in order to prevent complications like myocardial infarction, serious arrhythmias and cardiac death. In the acute setting, a nitrate can be administered to relieve an attack of angina. In the long-term setting, patients who smoke are strongly advised tostop smoking.
The main drug used to treat variant coronary syndrome is a calcium channel blocker, such as diltiazem. Calcium channel blockers are very effective in the prevention of ischemia. They may be given alone or given together with isosorbide mononitrate, a long-acting nitrate. Beta blockers are contraindicated as they reduce the dilatation of the smooth musculature through blocking the β2 receptors and would therefore, even further, increase the tone of the coronary vessels.
It has also been suggested that a statin can be given alongside a calcium channel blocker to suppress acetylcholine induced coronary artery spasm. Statins achieve this effect by inhibiting the Rho-associated kinase pathway.
If a patient suffers from arrhythmias secondary to the effects of coronary vasospasm, a pacemaker or automatic defibrillator may need to be implanted.
Medical treatment of vasospastic angina
- Commonly nitrates (isosorbide mononitrate) and calcium channel blockers (Diltiazem) are prescribed to a patient with Prinzmetal angina. Beta-blockers are contraindicated.
- Use of antioxidants like Vitamin C and E directly improve the endothelial function and enhances the effect of vasodilators.
New drugs:
- Nicorandil: A K+-channel agonist can be added in recurrent cases.
- Fasudil is a novel drug which inhibits rho-kinase preventing acetylcholine-induced vasospasm.
Coronary intervention in vasospastic angina
- In refractory cases of variant angina, angioplasty with stenting may improve the condition.
- Complete cardiac denervation with plexectomy, with or without coronary artery bypass surgery, is an option for resistant cases; however, procedural risks are high and results have been inconsistent.
Lifestyle modification
A person should also:
- Eat a healthy balanced diet and exercise regularly
- Quit smoking and limit the use of alcohol
- Report any change in the pattern, or severity of chest pains, to his or her healthcare provider right away.
Regular follow-up investigations include:
- Blood tests
- ECG
Cardiac stress tests or an ECG of the heart’s function during exercise.
Progression and Prognosis of Vasospastic Angina
If the condition is controlled from early on, it can have a favorable prognosis. Complications, such as acute myocardial infarction, coronary artery bypass grafting and cardiac death, typically occur early on after the onset of angina. Patients who have coronary spasm in multiple arteries are prone to having fatal arrhythmias.
Survival rates for vasospastic angina are over 90% at 5 and 10 years. Individuals, who do not have co-existing coronary artery stenosis, generally have a more benign prognosis and better survival, than those who do have severely diseased arteries and coronary artery vasospasm.
Review Questions
The answers are below the references.
1. A young boy of 18 years visits the A&E department with severe chest pain radiating to the back. On the ECG, ST-elevation is seen, but his cardiac enzymes are normal. The anxious parents insisted on coronary artery catheterization which reveals a normal study. What is your most probable diagnosis?
- Stable angina
- Unstable angina
- Ludwig’s angina
- Variant angina
- Vincent’s angina
2. A cardiologist sits with his 53-year-old patient of Prinzmetal angina to answer his queries regarding his medical condition. In response to his question regarding the cause of his chest pain, which of the following would be an appropriate response?
- Vasospasm of coronary vasculature
- Atherosclerotic plaque in coronary arteries
- Small emboli arising from DVT
- Subacute endocarditis
- Factor V Leiden mutation
3. A 56-year-old male, a known case of variant angina, visits the A&E department with an acute episode of chest pain. Which of the following would be the drug of choice for this patient?
- Nitroglycerine patch
- Sublingual nitroglycerine
- Oral nitroglycerine
- Verapamil
- Amlodipine
4. Which of the following therapies do not have a role in treating vasospastic angina?
- Calcium channel blockers
- Nitrates
- Beta blockers
- Rho-kinase inhibitors
5. Which of the following is a predisposing factor to vasospastic angina?
- Hypertension
- Cocaine use
- Increased age
- Hypercholesterolemia
6. What features are most likely to indicate a diagnosis of variant coronary syndrome?
- Cigarette smoker with chest pain during rest, episodic ST elevation, positive cardiac enzymes.
- Hypertensive patient with chest pain on exertion, ST depression, fixed artery stenosis.
- Female patient with chest pain during rest, transient ST elevation, relief with nitrates.
- A Japanese patient with chest pain during normal activity, ST depression, not relieved with nitrates.

Comentários
Enviar um comentário